Journal of
eISSN: 2373-4396


Research Article Volume 14 Issue 5
1Department of Hypertension, Hospital Británico de Buenos Aires (Hospital Británico), Argentina
2Department of Cardiology, Hospital Británico de Buenos Aires (Hospital Británico), Argentina
Correspondence: Pronotti María V, Department of Hypertension, Hospital Británico de Buenos Aires (Hospital Británico), Argentina
Received: August 14, 2021 | Published: October 20, 2021
Citation: Pronotti, María V, Miguel SJ, et al. Arterial hypertension and telemedicine in times of pandemic. J Cardiol Curr Res. 2021;14(5):133-135. DOI: 10.15406/jccr.2021.14.00529
The pandemic caused by the SARS-COV-2 virus started in late 2019 in China and spread rapidly around the world. The great impact it had on hypertensive patients has generated a change in the medical care paradigm, giving impetus to a virtual care modality, telemedicine. The objective of this work is to evaluate the technique of blood pressure measurement (equipment and procedure), its knowledge in this regard and, based on this, educate the hypertensive patient. Material and methods: descriptive and observational study of 426 patients, over 18 years of age, who requested a consultation by telemedicine in a community hospital, during July and November 2020. The patient was questioned about the equipment used, the measurement technique and on the knowledge of the blood pressure figures that defined him as hypertensive. Results: Of 426 patients, 49% were 62-year-old women. 92.95% had a blood pressure monitor at home, of which 73% were electronic arm, 16.16% were electronic wrist and 10.84% manual. Only 53% had a validated blood pressure monitor. 35% of the total made at least 2 records and 39.2% knew their blood pressure values considered normal.
Keywords: high blood pressure, SARS-COV-2 pandemic, telemedicine
The pandemic outbreak of COVID-19 (produced by the SARS-Cov-2 virus) erupted in China on December 2019 and quickly spread around the world. Over 212 countries and territories have been and still are affected by the disease. In Argentina, the first case was reported on March 3rd 2020, and the first death by COVID-19 occurred on March 7th. On March 20th, quarantine was ordained at a national level.
COVID-19 has had an impact on patients with high blood pressure in several ways. In the first place, it has resulted in work termination and loss of health insurance, produced by economic decrease, physical inactivity resulting from mandatory lockdown, ordained quarantine, closure of gyms and recreation centers, and, in addition, has generateda change in medical attention for chronic disease, boosting attention through virtual methods, also known as telemedicine. In this context, self-measurement for arterial pressure (AP), which are random measurements performed by the patient, become of high importance to handle hypertension and cardiovascular failure prevention.1,2
Telemedicine is a technological tool not frequently used by Argentina’s health providers, not only because there is a general lack of knowledge, but also due to the low access rate for the lower class population and the elderly groups, who have a steeper learning curve. However, this resource could improve health services, save resources, expand capacity for specialized attention in remote locations, ease clogged traditional medical services (emergencies or spontaneous demand) and is also a priceless instrument for education and research. The COVID-19 pandemic forces us to extend its usage and presents us with the opportunity to have a proper implementation.3
Such a tool is a complement to health services that must be regulated and integrated into the medical attention channels. It requires having up-to-date and monitored settings, clear security and confidentiality protocols, reliable and certified tele-diagnosis and tele-monitoring software, resources for digital documentation storage and back-up, as well as support for education and research.
Considering this new format for care service, we as professionals wondered about the actual quality of blood pressure measurements, as reported by patients themselves. This concern arose in relation to the fact that such data would be the ground for health-decisions that would affect the aforementioned patients. The goal in our work was to evaluate the technique for blood pressure measurement (equipment and procedure), to understand the patients’ knowledge on the matter and, based on such findings, to educate patients with high-blood patients on the proper behavior.
This work covers a cross-sectional, consecutive study that involved patients who were provided with a telemedicine appointment at a community hospital between July and December 2020. The appointments consisted of a questionnaire for the patient to respond about the equipment used for blood pressure control and measurement technique. Patients were also queried on which figures for blood pression would define a patient to be hypertensive. Patients included were at least 18 years old, and all of them had made appointments to consult on arterial hypertension.
For all cases, the following data was requested: The patient’s age and gender; pressure meter available at their home or, if applicable, at the location where the measurement took place; which kind of pressure meter did patients had (manual or electronic). For electronic pressure meters, the brand and model was requested to evaluate its’ validity. The interview also covered the technique for measurements, mostly related to the amount of measurements performed by the patient.
Lastly, patients were queried on figure thresholds that delimit arterial hypertension.
The total amount of queried patients was 426, 49% of which were women with an average age of 62 years old (Figure 1).
A 92.95% (396 patients) had blood pressure equipment at home, out of which 73% (289 patients) had electronic arm gadgets and 16.16% (64 patients) had electronic wrist gadgets. The remaining 10.84% (43 patients) had manual blood pressure equipment (Figure 2 & 3).
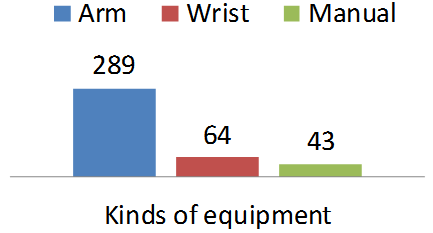
Figure 3 Kinds of pressure meters owned by patients.
Out of all surveyed patients, only 53% (210 patients) had a validated blood pressure equipment (Figure 4).
Lastly, knowledge about the disease was evaluated through the answered threshold value to determine arterial hypertension (taking into account that the expected values for at-home normal measurements were figures below 135 mmHg for systolic blood pressure and/or 85 mmHg for diastolic blood pressure) (Figure 4 & 5). Only 39,2% (167 patients) were in the know about these expected values (Figure 6).
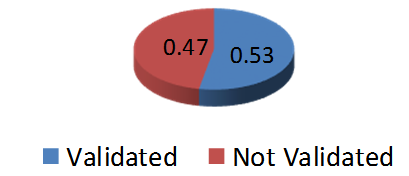
Figure 4 Percentage of patients with validated equipment
Regarding the technique in use for blood pressure measurement, only 35% (149 patients) performed at least 2 measurements (Figure 5).
There is sufficient evidence on the impact of blood pressure as a risk factor and how its adequate treatment helps to reduce risks for cardiac and cerebrovascular events in the medium- and long-term.4-5 Measurements in addition to those performed by physicians have become a useful aid for this. This procedure eliminates the alarm reaction and is more reproductible; it presents a greater correlation with end-organ damage and its regression; also a greater correlation with cardiovascular events within a population in general and within hypertensive patients who have or have not received treatment; and it better evaluates, in a more precise way, how much blood pressure has receeded after treatment.
The PAMELA study, which took place in 2005, concluded that blood pressure in a medical facility is less correlated to total mortality reduction and to cardiovascular mortality. Home blood pressure measured (HBPM) followed in terms of usefulness for the same matter, while ambulatory blood pressure measurements were correlated the most with the aforementioned events (ABPM).6
Medical guides recommend self-measurement of blood pressure as a way to improve control and treatment adherence.2-9 There is evidence on this kind of measurement diminishing blood pressure by the 6th and 12th month, regardless of any interventions occurring in the middle.10 The technique is simple, quick and has a low cost. The goal is to better classify patients, increase percentages for positive controls and avoid mistakes in blood pressure measurements that might result in over or underestimating actual figures, leading to make mistaken decisions.
It is of most importance to apply a proper technique, and there is a minimal set of concepts the patient must acquire so as to ensure a reliable measurement. It is also of interest for patients to know about validated equipment and normal thresholds for blood pressure. For this reason, medical guides and the Argentinian Consensus for Arterial Hypertension SAC/FAC/SAHA (2018) suggest a ABPM measurement or home-monitoring (HBPM) to perform an accurate initial diagnosis and an eventual treatment update, given that such procedures, unlike self-monitoring, involve a validated piece of equipment and a technique with specific application protocols.11
This observational study demonstrates that not many patients own validated pressure meters; also, most of the subjects do not apply a proper technique and the understanding rate on normal thresholds for hypertension is low.
It is to be concluded that blood pressure self-measurement provides clear evidence of it, but in order to make medical decisions, it is important that doctors educate their patients. The current pandemic brought the many gaps on the matter to the front, making a point about most of the recorded measurements have a similar quality to those of self-monitoring than to those expected out of a blood pressure home-monitoring.
The ongoing pandemic forced us to find new tools for medical assistance. When it comes to hypertension, one of the most important goals is the proper blood pressure control through monitoring blood pressure, regardless of the procedure involved (self-monitoring, ABPM or HBPM). It is to be considered that not all patients have the socioeconomic means to perform ABPM or HBPM. In any case, everyone should have the same access to education and blood pressure monitoring within a medical facility, being that a physical or virtual appointment. This last option could resolve the accessibility barrier. However, the study raised attention on the low amount of validated equipment, the lack of knowledge around measurement technique for blood pressure and also around the figures that could be expected for such measurements. For this reason, it is of high importance for a physician to enhance communication and educate the patient on the matter.
None.
No conflict of interest.
None.

©2021 Pronotti,, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.