Journal of
eISSN: 2373-4396


Opinion Volume 4 Issue 1
Cardiology Consultant, Medical Investigation Unit, Saint Bernard?s Hospital, Gibraltar
Correspondence: Sergio MejíaViana, Cardiology Consultant, Medical Investigation Unit, Saint Bernards Hospital, Harbour views road GX 111 AA Gibraltar, Tel 34 687445794
Received: November 23, 2015 | Published: November 23, 2015
Citation: Viana SM, Haberman D, Shimoni S. From framingham to hunt 2: 60 years blaming the wrong culprit? J Cardiol Curr Res. 2015;4(1):119-122. DOI: 10.15406/jccr.2015.04.00131
cholesterol, risk factors, cardiovascular disease, prevention, statins, coenzyme Q10, guidelines; secondary effects, atherosclerosis, inflammation
Every single cell in the human body is comprised of cholesterol. What is it doing there? The body manufactures cholesterol for a reason. Cholesterol is a primary constituent that provides cell membranes with their integrity. Without adequate cholesterol, cells will literally leak, falling apart in the bloodstream. Another critical function of cholesterol is to serve as an anti-inflammatory, preventing the formation of pro-inflammatory lipids, which when left unregulated generate high amounts of free radical. If unbound, arachidonic acid (AA), one of the omega 6 fats, can convert into pro-inflammatory lipids such as thromboxane and leukotriene. Adequate cholesterol can prevent this from happening.1,2
Thromboxanes are members of the eicosanoids signalling molecules which are the result of oxidation. Thromboxanes are vasoconstrictors, causing platelet aggregation as well as agglutination of red blood cells. Leukotrienes and prostaglandins are also fatty acid signalling molecules that are strongly involved in inflammatory responses. Each of these 3 proinflammatory fatty acids are inhibited by adequate cholesterol.3,4 Low density lipo-protein (LDL) is the “carrier” of cholesterol, sending out cholesterol to various parts of the body where needed. High density lipo-protein takes cholesterol back to the liver. If there is high LDL, this indicates that there is a greater need for cholesterol in the tissues of the body. Calling LDL “bad” does nothing to address what is really happening. Why is LDL elevated? In such a case, there are most likely pro-inflammatory conditions taking place in the body, which require additional cholesterol to halt excessive inflammation in the tissues. Basically, cholesterol is doing exactly what it is supposed to be doing, protecting you from harmful free radicals and cellular death. But the real question should be: why is there inflammation in the tissues? High serum cholesterol could be solely a risk marker that is secondary to the real causes.5
Cholesterol is, as well, the precursor of multiple hormones and vitamins: Adrenal hormones (cortisol and aldosterone), sexual hormones (Estrogens, progesterone and testosterone) and vitamin D. The mentioned hormones are synthesized through minor modifications of the cholesterol molecule in adrenal, ovarian and testicular cells. And vitamin D metabolism starts in the skin cells by the activation of cholesterol by sunlight.6 Moreover, cholesterol is the precursor of five bile acids that help in digestion by facilitating the absorption of fats and acting as transcription factors that take control on steroids levels and COX-2 synthesis.7 Does cholesterol exist in our cells so that it can kill us? In this scenario, calling LDL “bad” and HDL “good” is a big mistake in which our current practice is based upon. A huge number of studies suggest that some risk factors for coronary artery disease, like stress (emotional and physical), high carbohydrate diets and smoking may elevate total cholesterol and low density lipoproteins levels.8,9 Also, it is interesting to notice that in stress conditions, high carbohydrate diets and cigarette smoking there is a significant elevation in blood lactate levels. If cigarettes do not contain fat or cholesterol, and smoking ends up “depositing” fat and cholesterol in the artery walls, what is the mechanism for that? Clearly, cigarette smoking remains a leading preventable cause of mortality, much of it due to cardiovascular disease.10
Atherosclerosis is not a single disease entity. In fact, the lesions of atherosclerosis represent a common response of the artery to numerous and potentially different forms of insult. Examination of atherosclerotic lesions reveal that each lesion contains the elements of an inflammatory response together with varying levels of fibro proliferative response.11,12 The early lesion, called fatty streak, consists largely of monocyte-derived macrophages and T lymphocytes. Thus, it is a pure, highly specialized inflammatory response. The intermediate and advanced lesions also contain these elements, together with smooth muscle cells, which migrate, proliferate and lay down extracellular matrix, presumably as part of a healing response to the insult and inflammation. Together with the inflammatory-fibro proliferative response, both intracellular and extracellular lipid accumulation can be found in association with many of the lesions.13
Numerous prospective epidemiological studies have identified a direct relationship between serum total cholesterol level and coronary heart disease incidence.14 Since the Framingham study it has long been considered common knowledge that total serum cholesterol is a strong independent risk factor for cardiovascular disease. This study started in 1948 and has been cited thousands of times as one of the most important epidemiological sources in the risk factors field. During the last decades, cardiovascular disease prevention has been marked by a trend of gradually lowering thresholds of cholesterol levels.15 Campaigns aimed at the general public have underlined the risks associated with total cholesterol above 5.0 mmol L-1.
On the other hand, research continues on defining the actual importance of C-reactive protein (CRP) as an indicator of cardiovascular risk, thus inflammation, as reflected by an elevated CRP, has always been the major factor underlying atherosclerosis.16 Ravnskov et al.17 have written extensively about the holes in the cholesterol theory, and that mainstream medicine´s obsession with reducing cholesterol levels has always been misguided.17 CRP levels are improved by the same factors that improve cardiovascular health: exercise, balanced diet, maintaining a healthy weight and not smoking. Women should be aware that the hormonal therapy for menopausal symptoms might raise their CRP level considerably.18
Some researchers, non-supported by the pharmaceutical companies have questioned the overestimation of coronary risk factors in authoritative clinical guidelines. Getz et al.19 demonstrated that, following current guidelines that recommend a total cholesterol level of less than 5 mmol L-1, more than 75% of the adult population in Norway would therefore require clinical attention.19 The main problem could arise when we forget that correlation is not causation. One can find statistical studies that correlate divorce rate in Main with the per capita consumption of margarine, or the age of miss America with murders by steam hot vapours and hot objects. (Spurious correlations. Tylervigen.com). Obviously, statistical correlation is not causation but in modern evidence based medicine, statistical correlation is assumed and accepted in a wide variety of trials and meta-analyses in which current guidelines are based on.
There is also statistical evidence that correlates low serum cholesterol and other diseases. It is worth mentioning the paper of Tsuji and others that reported increased atrial fibrillation with lower cholesterol levels, independent of the thyroxin level which paradoxically increases the cardioembolic stroke incidence in patients with cholesterol lowering therapy.20 Let’s have a word about statins. Many doctors believe that cholesterol is the main culprit, and that an elevated cholesterol level automatically means treatment with one of the statin drugs. So it is no surprise that statins are the most prescribed drugs in many countries. Some doctors are so enthusiastic about statins’ ability to reduce cholesterol levels (which is proven truth), that they call statins “miracle drugs” and stated that heart attacks might disappear before the end of this century.21 Most of them also claim that statins cause no side effects but muscle pain, and that everyone over age forty should be taking a statin regularly.
Statins were discovered in 1980, launched to public pharmacological market in 1994 with the 4S, a secondary prevention trial that tested mortality at 5 years and dared to conclude that “long term” treatment with simvastatin improves survival in CHD patients. In absolute numbers, 189 (28%) deaths in the placebo group vs 111(19%) in the simvastatin group.22 Since then a huge amount of sponsored trials, new molecules, exciting presentations, and lots of sales representatives appeared giving us the evidence to defeat cardiovascular diseases: Cholesterol is bad, statins are good. However, we must take a detailed look at the statins’ mechanism of action. As shown in Figure 1, statins act blocking the HMG-CoA reductase in the mithocondrial mevalonate pathway. It will definitely lower the production of Cholesterol and Ubiquinone, also known as Coenzyme Q10. We have already learned that most of the body´s energy metabolism occurs in the mitochondria through a process called oxidative phosphorylation. Electrons are transported through this pathway down the electron transport chain, where they give up their energy to generate ATP from ADP. Coenzyme Q10 is a vital link in the electron transport chain, picking up electrons from one membrane of the chain and dropping them at the door of another. A deficiency or imbalance in any part of the system may contribute, over time, to the impaired functioning of cells, tissues, organs and eventually the entire body.23
Coenzyme Q10, a fat-soluble compound, has powerful antioxidant activity. As an antioxidant, its reduced form inhibits peroxidation in cell membranes and serum LDL, and it also protects proteins and DNA from oxidative damage. This is; it plays a vital role in combating free-radical stress. Coenzyme Q10 is involved in the reactions of at least three mitochondrial enzymes, rendering it the most essential component of the electron transport chain and is an important antioxidant. Without coenzyme Q10 our bodies cannot survive Figure 1.24
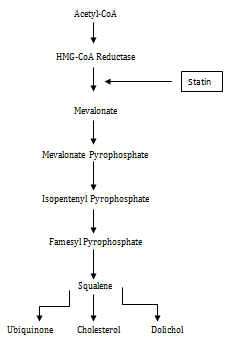
Figure 1 The mevalonate pathway. HMG-CoA reductase is inhibited by statins which affects ubiquinone synthesis.
So I make no mistake by saying that a long term treatment with a statin is an iatrogenic mitochondrial disease. Where do we find mitochondrial disease, frequently named as a “rare condition”? In Parkinson´s disease, Alzheimer´s, chronic fatigue, cardiomyopathy, diabetes, fibromyalgia, unexplained kidney disease, unexplained heart failure, multiple sclerosis, epilepsy, etc. Sounds familiar? Sixty years ago the impressive Framingham study, a longitudinal epidemiological study that included about five thousand people, gave out the basis to find the risk factors of ischemic heart disease: smoking, high blood pressure, high cholesterol, diabetes mellitus, obesity and family history. The extrapolation of data found in a small village near Boston to the rest of the world gave birth to decades of theories and investigation efforts ending in current clinical practice. The majority of those risk factors have been proven in clinical practice. All those factors increase inflammation and oxidative stress all over the body. But as mentioned above, cholesterol is there, maybe not creating the problem, but trying to solve it as an important anti-inflammatory tool used by the body´s defence systems.
The HUNT 2 study, a very elegant prospective study in Scandinavia (the same region where the 4S took place) included 52087 Norwegians, aged 20-74, that were followed-up on cause-specific mortality for 10 years. This is 510.297 person-years in total. The statistical power and the lack of conflict of interest make this a heavy evidence source, even stronger than Framingham. Based on their results, they clearly contradict the popularized idea of a positive, linear relationship between cholesterol and fatal disease, and conclude that the underlying assumptions regarding cholesterol in clinical guidelines for prevention might be flawed.25 This study could suggest that, like any other substance in the body, like thyroid hormone for instance, total cholesterol should be in a balanced situation, not too high, not too low. According to their presented results, between 5 and 7mmol L-1 would be the desired level. They reported an interesting low mortality rate among post-menopausal women with a mean cholesterol level of 7 mmol L-1.
Sugar, processed food, stress, heavy metals and radiation are surrounding us on a daily basis. They are the main source of free radicals, oxidative stress and inflammation nowadays. Many physicians are just prescribing cholesterol lowering drugs because we have been blaming the wrong culprit and we still are. Population studies reveal that, although we live longer, the quality of life in terms of a “doctor free life” is dropping down dramatically. The 3rd cause of mortality in the US is iatrogenic caused diseases.26 In an optimal healthcare system, solutions for many disorders would begin with nutrition, then natural interventions, then pharmaceuticals. But it is important to blame the correct culprits.
To Juan García, clinical physiologist for the careful proof reading.

©2015 Viana, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.