Journal of
eISSN: 2373-4396


Case Report Volume 11 Issue 3
Cardiology department, Hospital Senhora da Oliveira-Guimar
Correspondence: Margarida Oliveira, Cardiology department, Hospital Senhora da Oliveira-Guimarães, Rua dos Cutileiros n114, 4835-044 Guimarães, Portugal, Tel 351 253540330
Received: February 20, 2018 | Published: May 25, 2018
Citation: Oliveira M, Azevedo O, Faria B, et al. Left atrial myxoma: always so benign? J Cardiol Curr Res. 2018;11(3):141-142. DOI: 10.15406/jccr.2018.11.00387
Primary tumour of the heart are rare. Cardiac myxomas are the most common ones and usually described as benign masses but they have the potencial to cause serious embolic complications and heart failure. We report the case of a 57-year old woman with a giant left atrial myxoma which presented with ischemic stroke. The mass caused also heart failure symptoms trough transmitral flow obstruction. After surgery for mass removal she remained asymptomatic. Tumor size has been discussed as a risk factor for embolism. Here we present a patient with a giant left atrial myxoma and 2 episodes of embolism. We also emphasize the importance to always keep myxomas in clinician’s minds to timely diagnose and treat this apparently benign entity but that can have disastrous complications.
Keywords: Cardiac mass, myxoma, stroke, heart failure
Primary tumours of the heart are rare, with an incidence ranging between 0.0017% and 0.19% in autopsy series. Atrial myxomas are the most common primary heart tumours.1,2 They are found in all 4 cardiac chambers but in 75% of cases they arise in the left atrium3‒6 most of them involving the interatrial septum. The imaging modality of choice remains the echocardiogram but there are other imaging methods that allow mass visualization and better characterization as computed tomography and magnetic resonance imaging.
Patients with myxomas may remain asymptomatic or present with a wide variety of symptoms ranging from symptoms of heart failure to embolism or constitutional symptoms.7 Embolism is a major complication reported in 6-45% of patients with cardiac myxomas and in most of cases affecting brain circulation. Risk factors for embolism are reported to be associated with tumour pathology and villous configuration in which irregular composition and shape of tumour may be prone to shedding of fragments with distal embolization.8 Surgical removal is the recommended therapy and is curative in most cases.8
We report a case of a 57-year-old female, with previous history of smoking, hyperlipidaemia and history of ischemic stroke without residual deficits. She was ordered a transthoracic echocardiogram (ETT) to rule out cardiac embolism which revealed an echogenic left atrial mass of huge dimensions (5.8x2.8cm) connected by a small pedicle to the interatrial septum and prolapsing into the left ventricle in diastole causing transmitral flow obstruction (Figure 1) (Figure 2). Doppler revealed a mean pressure gradient between left atrium and ventricle of 9.71mmHg (Figure 3). Transthoracic 3D echocardiography allowed a better characterization of the mass and its attachment to the interatrial septum (Figure 4).
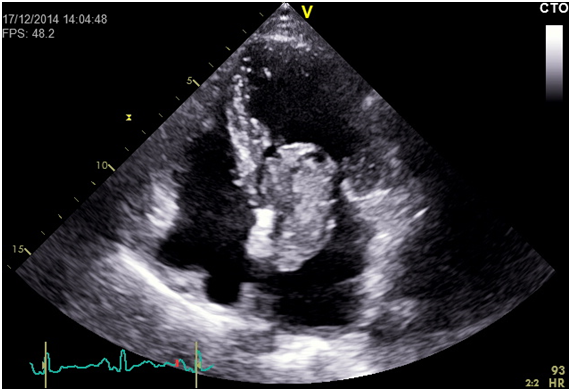
Figure 1 Ecocardiographic 4-chamber view showing giant left atrial myxoma prolapsing into left ventricular in diastole.
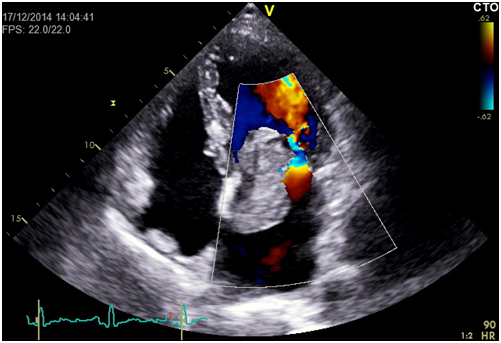
Figure 2 Echocardiographic 4-chamber view with colour doppler showing turbulent flow caused by transmistral flow obstruction by the giant left atrial myxoma.
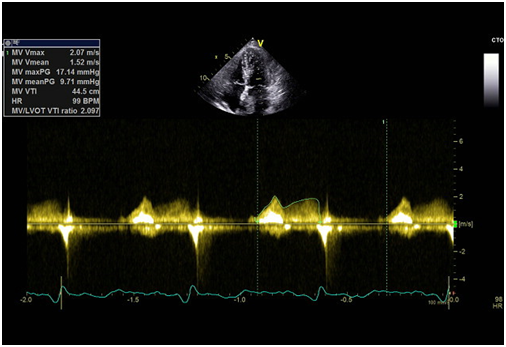
Figure 3 Transmitral doppler flow showing the elevated mean pressure gradient between left atrium and ventricle.
When she was first evaluated, her symptoms were mild with dyspnoea for moderate exertion that she reported to be common and that she always related to smoking. While she was performing pre-operative exams, she had a new episode of ischemic stroke without residual deficits. Until surgery was performed she progressed in heart failures symptoms with dyspnoea with only minimal exertion and orthopnoea. The mass was surgically removed and pathological analysis confirmed the clinical suspicion of myxoma. One month later, the patient was asymptomatic.
Myxomas are known as ‘benign’ tumours but they can have malignant complications if not timely diagnosed and treated. Systemic embolization is one of the most serious and frequent complications, being the second most commonly reported complication from the classic triad of myxomas. In most cases, central nervous system circulation is affected but emboli may migrate to any vascular bed – upper and lower extremities, eye, kidney, liver, coronary arteries. Although myxomas are a rare cause of ischemic stroke (less than 1%), this case emphasizes the indication to perform TTE in every patient diagnosed with acute stroke. This indication is even stronger in patients of young age and in the absence of conventional risk factors. In this case the patient remains without neurological deficits, but if she had not been properly diagnosed and treated, ischemic events may have recurred and caused devastating damage.
Tumour size has been discussed as a risk factor for embolism but it remains inconsistent in previous studies.8,9 Some studies report no effect of tumour size8 while other show a tendency towards great risk of embolism with bigger masses (diameter > 5cm).9 In this case the patient presented with a huge mass in the left atrium and recurrent ischemic stroke, which supports the claim that myxoma size is a risk factor for systemic embolism. Cardiac myxomas are a rare cause of ischemic stroke but that physicians should kept in mind, most importantly in patients without conventional risk factors. Cardiac surgery is curative in most cases.
We declare that consent form was obtained to publish the clinical report.
There is no conflict of interest to be declared.

©2018 Oliveira, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.