Journal of
eISSN: 2373-4396


Mini Review Volume 12 Issue 1
Department of Cardiology, Faculty of Medicine, Marmara University, Turkey
Correspondence: Batur Gonenc Kanar, Department of Cardiology, Faculty of Medicine, Marmara University, Turkey, Tel +905395855150, Fax +902166570695
Received: December 11, 2018 | Published: January 4, 2019
Citation: Kanar BG. Overview of left atrium phasic volumes using real time three dimensional echocardiography. J Cardiol Curr Res. 2019;12(1):8-10. DOI: 10.15406/jccr.2019.12.00421
The reservoir, conduit, and contractile phasic volumes and functions of the left atrium (LA) are important to understand overall cardiac performance. As far as recent studies are concerned, the accurate assessment of LA phasic functions and structure, using techniques such as conventional two-dimensional echocardiography (2D-echo), real time three dimensional echocardiography (RT3DE), color tissue Doppler imaging (TDI), and speckle tracking echocardiography (STE), as well as cardiac computed tomography (CT) and magnetic resonance imaging (MRI). This review article explains how to determine the LA volume and functions using RT3DE and emphases their relationship with current diseases.
Keywords: left atrium, two-dimensional echocardiography, computed tomography, tissue doppler imaging
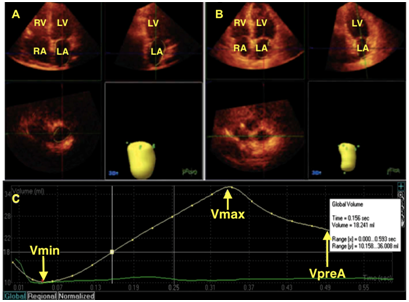
The importance of the LA in cardiovascular performance has long been acknowledged. The LA plays a pivotal role in stroke volume by modulating left ventricular (LV) filling with its reservoir, conduit, and contractile functions (Figure 1).1 The LA acts as a volume sensor of the diastolic burden, and communicates with the neurohormonal systems via the secretion of atrial natriuretic peptides.2 There is notable interplay between LA and LV function, such that events during each phase of “LA phasic function” are affected by factors from both the LA and LV.
Left atrium volume and measurements
LA size increases with conditions of pressure overload, such as mitral stenosis and increased LV filling pressures, and conditions of volume overload, such as mitral regurgitation. LA size reflects the average effect of LV filling pressures over time, making it a useful marker of the severity of LV diastolic dysfunction.3 Measuring the maximum LA volume using conventional 2DE at the time of mitral valve opening is now routinely performed with calculation with a formula, but it only represents a snapshot of LA function at a specific point of the cardiac cycle and also its an assumption compare to RT3DE.4 In daily practice, prognostic information may be obtained by assessing LA phasic volumes (maximum LA volume [LA max], pre-atrial contraction LA volume [LA preA], and minimum LA volume [(LA min]) and deriving LA stroke volumes (Table 1).1
Reservoir function |
Conduit function |
Contractile function |
Total LA SV = LA max -LAmin |
Passive LA SV = LA max -LA preA |
Active LA SV = LA preA - LA min |
Total LA EF = total LA SV/LAmax |
Passive LA EF = passive LA SV/LAmax |
Active LA EF = active LA SV/ LA pre A |
Table 1 Left atrium phasic volumes and functions
LAmax, left atrium maksimum volume; LAmin, LA minimum volumme; LA preA, left atrium preatrial contraction volume; LA SV, left atrium stroke volume; LA EF, left atrium emptying fraction
In comparison with other current imaging modalities, the cardiac MRI and CT have higher spatial resolution than RT3DE.5,6 Another disadvantage of RT3DE is related with LA appendage. It has a considerable role for the function of LA. On account of shape of the LA appendage and the oblique position of the interatrial septum calculations may be resulted with errors in RT3DE.7 That is the reason why echocardiography systematically tends to underestimate LA volumes when compared to MRI or CT. On the other hand, RT3DE is more available and cost effective then the others in daily usage.8
Clinical implication and current researches
According to current researches, RT3DE is most suited to measuring phasic LA volumes among the other modalities. Because, it allows the assessment of individual LA function components and furthers our understanding of LA pathophysiology in various disease states. Kanar et al.9 measured LA phasic volumes and functions in hypertensive patients using RT3DE and revealed that LA phasic volumes and mechanical functions are associated with hypertensive end organ damaged. Moreover, the observed LA dilation in hypertensive patients (increased LA max, LA min, and LA preA volumes) was associated with augmentation of reservoir and conduit functions, but no significant change in atrial contractile function. In another RT3DE based study showed the relationship between LA phasic volumes and dysfunction with LV diastolic dysfunction and hypertensive retinopathy (according to the Keith-Wagener-Barker classification) in patients with systemic hypertension. The high grade hypertensive patients had higher LA phasic volumes and worse LV diastolic functions (higher E/e').10 In a RT3DE LA volumes measured study, Atas et al. demonstrated that Patients with type 2 diabetes mellitus were found to have increased LA volumes and impaired atrial compliance and contractility.11 Eventually, increased LV filling pressure due to systemic hypertension, diabetes mellitus ,or systemic diseases which can cause increased LV compliance might cause increase of LV phasic volumes and deterioration of the LA functions. Therefore, dedicated advanced LA imaging using RT3DE is mainly required in daily clinical practice. Currently, advanced in LA imaging may also provide new parameters with incremental prognostic information over existing techniques and ultimately improve management.
None.
None.
None.
Author declares that there is no conflict of interest.

©2019 Kanar. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.