Journal of
eISSN: 2373-4396


Research Article Volume 16 Issue 1
The Bowling Green Study Center, USA
Correspondence: William E. Feeman Jr, The Bowling Green Study Center, Bowling Green, Ohio, USA, Tel (419) 352-4665
Received: February 12, 2023 | Published: February 23, 2023
Citation: Feeman WE. The population at low risk of atherothrombotic disease. J Cardiol Curr Res. 2023;16(1):12-23. DOI: 10.15406/jccr.2023.16.00572
Background: There are two approaches to the determination of the population at risk of atherothrombotic disease: the herd approach and the targeted approach. In the former scenario, all people are treated, usually with lifestyle changes, but also with medications at times. In the latter scenario, only those deemed at risk of atherothrombotic disease are treated. The author has always favored the latter approach, but for the target approach to be effective, one must know the population at low risk of atherthrombotic disease.
Objectives: The purpose of this manuscript is to demonstrate that the population at low risk of atherothrombotic disease can be readily identified and needless treatment can be avoided.
Methods: The author has conducted a chart review of his family practice patients roster and separated out the cohort of those who developed some form of atherothrombtic disease from the general population cohort.
Results: The author has shown that three major risk factors for atherothrombotic disease can accurately define the population at low risk of atherothrombotic disease: no use of cigarettes, lack of dyslipidemia, and lack of hypertension. Dyslipidemia is defined in terms of the Cholesterol retention Fraction, defined as the difference between low-density lipoprotein cholesterol and high-density lipoprotein cholesterol, that difference divided by the low-density lipoprotein cholesterol, but also whenever low-density lipoprotein cholesterol exceeds 170mg/dl. Hypertension is defined as a systolic blood pressure of 140mmHG or higher or any blood pressure that is being treated. Additionally, the author has shown that in the absence of these three major risk factors, the presence of diabetes mellitus is not associated with early onset atherothrombotic disease.
Conclusions: People who do not manifest the three major risk factors for atherothrombotic disease (cigarette smoking, dyslipidemia, and hypertension)are not at risk of early or middle-age onset atherothrombotic disease. Such people do not require therapy though the high blood sugar levels of uncontrolled diabetes mellitus will require treatment to prevent microvascular disease.
Keywords: atherothrombtic disease, cholesterol retention fraction, lower risk of premature; ramingham heart, total cholesterol study, cholesterol retention fraction
ATD, atherothrombotic disease; FSH, Framingham Heart Study; BSL, blood sugar levels; BGS, Bowling Green Study; CT, total cholesterol; TG, triglycerides; CRF, cholesterol retention fraction; SBP, systolic blood pressure
There are two major approaches to the prevention of atherothrombotic disease (ATD, which is atherosclerotic disease with emphasis on the thrombosis, which is so often the presenting sign of clinical atherosclerosis, such as heart attack, stroke, etc): the herd approach and the targeted approach. In the herd approach, everyone is put on therapy (usually diet, but in some cases medication) regardless of ATD risk. In the targeted approach, only those deemed to be at risk of ATD receive therapy. The author prefers the targeted approach. The Framingham Heart Study (FHS) has published its research into those factors that are associated with ATD.1-8 and the author has used those “factors of risk” (now called risk factors) to extend the FHS findings. The major ATD risk factors are cigarette smoking, dyslipidemia, and hypertension, with some contribution by the very high blood sugar levels (BSL) of uncontrolled diabetes.9-11 These publications have focused on those individuals who are at higher risk of ATD. There is a population that is at lower risk of premature ATD12 and the author now presents the findings of his own study: the Bowling Green Study (BGS) of Primary and Secondary Prevention of Atherothrombotic Disease, as it relates to the population at low risk of ATD. This study will be referred to simply as the BGS for the purposes of this paper.
The Bowling Green Study was begun on 4 November 1974 and terminated on 1 January 2019, when the author left his service in the United states Air Force and established his practice of family medicine in Bowling Green, the county seat of Wood County, in northwest Ohio. Bowling Green is a small city of 30,808 people at last census (2020) and the Wood County population in 2020 was 132,248. It is the home of Bowling Green State University, which is the chief employer in the area. Though the county is mainly agricultural, there are numbers of small industries that offer employment. The populace of the county is mainly of European origin, with Latin Americans being the chief minority. People of Asian and African extraction are increasing in numbers in the county. The author, as a family physician, accepted into his practice people of all ages (from newborns to people in their ninth and tenth decades of life) and both genders. This population became the foundation of the BGS. The foundation of the BGS has been described on a number of occasions in the literature.9,10,13,14
The author’s aim at initiating the BGS was to find a way to more accurately predict the population at risk of ATD. To do this, the author knew that he would need a data base of ATD risk factors. Following the example of the FHS, the author began collecting blood pressure, height, and weight data on everyone who entered his practice. The height and weight data were later integrated as the body mass index. Moreover, when the fundamental role of cigarette smoking became obvious in 1983, he began asking all members of his practice (initially those aged 15years or older but then, in the 1990’s, all those aged 10years or older) about cigarette smoking habits. Additionally, he began to collect lipid and glucose data whenever the opportunity arose. This data consisted of fasting lipids, which consisted of total cholesterol (CT) and triglycerides (TG) until 1 January 1978, when high-density lipoprotein cholesterol (HDL-c) was offered by the local hospital laboratory, and with it the opportunity to calculate low-density lipoprotein cholesterol (LDL-c) via the Friedewald formula: LDL-c =CT minus HDL-c minus TG/5.15 All of these measurements were then placed in a general population database, ranked by age at which the testing was done.
Prevention of ATD was a new concept to people in Bowling Green in the early years of the BGS (1974 and thereafter to the late 1980’s) and their physicians were not interested either. Additionally FHS guidelines at the time were fairly vague and anti-dyslipidemic medications were not very effective. As a result, many people declined the author’s invitation to begin therapy of ATD risk factors—especially dyslipidemia. Subsequently, a large number of the author’s patients developed some form of ATD. By 1981, enough patients had sustained ATD events, such that the author was able to separate out a database for ATD patients from the general population database.
Inspection of the ATD database revealed that ATD risk factors rarely were present individually—virtually all of the time, they were present in combination with other ATD risk factors. While the other ATD risk factors appeared to be relatively straight forward, the lipid risk factors were not. The tabulated risk factors were examined initially as independent risk factors. However, some people had ATD events in the face high LDL-c levels, as expected—but then some people had ATD events in the face of low LDL-c levels. Conversely, some people had ATD events in the face of low HDL-c levels, as expected—but then some people had ATD events in the face of high HDL-c.
In 1981 an article appeared in a medical journal (unfortunately lost to the author, so that the author is unable to give proper attribution), an article entitled “Is the LDL: HDL Ratio the Best Lipid Predictor?” In light of this article the author re-examined his ATD database. Those ATD patients who had low LDL-c levels also had very low HDL-c levels and those ATD patients with high HDL-c levels also had very high LDL-c levels. When these relationships did not hold, the younger patients were cigarette smokers, current or past, and the older patients had hypertension, with or without diabetes.
In 1983, it occurred to the author that what he really wanted to know was the amount of cholesterol accumulating within the arterial wall. This, he reasoned, could be best estimated by subtracting the amount of cholesterol exiting the arterial wall via reverse cholesterol transport (HD-c) from the amount of cholesterol entering the artery wall (LDL-c) and then expressing the difference as a percentage of the cholesterol entering the arterial wall (LDL-c). This ratio was termed the Cholesterol Retention Fraction (CRF): (LDL-C minus HDL-c)/LDL-c. This ratio is abnormal at 0.70 and higher. However, when LDL-c is very high, the reverse cholesterol mechanism (as represented by HDL-c) is overwhelmed. This scenario occurs when LDL-c is 170 mg/dl or higher. Thus a state of dyslipidemia occurs whenever the CRF is 0.70 or higher, or whenever LDL-c is 170 mg/dl or higher—and is termed the Cholesterol Threshold (CThr).
As noted previously, inspection of the ATD database revealed that the various ATD risk factors rarely operated in a vacuum, but rather were most often present in a milieu. The author therefore examined various risk factor combinations to determine which combinations were predictive. Only the ratio between LDL-c and HDL-c (in 1981, but the CRF in 1983 and thereafter because the CRF predicted the population at risk of ATD 5% better than did the LDL-c : HDL-c ratio [Feeman, unpublished data]) and systolic blood pressure (SBP) was predictive—and then only when stratified by cigarette smoking status. By 1988, enough people had developed ATD events, the author was able to formulate a threshold line, above which lay the vast majority of the ATD patients’ CRF-SBP plots and below which lay the CRF-SBP plots of a relative few outliers (Figure 1). In 2000, the author published an article in which he plotted the CRF-SBP plots of all patients in eight published angiographic regression studies.16 These were all secondary prevention trial and one of them (Lipoprotein and Coronary Atherosclerosis Study) had an average of end-of-trial CRF-SBP plots, associate with plaque progression, that lay just below the threshold line. It then occurred to the author that many people who presented to the BGS may have had subclinical atherosclerosis, so he lowered the threshold line to its present location, with CRF-SBP loci at (0.74,100) and (0.49.140). This predictive tool is termed the BGS graph. The BGS graph can be stratified by cigarette smoking status. “Current cigarette smoking” means that the patients were smoking cigarettes at the time of their presentation to the BGS. “Past smoking” means that the patients had been cigarette free for at least six months prior to their presentation to the BGS. “Other tobacco” means that the patients were smoking pipes or cigars or were chewing tobacco at the time of their presentation to the BGS—but had never smoked cigarettes. “Never smoking” means that the patients had never smoked cigarettes and if they had used other tobacco products, then they had not done so within six months of presenting to the BGS.
The BGS has used the two hour postprandial Blood Sugar Level (2hr pp BSL) as its measure of glucose tolerance since the inception of the study. Instead of using Glucola, the author opted to utilize a standard 100 gm carbohydrate breakfast, as calculated by the Wood County Hospital dietician. The reason underlying this course of action was that this test would measure the glucose response to actual food and thus represent a real world response. Such a breakfast consists of a glass of orange juice, a bowl of cereal with milk and sugar, and three pieces of toast with butter and jelly. The breakfast was to ingested within a 15 minute timeframe and a blood sugar level determined exactly two hours after finishing breakfast. (A copy of the protocol is placed in the appendix and has been the BGS standard of measuring glucose tolerance since 1974.) Diabetes is diagnosed when a 2hr pp BSL of 200mg/dl or higher is found; impaired glucose tolerance, when the 2hr pp BSL of 125-199 mg/dl is found; high normal glucose tolerance is diagnosed when the 2hr pp BSL is 100-124mg/dl is found; and normal glucose tolerance is diagnosed when the 2hr pp BSL is 99mg/dl or lower.
Caveat
The measurement of HDL-c has changed over time, from the classic precipitation method to the newer enzymatic method. In the BGS, this change in HDL-c measurement methodology occurred in May, 1999. These differing methodologies do not give the same results: indeed, the HDL-c levels derived from the enzymatic method results in an HDL-c level on the order of 10mg/dl higher than that derived from the precipitation method.17 Since LDL-c is usually not measured but rather calculated by the Fried Ewald formula, this higher HDL-c results in a drop in LDL-c levels by the same amount. This difference is not trivial. The author has reported the case of a patient who sustained an acute myocardial infarction without any apparent ATD risk factors—albeit his lipids had never been measured. The auto-analyzer that measured his lipid at the time of his myocardial infarction utilized the enzymatic methodology of HDL-c measurement and his CRF calculate on these values was slightly abnormal, but more marked abnormal when the enzymatic determination of HDL-c was converted to its precipitation-determined equivalent.17 It is important to take this difference into account because the eight angiographic regression studies used by the author to validate the CRF and CThr all utilized the precipitation method of HDL-c determination. The author’s data and the data from the studies he cites are all based on the precipitation method of HDL-c measurement or the conversion of the enzymatic HDL-c value into its precipitation method equivalent by the formula:
HDL-c (precipitation method)= (HDL-c [enzymatic method] -12)/0.93
Which is valid at the author’s local hospital lab. The author has made adjustments to the BGS graph to accommodate this change and presents them in Figure II. However, all data presented in this paper are based on the precipitation methodology.
The area above the threshold line in Figure 1 is expansive and covers a wide range of CRF-SBP plots (Figure 2 will not be considered for the reasons noted above.). It is useful to subdivide the areas above and below the threshold line into smaller areas such that similar CRF-SBP plots are considered together. If one determines a vertical line at the SBP level of 140 mm Hg, one can separate hypertensive patients from normotensive patients. (In this case, patients with treated hypertension on BGS presentation have their CRF-SBP plots placed to the right of the vertical line.) If one also determines a horizontal line at the CRF level of 0.70, then one can separate the eulipidemia patients (below the line) from the dyslipidemic patients (above the line). (Again, patients with LDL-c levels of 170mg/dl or higher, regardless of CRF value, will also be placed with the patients having a CRF of 0.70 or higher.) Such divisions create seven zones on the BGS graph (Figure 3). Zone I-A encompasses all patients with CRF-based dyslipidemia, but no hypertension, with CRF-SBP plots above the threshold line, whereas Zone I-B encompasses a similar group of patients, but whoser CRF-SBP plots lie below the threshold line. Zone II encompasses those patients who have dyslipidemic hypertension, as defined previously. Zone III encompasses those patients with hypertension (treated or untreated), but no CRF-based dyslipidemia. Zone III-A patients having their CRF-SBP plots above the threshold line and Zone III-B patients having their CRF-SBP plots below the threshold line. Zone IV patients have neither CRF-based dyslipidemia nor hypertension (treated or untreated), and again Zone IV-A patients have CRF-SBP plot above the threshold line while Zone IV-B patients have CRF-SBP plots below the threshold line (Figure 3).
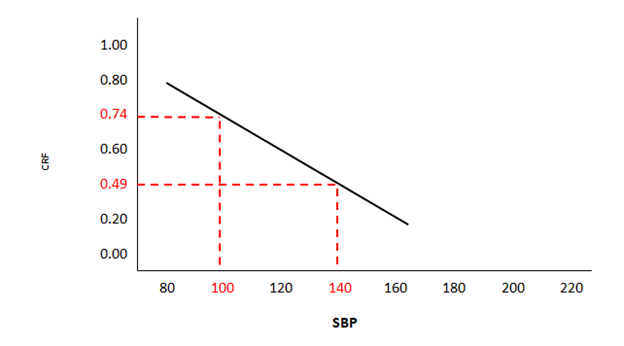
Figure 1 Precipitation Method of HDL Cholesterol Measurement
CRF means Cholesterol Retention Fraction, SBP Means Systolic Blood Pressure, HDL means High Density Lipoprotein.
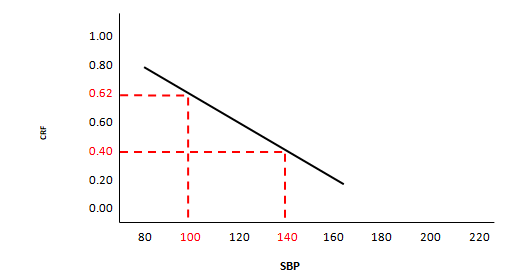
Figure 2 Enzymatic Method of HDL Cholesterol Measurement
CRF means Cholesterol Retention Fraction, SBP Means Systolic Blood Pressure, HDL means High Density Lipoprotein.
Table 1 shows the average of ATD onset with respect to the threshold line. Table 2A shows the average age of ATD onset, in the male ATD population, with respect to the various zones defined in Figure III. Table 2B show similar results for the female ATD population. All tables are stratified by cigarette smoking status. It will be clear that current cigarette smoking is associated with the youngest average age of ATD onset, whereas never smoking status, even if associated with other tobacco use, was associated with the oldest average age of ATD onset. Inspection of Table 2A & 2B also reveals that there are many more cigarette smokers, current or past, in the male ATD population than in the female ATD population. The interpretation of past smoking is more difficult, since the BGS is made up of a large number of people who had had their ATD events prior to their presentation to the BGS, and hence were placed in the “History” category.10 Such patients could have smoked cigarettes at the time of their earlier ATD events, but even so, there is still a clear cut increase in the average age of ATD onset in males and females when current cigarette smoking is compared to past smoking. A similar increase in the average age of ATD onset is seen in females when comparing past smoking with never smoking (cigarettes) but in males, when past smoking is compared to never smoking cigarettes, the increase is seen essentially only in Zones IV-A and IV-B.
Sex |
Average Age of ATD Onset with Respect to Threshold Line |
+ |
Past |
OT |
NT |
? |
∑ |
Male |
Above Threshold Line |
160 |
149 |
21 |
88 |
-- |
418 |
|
Below Threshold Line |
25 |
23 |
1 |
12 |
1 |
62 |
|
∑ |
185 |
172 |
22 |
100 |
1 |
480 |
Female |
Above Threshold Line |
86 |
62 |
-- |
155 |
-- |
303 |
|
Below Threshold Line |
24 |
18 |
-- |
46 |
-- |
88 |
|
∑ |
110 |
80 |
-- |
201 |
-- |
391 |
Table 1 Population at Low Risk of ATD
ATD Means Atherothrombotic Disease, + Means Current Smoker, Past Means Past Smoker, OT Means Use of Other Tobacco Products, NT Means No History of Any Tobacco Products, ? Means Cigarette Status Unknown
Cigarettes |
IA |
IB |
II |
IIIA |
IIIB |
IVA |
IVB |
+ |
62 |
1 |
56 |
24 |
4 |
18 |
20 |
Past |
41 |
|
64 |
30 |
12 |
14 |
11 |
OT |
7 |
|
6 |
7 |
1 |
1 |
|
NT |
32 |
2 |
35 |
14 |
2 |
7 |
8 |
? |
|
|
|
|
|
|
1 |
|
|
|
|
|
|
|
|
∑ |
142 |
3 |
161 |
75 |
19 |
40 |
40 |
|
|
|
|
|
|
|
|
Table 2A Zonal Distribution in ∑ Male ATD Pop w/r Cigarettes Ave Age of ATD Onset Zone
ATD Means Atherothrombotic Disease, + Means Current Smoker, Past Means Past Smoker, OT Means Use of Other Tobacco Products, NT Means No History of Any Tobacco Products, ? Means Cigarette Status Unknown
Cigarettes |
IA |
IB |
II |
IIIA |
IIIB |
IVA |
IVB |
+ |
36 |
1 |
25 |
14 |
6 |
11 |
17 |
Past |
15 |
1 |
25 |
19 |
5 |
3 |
12 |
OT |
|
|
|
|
|
|
|
NT |
27 |
1 |
67 |
49 |
15 |
12 |
30 |
? |
|
|
|
|
|
|
|
∑ |
78 |
3 |
117 |
82 |
26 |
26 |
59 |
|
|
|
|
|
|
|
|
Table 2B Zonal Distribution in ∑ Female ATD Pop w/r Cigarettes Ave Age of ATD Onset Zone
ATD Means Atherothrombotic Disease, + Means Current Smoker, Past Means Past Smoker, OT Means Use of Other Tobacco Products, NT Means No History of Any Tobacco Products, ? Means Cigarette Status Unknown
Table 3A shows the prevalence of the various zones in the general population versus the ATD population for males, while Table III-B shows the same distributions for females. For males, the prevalence of Zone II is much higher in the ATD population than it is in the general population, and Zone III-A is moderately higher in the ATD population than it is in the general population, whereas in the female ATD population Zones II and III-A are both much higher than in the general population. Conversely, Zone IV-B is much more common in the general population than in the ATD population.
|
General Population |
ATD Population |
||
Zone |
Zone incidence |
% ATD |
Zone Incidence |
Average Age of ATD Onset |
IA |
504 |
121 |
142 |
142 |
IB |
15 |
4 |
3 |
3 |
II |
290 |
123 |
161 |
161 |
IIIA |
168 |
59 |
75 |
75 |
IIIB |
31 |
14 |
19 |
19 |
IVA |
227 |
31 |
40 |
40 |
IVB |
400 |
34 |
40 |
40 |
Table 3A CRF-SBP Zones ∑ Males
CRF Means Cholesterol Retention Fraction, SBP Means Systolic Blood Pressure, ATD Means Atherothrombotic Disease
Further inspection of Table 3A reveals that while the prevalence of isolated dyslipidemia in the general male population is 32% (519/1635), it is 30% (145/480) in the ATD population. Moreover, the prevalence of dyslipidemic hypertension in the general male population is 18% (290/1635) and 34% (161/489) in the ATD population. Further, isolated hypertension occurs in 12% (199/1635) of the male general population and in 20% (94/480) in the ATD population. Neither dyslipidemia nor hypertension were found in38% (627/1635) of the male general population and 17% (80/480) of the ATD population.
Further inspection of Table 3B reveals that the female general population has a prevalence of isolated dyslipidemia of 21% (346/1628), compared to 21% (81/391) in the ATD population. Further, the prevalence of dyslipidemic hypertension in the female general population is 10% (170/1628) while it is 30% (17/391) in the ATD population. Moreover the prevalence of isolated hypertension in the female general population is 11% (183/1628) while it is 28% (108/391) in the ATD population. Finally, 57% (929/1628) of the female general population and 22% (85/391) of the female ATD population have neither dyslipidemia nor hypertension.
|
General Population |
ATD Population |
||
Zone |
Zone incidence |
% ATD |
Zone Incidence |
Average Age of ATD Onset |
IA |
316 |
83 |
78 |
78 |
IB |
30 |
7 |
3 |
3 |
II |
170 |
75 |
117 |
117 |
IIIA |
123 |
54 |
82 |
82 |
IIIB |
60 |
25 |
26 |
26 |
IVA |
181 |
26 |
26 |
26 |
IVB |
748 |
56 |
59 |
59 |
Table 3B CRF-SBP Zones ∑ Females
CRF Means Cholesterol Retention Fraction, SBP Means Systolic Blood Pressure, ATD Means Atherothrombotic Disease
So far this analysis has not focused on diabetic patients. Ever since the publication of the East-West Trial, diabetes has been termed an ATD “equivalent.”18 If this is true then, diabetic patients ought to be spread through out the various zones and diabetes ought to produce ATD events in the low risk zones—i.e., Zones IV-A and IV-B. That is to say, diabetes should induce ATD events in the absence of other ATD risk factors. For purpose of this analysis, the author will use two hour postprandial blood sugar levels (2 hr pp BSL) to define glucose tolerance. The author defines diabetes as a 2hr pp BSL of 200mg/dl or higher. Impaired glucose tolerance is defined as a 2hr pp BSL of 125-199mg/dl. Euglycemia is defined as a 2hr pp BSL of 124 mg/dl or less. Euglycemia can be sub-divided into high euglycemia (2hr pp BSL of 100-124mg/dl) and ideal euglycemia (2hr pp BSL of 99mg/dl or less). 2hr pp BSL levels are available for 348 male ATD patients and 303 female ATD patients, for a grand total of 651 ATD patients. All values of the 2hr pp BSL are determined precisely 2 hours after a standard 100 gm carbohydrate breakfast, as defined by the Wood County Hospital dietician in 1974. (The protocol can be found in the appendix.) Table IV shows the distribution of the 2hr pp BSL in the male and female General Population as well as the ATD population. In both males and females the distribution of 2hr pp BSL values are shifted to higher levels in the ATD population than in the general population, perhaps more so in females than in males. Tables 5A & 5B give the 2hr pp BSL distributions in the various BGS graph zones, for males and females respectively, and demonstrate that in diabetic male ATD patients only 12% do not have associated dyslipidemia or hypertension whereas in diabetic female ATD patients only 14% do not have associated dyslipidemia or hypertension. Zone II has the highest prevalence of diabetics. Tables 6A & 6B give the average ages of ATD onset in the various Zones. Diabetics whose CThr-SBP plots lie in Zones IV-A and IV-B have the oldest average age of ATD onset, though in females Zone III-A has a similar average age of ATD onset. Table VII reveals that there were no diabetics whose CThr-SBP plots, in the male ATD population, were located in the never-smoker cohort of the low ATD risk zones (Zones IV-A and IV-B), whereas in the comparative female ATD population, only four patients, with an average age Of ATD onset of 75 years. As regards impaired glucose tolerance (2hr pp BSL of 125-199mg/dl), again there were no male ATD patients whose CThr-SB P plots were located in the never-smoking cohort of the low risk zones (Zones IV-A and IV-B) and only three female ATD patient in the comparative category, with an average age of ATD onset of 59years. (Table VIII)
|
Male |
Female |
||||
2 hr pp BSL |
Gen Pop |
ATD Pop |
Gen Pop |
ATD Pop |
Gen Pop |
ATD Pop |
< 99 |
910 |
115 |
976 |
99 |
1856 |
214 |
100-124 |
433 |
105 |
462 |
91 |
895 |
196 |
125-149 |
135 |
42 |
135 |
39 |
270 |
81 |
150-174 |
48 |
22 |
54 |
17 |
102 |
39 |
175-199 |
25 |
13 |
11 |
7 |
36 |
20 |
> 200 |
134 |
52 |
124 |
50 |
258 |
102 |
∑ |
1685 |
349 |
1762 |
303 |
3447 |
652 |
Table 4 2 hr pp BSL Distribution, In ∑ ATD Population vs General Population ∑∑ Cigarettes
PP Means Postprandial Glucose Levels, BSL Means Blood Sugar Levels, ATD Means Atherothrombotic Disease
Zone |
< 99 |
100-124 |
125-149 |
150-174 |
175-199 |
> 200 |
∑ |
IA |
46 |
28 |
12 |
6 |
2 |
9 |
103 |
IB |
1 |
|
|
|
|
|
1 |
II |
32 |
40 |
18 |
6 |
7 |
25 |
128 |
IIIA |
15 |
20 |
6 |
6 |
2 |
9 |
58 |
IIIB |
2 |
2 |
1 |
1 |
1 |
3 |
10 |
IVA |
14 |
8 |
3 |
3 |
1 |
1 |
30 |
IVB |
5 |
7 |
2 |
|
|
5 |
19 |
∑ |
115 |
105 |
42 |
22 |
13 |
52 |
349 |
|
|
|
|
|
|
|
|
Table 5A 2 hr pp BSL Distribution In ∑ Male ATD Population
PP Means Postprandial Glucose Levels, BSL Means Blood Sugar Levels, ATD Means Atherothrombotic Disease
Zone |
< 99 |
100-124 |
125-149 |
150-174 |
175-199 |
> 200 |
∑ |
IA |
34 |
17 |
4 |
2 |
|
7 |
64 |
IB |
2 |
1 |
|
|
|
|
3 |
II |
20 |
28 |
13 |
9 |
3 |
21 |
94 |
IIIA |
11 |
21 |
10 |
3 |
4 |
14 |
63 |
IIIB |
4 |
4 |
5 |
|
|
1 |
14 |
IVA |
10 |
6 |
2 |
|
|
5 |
23 |
IVB |
18 |
14 |
5 |
3 |
|
2 |
42 |
∑ |
99 |
91 |
39 |
17 |
7 |
50 |
303 |
Table 5B 2 hr pp BSL Distribution In ∑ Female ATD Population
PP Means Postprandial Glucose Levels, BSL Means Blood Sugar Levels, ATD Means Atherothrombotic Disease
Zone |
< 99 |
100-124 |
125-149 |
150-174 |
175-199 |
> 200 |
IA |
46 |
28 |
12 |
6 |
2 |
9 |
IB |
1 |
|
|
|
|
|
II |
32 |
40 |
18 |
6 |
7 |
25 |
IIIA |
15 |
20 |
6 |
6 |
2 |
9 |
IIIB |
2 |
2 |
1 |
1 |
1 |
3 |
IVA |
14 |
8 |
3 |
3 |
1 |
1 |
IVB |
5 |
7 |
2 |
|
|
5 |
Table 6A 2 hr pp BSL Zonal Distribution Ave Age of ATD Onset: ∑∑ Cigarettes Male 2 hr pp BSL
PP Means Postprandial Glucose Levels, BSL Means Blood Sugar Levels, ATD Means Atherothrombotic Disease
Zone |
< 99 |
100-124 |
125-149 |
150-174 |
175-199 |
> 200 |
IA |
34 |
17 |
4 |
2 |
|
7 |
IB |
2 |
1 |
|
|
|
|
II |
20 |
28 |
13 |
9 |
3 |
21 |
IIIA |
11 |
21 |
10 |
3 |
4 |
14 |
IIIB |
4 |
4 |
5 |
|
|
1 |
IVA |
10 |
6 |
2 |
|
|
5 |
IVB |
18 |
14 |
5 |
3 |
|
2 |
Table 6B 2 hr pp BSL Zonal Distribution Ave Age of ATD Onset: ∑∑ Cigarettes Female 2 hr pp BLS
PP Means Postprandial Glucose Levels, BSL Means Blood Sugar Levels, ATD Means Atherothrombotic Disease
|
Male |
Female |
|
|
||
Cigarettes |
IV-A |
IV-B |
IV-A |
IV-B |
IV-A |
IV-B |
+ |
|
1 |
1 |
|
1 |
1 |
Past |
1 |
3 |
1 |
1 |
2 |
4 |
OT |
|
|
|
|
|
|
NT |
|
|
3 |
1 |
3 |
1 |
? |
|
|
|
|
|
|
|
1 |
4 |
5 |
2 |
6 |
6 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Table 7 Cigarettes vs 2 hr pp BSL In Zone IV-A & IV-B Average Age of ATD Onset in ∑ ATD w/r Cigarettes 2 hr pp BSL 125-199
PP Means Postprandial Glucose Levels, BSL Means Blood Sugar Levels, ATD Means Atherothrombotic Disease, + Means Cigarette Smoker, Past Means History of Cigarette Smoking, OT Means Use of Other Forms of Tobacco, NT Means Never Used Tobacco, ? Means Unknown Use of Tobacco
Zones |
||||||
|
Male |
|
Female |
|||
Cigarettes |
IV-A |
IV-B |
IV-A |
IV-B |
IV-A |
IV-B |
+ |
|
3 |
1 |
3 |
1 |
6 |
Past |
5 |
3 |
1 |
2 |
6 |
5 |
OT |
|
|
|
|
|
|
NT |
|
|
|
3 |
|
3 |
? |
|
|
|
|
|
|
|
5 |
6 |
2 |
8 |
7 |
14 |
|
|
|
|
|
|
|
Table 8 Cigarettes vs 2 hr pp BSL In Zone IV-A & IV-B Average Age of ATD Onset in ∑ ATD w/r Cigarettes 2 hr pp BSL 125-199
PP Means Postprandial Glucose Levels, BSL Means Blood Sugar Levels, ATD Means Atherothrombotic Disease, + Means Cigarette Smoker, Past Means History of Cigarette Smoking, OT Means Use of Other Forms of Tobacco, NT Means Never Used Tobacco, ? Means Unknown Use of Tobacco
The individual ATD risk factors are, in order: cigarette smoking, dyslipidemia (as described by the CRF and CThr), and hypertension, with some contribution by the very high blood sugar levels of uncontrolled diabetes, as measured by the 2 hr pp BSL.11 The population at risk of ATD can be accurately defined by combining the first three of these factors.9 This is done by graphing the CRF versus the systolic blood pressure (SBP) and stratifying the resultant graph by cigarette smoking status (Figures 1 & 2). Table 1 reveals the average age of ATD onset with respect to the threshold line on the BGS graph. Current cigarette smoking is associated with an early age of ATD onset, whereas a past smoking history (having quit smoking cigarettes and not re-starting smoking) is associated with an older average age of ATD onset; use of non-cigarette tobacco products (but no history of cigarette smoking; cigarette smokers who quit cigarettes and switched to non-cigarette tobacco use are considered past smokers), with a late average age of ATD onset; and never smokers (excluding use of non-cigarette tobacco products), with a late average age of ATD onset in males and an even later age of ATD onset in females. The most common ATD category in the BGS is a history of an ATD event, comprising almost 50% of cases.10 Thus, patients with such histories could have been smoking at time to their clinical ATD event and could have quit at that time, thus presenting to the BGS years later in the “History” category as past smokers. Similarly, patients who themselves never used tobacco products could have had spouses who smoked cigarettes and thus been exposed to passive smoking. The role of passive cigarette smoking was unappreciated at the inception of the BGS and in its early years, and while such data is known for some ATD patients, it is not included as a category in this report. The great majority of such patients were women, but men were not rare.
Evaluation of Tables 2A and 2B reveals that the CRF-SBP plots of 66% of male ATD patients and 53% of female ATD patients are located in Zones I-A, I-B, and II and thus have CRF-based dyslipidemia. Similarly 51% of male ATD patients and 55% of female patients have CRF-SBP plots located in Zones II, III-B, and III-A, and thus have hypertension (treated or untreated). 66% of males with hypertension have associated dyslipidemia, whereas 55% of females have dyslipidemic hypertension. The average age of ATD onset in isolated dyslipidemia in ATD males is 58 years, and in dyslipidemic hypertensive males, is 62years whereas in isolated hypertension is 67years. Corresponding figures for women are 61, 69years of age and 74years of age. This indicates the prime importance, after cigarette smoking, of dyslipidemia in the prediction of the population at risk of ATD.
Those ATD patients with neither CRF-based dyslipidemia nor hypertension (treated or untreated) have CRF-SBP plots in Zones IV-A or IV-B. In theory, ATD patients in Zones IV-A and IV-B should have the lowest ATD risk and the oldest age of ATD onset—if they are never smokers. Current male smokers in these low-risk zones have an average age of ATD onset of 55years; past smokers, 69years; while those who have never smoked cigarettes have an average age of ATD onset of 75years. Corresponding ages for female ATD patients are 60, 68, and 71years.
Tables 3A and 3B show the distributions, for males and females respectively, of the various zones in the ATD population and the general population. For males, the greatest differences in distributions between the ATD population and the general population are in Zone II, where there are many more patients in the ATD population than in the general population and in Zone IV-B where there are many more people in the general population than in the ATD population. These findings are mimicked in the female ATD population versus the general population.
Table 3A further reveals that 64% of males in the ATD population have CRF-based dyslipidemia, whereas on 50% of males in the general population are dyslipidemic. Similarly 51% of ATD females have CRF-based dyalipidemia, whereas only 31% of general population females are dyslipidemic (Table 3B). Hypertension (treated or untreated) is present in 54% of ATD males, but only 30% general population males. The corresponding numbers for females are 58% for ATD females and 22% for general population females. This leaves 38% of general population males in Zones IV-A and IV-B, but only 16% in the ATD population. The corresponding numbers for females are 57% (general population) and 22% (ATD population).
Tables 5A and 5B demonstrate the average ages of ATD onset for male and female ATD patients respectively. In this analysis, however, one can include ATD patients who had their events prior to BGS presentation and who were placed on anti-dyslipidemic medications: 30 male and 14 female patients. The medications were mainly statins. Making the assumption that these ATD patients actually did have dyslipidemia, one could add these patients to the ATD database in terms of Zones I-, I-B, and II, depending upon their blood pressure status. Doing this swells the number of patients in the male cohort to 510 and the female cohort to 405 patients , for a grand total of 915 patients, increasing the numbers of patients in Zones I-A and II. (There were no I-B Zone patients in this addition.) However there were no effects upon the average age of ATD onset.
Table VII reveals the average age of ATD onset for males and females respectively, in whom the 2hr pp BSL are known. As stated previously, if the 2hr pp BSL is an ATD equivalent, then it ought to cause ATD events in the low risk patients (in Zones IV-A and IV-B and no history of cigarette smoking). Table 7 reveals that there were no diabetic patients in the never-smoker cohort of the low risk zones in ATD males. Table 7 also reveals that in the low risk zone, there were three females in Zone IV-A (average age of ATD onset was 69 years) and one female in Zone IV-B (aged 90 years at ATD onset).
With respect to impaired glucose intolerance, Table 8 reveals that there were no males in Zone 4A or IV-B. Likewise Table 8 also reveals that there were no female patients in Zone 4A and three females in Zone IV-B with an average age of ATD onset of 59years).
Females are more difficult to interpret since many of their ATD risk factors are not unmasked until the peri-menopausal portion of their lives.19–21 This may well explain the older ages in females in the never smoking cohort of the various zones of the BGS graph. Moreover, the graph in Figure I does not allow for CThr and hence women with LDL-c of 170mg/dl or higher will be positioned below the threshold line. This problem is eliminated by the use of Zones. Furthermore, there are many more cigarette smokers, current or past, in the male ATD population than in the female ATD population, and this too explains the older age of ATD onset in females with respect to males (Tables 1,2A and 2B.) Additionally, some females in Zone 4B have confounding factors, chief among which is the problem of second-hand smoking. Many women in the BGS, especially in the early years, did not smoke cigarettes, but their husbands did. When the BGS began, the role of cigarette smoking in ATD was not properly appreciated—and the role of passive smoking in women was never even considered. Hence the BGS has no formal data of second hand smoking. (A few BGS males also suffered from passive smoking.) Other factors that confound BGS females include multiple sclerosis therapy and chest radiation of lymphoma, which were not seen in males in this study. Finally, microvascular ATD was included in the BGS ATD categories, such as microvascular angina, were included in this analysis, and such women may not have dyslipidemia.
The author, given the preceding discussion, feels that people whose CThr-SBP plots lie within the low risk zones (IV-A and IV-B) do not require either dyslipidemic or hypertensive therapy. In the author’s experience and in the experience of others (Lale Tokgozoglu, MD, personal communication, 28 May 2019) there is no combination of the major three risk factors described in this paper that results in no ATD risk. Moreover, the author has discussed the level of ATD risk that warrants therapy with several well-known experts (who spoke on the condition of anonymity) and the opinion was that a 15% risk should warrant therapy for blood lipid levels. In the BGS, this risk level is not attained until the ninth decade of life when only a CRF of 0.59 or lower is considered. Therefore, in the author’s opinion, the goal of preventive cardiology should be to treat those people whose CThr-SBP plots lie in the higher risk zones and not to treat those whose CThr-SBP plots imply immunity to clinical ATD until very late in life.
Finally, the author has shown that, in eight published angiographic regression studies, any therapy that brings the CRF-SBP plot below the threshold line in Figure I results in plaque non-progression in 75% of cases provided that the SBP is kept below 140mm Hg.16 Moreover, in these same studies, achievement of either a target goal of CRF of 0.59 or lower or LDL-c of 99mg/dl or lower is associated with minimal plaque progression.22 In the 1990’s, when these studies were done, the concept of CThr was not appreciated, but in any event, when the CRF is 0.59 or lower, the CThr-SBP plot should lie in Zones IV-A or IV-B. This point is made to support the therapy of dyslipidemia and/or hypertension to ameliorate the risk of ATD. The author has also shown that a CRF of 0.59 or lower is associated with such a low risk of ATD, in both males and females, that it might not need therapy at all, even if CThr is present.10 For those at higher ATD risk, the treatment that is mostly likely to achieve the goal of achieving a CThr-SBP plot position in the low risk zones (Zone IV-A and IV-B) is one that simultaneously lowers LDL-c and raises HDL-c.23,24
Zones IV-A and IV-B , in the general population, are much more common than in the ATD population. A CThr-SBP plot that lies within Zones IV-A and IV-B in the ATD population is associated with ATD events that are late in life in never-smokers. Cigarette smoking destroys any such benefit. It is recommended that patients whose CThr-SBP plots are outside the low risk Zones have therapy to attain the low risk zones, and that patients be strongly counseled to stop smoking.
None.
The authors declare no conflict of interest.
None.

©2023 Feeman. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.