Journal of
eISSN: 2373-4396


Review Article Volume 2 Issue 2
University Clinic of Cardiology, Macedonia
Correspondence: Marjan Boshev, University Clinic of Cardiology, Rugjer Boshkovikj 5/2-3, - Skopje, Macedonia, Tel 3877540808
Received: December 08, 2014 | Published: March 3, 2015
Citation: Boshev M. Does transradial approach become a golden standard for percutaneous coronary interventions? J Cardiol Curr Res. 2015;2(2):42-44. DOI: 10.15406/jccr.2015.02.00053
Transradial approach (TRA) in percutaneous coronary interventions (PCI) today becomes widely accepted and practiced procedure worldwide. TRA for PCI is safe and fast growing alternative to transfemoral approach (TFA) in many clinical settings and it is the desirable vascular access for most highly experienced operators. Although the TRA provides many clinical and economical benefits, may be the most important advantage is a decreased rate of vascular access-related bleeding complications after PCI. TRA is associated with certain learning curve and generally it requires higher technical skills of the operator compared to TFA. If progressive use of TRA for PCI continues to rise over next several years, we can expect soon TRA to become a golden standard for PCI procedures. Radial artery occlusion (RAO) remains one of the possible consequences of TRA especially if repeated PCI is performed via the same radial artery. TRA is feasible and effective approach for PCI in vast majority of patients and its value becomes especially important in high risk subset of patients including STEMI patients. The main advantages over TFA include lower rate of access-site bleeding complications, lower mortality in STE-ACS, better patient comfort, early ambulation and shorter in-hospital stay and they are clearly documented today.
Keywords: transradial approach, percutaneous coronary interventions, transfemoral approach
TRA, transradial approach; PCI, percutaneous coronary interventions; RAO, radial artery occlusion; TFA, transfemoral approach
Transradial approach (TRA) in percutaneous coronary interventions (PCI) today becomes widely accepted and practiced procedure worldwide. TRA for PCI is safe and fast growing alternative to transfemoral approach (TFA) in many clinical settings and it is the desirable vascular access for most highly experienced operators. The radial artery is a preferred approach because perfusion of the hand can remain uncompromised even in case of radial artery occlusion (RAO) due to double arterial vasculature including ulnar artery and a palmar vascular arch.1
Although the TRA provides many clinical and economical benefits, maybe the most important advantage is a decreased rate of vascular access-related bleeding complications after PCI.1˗4 In general, bleeding complications which frequently can be life threatening in the clinical settings of acute coronary syndrome (ACS) have lower rate if TRA is used. Nonetheless, clinically significant bleeding events may still occur, although less frequently and in these cases they are usually associated with poorer outcome. That is the reason they cannot be ignored even with TRA, but vascular adverse events profile in TRA appears to be different in comparison to TFA concerning nature and frequency of events.
Percutaneous treatment of ST-elevation myocardial infarction (STEMI) has been permanently improved over time and today general outcome is significantly better. Despite this improvement, patients with STEMI undergoing invasive procedure and PCI (primary PCI, PPCI) still represents a high risk subset of population that have lower survival rates, higher rates of procedural failure, as well as more bleeding complications compared to those undergoing elective or staged PCI or even PCI for NSTE-ACS. It seems that bleeding appears to be a major risk factor linked to higher mortality in the STEMI population, and strategies developed towards bleeding reduction are also related to lower mortality rate. TRA represents a relatively novel vascular approach which lowers bleeding risk in this cohort of patients. The association between TRA PPCI and reduced mortality rate has been thoroughly showed in one meta-analysis of radial PPCI studies and we must emphasize that it was driven by limiting post procedural cardiovascular and hemorrhagic complications.3,5
Knowing the learning curve associated with accepting TRA PCI, starting a TRA PPCI program should be planned for experienced operators and cat lab personnel who are familiar with and are often involved in complex TRA PCI (long or calcified lesions, bifurcation lesions, LM lesions, etc).5 There are several procedures that can improve the general performance of TRA PPCI.
Another practical advice is recommendable and sometimes preferable use of the left TRA for PPCI because of the lower incidence of proximal vascular tortuosity compared to the right wrist approach.5˗7 Subclavian and brachiocephalic tortuosity have been reported as a frequent cause for TRA procedural failure in approximately 18-22% of cases. This can be particularly associated with advanced patients` age; therefore left TRA in selected, more frequently in older population (over 75years old) as well as sometimes in those with less than 165 cm in height may facilitate and shorten PPCI.4,5
Several well-known trials have showed that TRA is feasible approach for the treatment of STEMI (RADIAMI, FARMI, TEMPURA, RADIAL-AMI, RIVAL trial). However, each of these trials have recruited operators with relatively high proficiency in TRA PCI procedures (>100). In addition, operators achieved comparable procedural success rates and lower rate of bleeding complications compared to TFA. And which was more interesting and important, these studies generally confirmed that there was no statistically significant difference between TRA and TFA in terms of door-to-reperfusion time.3 As an example, the RIVAL study showed that TRA reduced the primary outcome (death, myocardial infarction, stroke or non-CABG related major bleeding within 30days) and mortality in patients presenting with STEMI,3,5 although there was no such benefit in patients presenting NSTE-ACS and these data suggest that TRA might be the preferred option in patients with STEMI.
As the number of TRA for PCI worldwide is growing up, one of the main obstacles the operators are facing with is the problem of radial artery occlusion (RAO), especially in patients with need for subsequent or staged PCI procedure. According to different statistics, up to 8% of patients after TRA PCI have developed RAO.4,8 This issue is most probably caused by micro injury of the arterial endothelium during catheter manipulation triggering further spasm and subsequent thrombosis. In most cases RAO is happening completely asymptomatic or rarely with subclinical expression. Several major risk factors promote RAO and they include higher arterial sheath diameter (6 or 7 F over 5 F), absent systemic anticoagulation, consecutive or repeated arterial puncture as well as irregular puncture-site hemostasis.2,8
Regarding these factors, minimization of the risk of RAO can be achieved by adoption of several strategies. Some of these strategies include use of parenteral anticoagulation (UFH – 5000 IU preferred over 3000 IU, LMWH or bivalirudin), low profile arterial sheaths (5 or 6 F) or sheathless catheters and supporting the concept of patent hemostasis.1,2,4 The concept of patent hemostasis means to perform adequate hemostasis that simultaneously maintains and promotes antegrade flow in radial artery. It is believed that this technique is of major clinical importance and current data showed that patent hemostasis significantly lower the rate of RAO.2,8 Some authors suggest that concomitant use of the medication Trimetazidine post procedurally (after performed coronary angiography) may potentially inhibit neointimal hyperplasia and prevent RAO.2 Another practical tip is performing angiography of the right (or left) forearm (˗) as a routine procedure1 immediately before coronary angiography. The main concept here is to minimize radial artery wall injury, thus minimizing the risk for radial artery thrombosis and RAO. Routine angiography of the forearm gives us all necessary data concerning radial artery anatomy and variations as well as possible difficulties traversing it (loops, tortuosity, high take-off, radial artery spasm etc). In such cases operator can directly visualize radial artery impediments, anticipate possible.
According to the Consensus document on the radical approach in PCI (position paper by the EAPCI and Working Groups on Acute Cardiac Care and Thrombosis of the ESC) published in 2013, TRA offers lower access-site bleeding rates, particularly in high-risk patients for thrombotic or hemorrhagic complications. According to current recommendations, total reduction of both access and non-access-site bleeding rates is expected when TRA is associated with optimized anticoagulation.1 Nevertheless, a default TRA is safe and feasible in routine practice after appropriate training (starting from diagnostic coronary angiography, going through simple PCI in elective patients, next through PCI in NSTE-ACS patients, coming to PPCI in STEMI patients), but proficiency in TFA (Figure 1) is required because it may be needed as a bailout strategy, thus better results with TRA are expected with increasing procedural volume of operators, says this document.
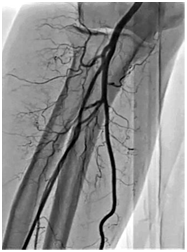
Figure 1 Angiogaram of the right forearm problems, minimize radial artery injury and find appropriate solution to surpass it.
Recently published 2014 ESC/EACTS Guidelines on myocardial revascularization have also shown that concerning procedural aspects in primary PCI for myocardial reperfusion in STEMI, TRA should be preferred over TFA if performed by an experienced radial operator (Class IIa, Level of evidence A).5,9 In conclusion, TRA is feasible, safe and effective approach for PCI in vast majority of patients and its value becomes especially important in high risk subset of patients including STEMI patients.3 The main advantages over TFA include lower rate of access-site bleeding complications, lower mortality in STE-ACS, better patient comfort, early ambulation and shorter in-hospital stay and they are clearly documented today.1˗3,10 Although use of TRA increases over time worldwide, proficiency in TFA is still required because sometimes it may be necessary as a bailout strategy or when higher profile guiding catheters are needed.1,10 TRA is associated with certain learning curve and generally it requires higher technical skills of the operator compared to TFA. If progressive use of TRA for PCI continues to rise over next several years, we can expect soon TRA to become a golden standard for PCI procedures. RAO remains one of the possible consequences of TRA especially if repeated or staged PCI is performed via the same radial artery. Therefore, procedural and pharmacological strategies which minimize radial artery injury during TRA PCI should be adopted by the operators and should be considered a key component of all transradial procedures.2,4
None.
Author declares there are no conflicts of interest.
None.

©2015 Boshev. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.