Journal of
eISSN: 2373-4396


Case Report Volume 6 Issue 2
Division of Cardiology, USA
Correspondence: Najam Wasty, Director, Cardiac Catheterization Laboratory, Associate Professor of Medicine, Newark Beth Israel Medical Center, 201 Lyons Avenue, Newark NJ 07112, USA, Tel 5713370963
Received: July 10, 2016 | Published: July 14, 2016
Citation: Sekhar A, Khakwani MZ, Cohen M, Wasty N (2016) Novel Use of the “Contra Catheter†(CC) In Proximal Iliac Artery Chronic Total Occlusion (PICTO) Recanalization. J Cardiol Curr Res 6(2): 00201. DOI: 10.15406/jccr.2016.06.00201
Proximal Iliac Artery chronic total occlusion (PICTO) interventions via contralateral femoral approach are challenging due to the lack of catheter support. In patients with the appropriate anatomy, the Contra Catheter (CC) grasps the aortic bifurcation like a clip and can facilitate crossing of the occlusion. We describe three cases with PICTOs in which the CC was able to provide adequate support with a contralateral femoral approach and obviate the need for an arm approach.
Keywords: AortoIliac occlusion, Iliac endovascular Intervention, TASC D, Peripheral artery disease
Proximal Iliac Artery chronic total occlusions (PICTOs) are complex peripheral interventions that typically require an arm approach for adequate leverage. These are typically Trans-Atlantic Inter-Society Consensus1 (TASC) Type C/ D lesions that have traditionally treated by Aorto-bifemoral surgery2 but are being increasingly approached by endovascular methods.3,4 The endovascular approach4 may be the only option in some patients who are poor surgical candidates due to age, lung disease and comorbidities that typically seen in patients with severe PAD. In addition, endovascular approaches have inherent advantages in that they are less invasive with a shorter length of stay and early recovery and can be performed with local anesthesia1 and can provide durable results.5
PICTOs are especially challenging for endovascular approaches as these cases can be complicated by lack of equipment to be able to treat disease distal to the iliac via a radial approach and may require brachial6 or axillary approach with associated risks. The most common reason for failure of an endovascular approach in CTOs is inability to cross the CTO with a guidewire.7 In cases with a retrograde femoral approach from the ipsilateral side can be complicated by difficulty in obtaining femoral access and if successful access is obtained, there can be difficulty in crossing the distal cap and use of re-entry devices is fraught with the risk of causing perforation especially with unpredictable level of re-entry into the Aorta.
The contralateral femoral approach is less risky as the CTO is approached from the Aorta but in cases of very proximal occlusions, crossing the proximal cap can be difficult. In these PICTOs, inability to cross with the guidewire via the contralateral femoral approach is due to the lack of catheter support resulting in the catheter backing out.8
The Contra Catheter (Boston Scientific Corporation, Massachusetts) can be a useful tool in PICTO cases with a contralateral femoral approach as it grasps the aortic bifurcation like a clip without backing out because as one pushes the wire down the clipping action of the contra catheter prevents it from backing up. Here we describe three cases with PICTOs which were successfully recanalized via a contralateral femoral approach using the Contra Catheter (CC).
Case 1
A 66 year old African American female Jehovah’s witness with a history of CAD s/p CABG, Diabetes, Tobacco use and PAD with Right Iliac and Left SFA stents presented with a 2 week h/o severe left lower extremity claudication extending from Left buttock and thigh to calf and foot and was noted to have a cooler Left lower extremity without palpable pulses in the left femoral and weak left popliteal and left posterior tibial pulse detected by Doppler consistent with critical left lower limb ischemia.
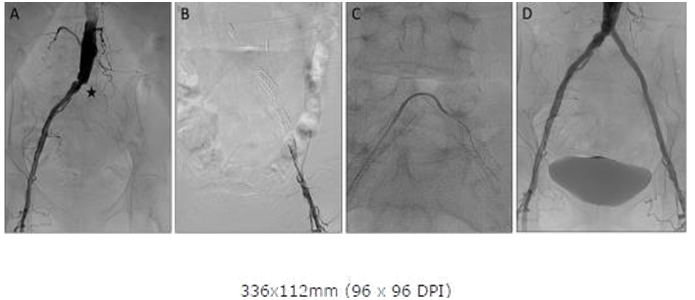
Right Common Femoral Artery (CFA) access was obtained and abdominal angiogram revealed a left proximal Iliac occlusion (Figure 1A) with reconstitution at the left femoral bifurcation (Figure 1B). Left CFA access was obtained with fluoroscopic guidance and a 6 Fr sheath placed in the Left CFA. Attempts were made with a 0.035 angled glidewire through the 6 Fr sheath from below but were unsuccessful in crossing the distal cap of the occlusion and a the wire was noted to enter a subintimal plane. A CC was advanced from the Right CFA and pulled down to firmly clip the aortic bifurcation (Figure 1C). A 0.035 stiff angled glidewire was then slowly advanced through the PICTO from the CC above without catheter back out and able to exit into the true lumen below. The wire was then snared and externalized through the Left CFA sheath. Once the wires were positioned true lumen to true lumen, the rest of the case was finished using standard stenting techniques and the left PICTO was recanalized with an excellent angiographic result (Figure 1D). The patient was claudication free at 1 month follow up without any complications.
Case 1
Figure 1A: Abdominal Aortogram showing Left Common Iliac occlusion and proximal cap (asterisk). Note previous stent in Left common iliac.
Figure 1B: Angiography from sheath inserted in Left femoral showing dissection due to attempts at retrograde crossing from left.
Figure 1C: Contra catheter with angled glide from right seated at bifurcation with clip like action providing support for crossing occlusion.
Figure 1D: Abdominal Aortogram post stenting showing good angiographic result.
Case 2
A 56 year old Caucasian male with a history of CAD s/p coronary stents, Diabetes, PAD s/p right iliac stenting presented after failed Left Iliac revascularization with critical limb ischemia of left lower extremity.
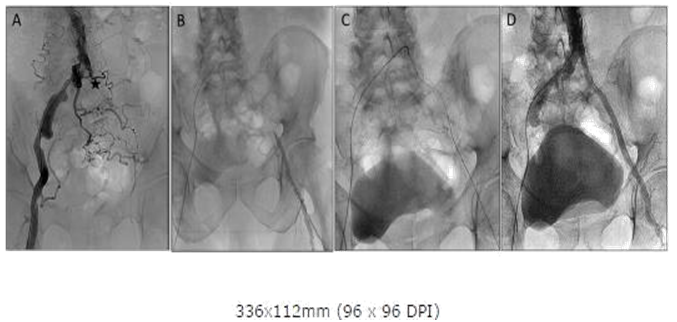
Abdominal angiography revealed a left PICTO with ostial left common Iliac occlusion (Figure 2A). Lt femoral access was obtained but despite multiple attempts the occlusion could not be crossed from below with an 0.035 wire (Figure 2B) and appeared to enter a dissection plane. A CC was again positioned in the aortic bifurcation and a 0.035 glidewire was then slowly advanced through the PICTO from the CC above and used to cross the PICTO. Once the wire crossed the occlusion with the support of the contra catheter and was confirmed to be in the true lumen, it was snared from below and externalized through the left sheath (Figure 2C). The procedure was then completed with standard stenting with final kissing balloon dilatation with an excellent angiographic outcome (Figure 2D) and the patient was complication free on follow up at one month.

Case 2
Figure 2A: Abdominal Aortogram showing ostial Left Common Iliac occlusion (asterisk).
Figure 2B: Angiography from sheath inserted in Left femoral showing distal cap and wire in subintimal plane and Contra catheter in distal Aorta.
Figure 2C: After crossover with Contra and angled glide from right and snaring the wire from the left sheath.
Figure 2D: Final Abdominal Aortogram after stenting showing good angiographic result.
Case 3
A 78 year old male with a history of CAD s/p CABG, CVA, tobacco use and PAD s/p stents in both lower extremities presented with critical limb ischemia, gangrene of toes of the left foot and non-healing left foot ulcer with ABI of 0.37.
Similar to case 1, Abdominal angiography revealed a left PICTO (Figure 3A) and Lt femoral access was obtained but could not cross the occlusion from below with an 0.035 wire and appeared to enter a dissection plane. A CC was again positioned in the aortic bifurcation (Figure 3B) and a 0.035 glide wire was then slowly advanced through the PICTO from the CC above and the two 0.035 wires lay juxtaposed midway allowing the wire being advanced from below to find the true lumen via the channel of the wire approaching from above (Figure 3C). Once the occlusion was crossed from below and wire position confirmed to be in the true lumen the revascularization was completed with a good angiographic outcome (Figure 3D) and the patient was complication free on follow up at one month.
Case 3
Figure 3A: Abdominal Aortogram showing Left Common Iliac occlusion and proximal cap (asterisk).
Figure 3B: Angiography from sheath inserted in Left femoral showing distal cap- attempts at wiring from sheath entered subintimal plane.
Figure 3C: Contra catheter with angled glide from right created a channel though which glide wire with Rubicon succeeded in crossing from distal cap. The contra catheter in this case assisted in creating a channel and guiding the wire from the Left.
Figure 3D: Final Abdominal Aortogram after stenting showing good angiographic result.
As demonstrated by the success of the above cases, the Contra catheter (CC) with its the clip like configuration, once snugly nestled in the aortic bifurcation from the contralateral femoral approach, could be harnessed to provide a stable platform to partially or completely burrow through a PICTO obviating the need for the usual simultaneous arm approach typically employed by most operators to gain more purchase from above. Another approach that has been described for such cases involves use of a brachial approach with a 7Fr system with contralateral Iliac balloon occlusion for support.6,9 Our approach is simpler and avoids balloon occlusion for support and brachial access with their associated risks. Our approach is also less risky than a “pure” retrograde approach from the ipsilateral femoral as it is easier to confirm position in the true lumen in the Aorta and can lower the risk of perforation or dissection at the distal Aorta10 without requiring complicated imaging guided reentry devices.8 This approach is also less aggressive and worth attempting before trying more radical methods such as stiff end of wires and sharp needles as described in other reports.7 There are additional factors that may have contributed to the success in the described cases. The presence of calcification, absence of a stump, and retrograde approach, has all been described as predictors of failure.11 The occlusions described were not heavily calcified and the amount of support provided by the CC may not be sufficient in cases with a more recalcitrant proximal cap. The success of this technique also rests on the ability to position the CC in the Iliac bifurcation with a snug fit and can be complicated by cases with unfavorable anatomy such as those with ostial flush occlusions and excessive angulation. In the first case described above, the CC was successful despite the occlusion being located in a very proximal portion of the Iliac as the CC was able to snugly fit in the distal Aorta.
As demonstrated in the above cases, this technique can be especially useful in cases where a retrograde approach via the distal cap is unsuccessful and enters a subintimal plane as seen in figure 1B and 3B. In these cases aggressive attempts at retrograde crossing can be disastrous due to the risk of Iliac perforation. The major advantage of this technique is that it avoids an additional upper extremity access and can also assist in treating further stenoses distal to the Iliac in the same setting which may not be possible via a radial approach. The development of a CC with even more elastic recoil and grip may further facilitate this simpler approach to PICTO recanalization. Additional studies are required to evaluate predictors of success with this approach such as duration of occlusion and favorable anatomical factors.
The clip-like configuration and action of the commonly used CC may provide adequate support to tackle a PICTO from the contralateral CFA obviating the need for a simultaneous arm approach. The approach described with CC is simple, affordable and less invasive than other options and can be a valuable technique in the algorithm of endovascular approaches to PICTO recanalization.
The authors would like to thank Dr Mohammad Al- Madani for assistance with cases and comments and Dr. Gail Baker for her assistance in the follow up care of the patients.
The authors declare there is no conflict of interests.
The authors declare there is no conflict of interests.

©2016 Sekhar, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.