Journal of
eISSN: 2373-4396


The aim of this study was to evaluate the role of surgical treatment for mediastinal tumors. A retrospective study was done from 6.8.2005 to 27.5.2014. Total 31 patients were included in this study. Age range was from 30 years to 70 years. Male was 18 and female was 13. Most of the tumour was thymoma (12 cases), thymoma with myasthenia gravis in 3 cases, Thymic carcinoma 2 cases, Nodular sclerosing Hodgkins lymphoma in 1 case, schawannoma in 2 cases, cystic mass in 5 cases, schawannoma with cystic degeneration in 1 case, fibromyxoma in 1 case, dermoid in 3 cases, teratoma in 2 cases, Fibrosing mediastinitis in thymic mass in 1 case, lymphoid hyperplasia in 1 case, malignant mesenchymal tumour in 1 case, myxoid liposarcoma in 1 case. Surgical exposure varies from strenotomy in 17 cases to clamshell incision in 1 case to postero-lateral thoracotomy in 12 cases and antero ateral thoracotomy in 1 case. Superior Venacava was injured in 1 case, repaired successfully by 6/0 prolene controlled by partial clamp. Some of the medistinal mass needed careful dissection from lung, pleura, encircling distal aortic arch and proximal part of left subclavian artery, encircling left brachiocephalic vein. 1 case needed Reconstruction of sternum with prolene mesh, marsupialization was done in 2 cases, adjacent pleura, fatty tissue, part of pericardium was removed in 5 cases. Lobectomy was needed in 1 case. In 1 case Recurrence of Fibrosing mediastinitis needed steroid therapy. Extensive growth of the tumour which involve surrounding vital structures was decided not to proceed for excision in 2 cases. Overall Five-years survival rate was 93.5%. 2 patients of the series died due to dieases process as they were advanced malignant medistinal mass. Surgical treatment done by cardiothoracic surgeon for mediastinal mass specially involving surrounding structures though challenging, gives good outcome.
Mediastinal masses represent a vast group of tumours and pseudo-tumours which can involve the various compartments of the mediastinum.1 The most common mediastinal masses are neurogenic tumors (20% of mediastinal tumors), usually found in the posterior mediastinum, followed by thymoma (15-20%) located in the anterior mediastinum. Surgical removal of mediastinal masses usually gives good result.
A retrospective study was done from 6.8.2005 to 27.5.2014. Total 31 patients were included in this study. Age range was from 30 years to 70 years. Male was 18 and female was 13. Most of the tumour was thymoma (12 cases), thymoma with myasthenia gravis in 3 case, Thymic carcinoma 2 case, Nodular sclerosing Hodgkins lymphoma in 1 case, schawannoma in 2 cases, cystic mass in 5 cases, schawannoma with cystic degeneration in 1 case, fibromyxoma in 1 case, dermoid in 3 case, teratoma in 2 case, Fibrosing mediastinitis in thymic mass in 1 case, lymphoid hyperplasia in 1 case, malignant mesenchymal tumour in 1 case, myxoid liposarcoma in 1 case.
Symptomatically most common symptom was cough and chest pain. Second most common symptom was breathlessness and heaviness over the anterior chest wall. Other complains was intermittent fever, stabbing type of chest pain, difficulty in swallowing, dropping of upper eye lid ,weight loss ,anorexia, low grade fever, oral ulcer, swelling over lower part of the sternum. Double lumen endotrachieal tube intubation was used in all patients and fibreoptic bronchoscope was used. Surgical exposures varies from strenotomy (17 cases) to clamshell incision in 1 case to postero-lateral thoracotomy in 12 cases and antero ateral thoracotomy in 1 case. Superior Venacava was injured in 1 case, repaired successfully by 6/0 prolene controlled by partial clamp. Some of the medistinal mass needed careful dissection from lung, pleura, encircling distal aortic arch and proximal part of left subclavian artery, encircling left brachiocephalic vein.
1 case needed Reconstruction of sternum with prolene mesh, marsupialization was done in 2 cases, adjacent pleura, fatty tissue, part of pericardium was removed in 5 cases. Lobectomy was needed in 1 case. Extensive growth of the tumour which involve surrounding vital structures was decided not to proceed for excision in 2 cases. Different type of presentation was found during operation. Large cystic mediastinal tumour was adherent with lower part of left lung and pericardium, separated carefully. Bronchial cyst was found tightly adherent to surrounding structures, excised the roof and suck out the chocolate coloured thick secretion, marsopialization of exised border was done-kept the mouth wide open.
Thymic carcinoma was hard like stone adherent with the sternum, pericardium, left and right pleura, upper mediastinal surface of right lung, also encircling the left brachiocephalic vein, left lobe of the mass was removed totally along with the part of left pleura and pericardium-right lobe of the tumour was also removed as much as possible. Histopathologically was found epidermoid non keratinizing carcinoma.
Thymoma with Myaesthenia Gravis-total thymectomy along with removal of mediastinal fat, adjacent pleura, fatty tissue and small part of pericardium was removed. Large fibro sarcoma (8.5 kg)–malignant mesenchymal tumour, excision of 1-4 ribs posteriorly, partial removal of left scapula and partly left pleura was exised. Myxid liposarcoma-adherent to great vessels pleura, chest walls, lungs, diaphragm and heart-frozen section biopsy was down-malignancy-sample of tissue was then sent for histopathology. Clamshell-curvalinear bilateral sub mammary incision was performed extending from one mid axillary line to the opposite across the anterior aspect of chest, histopathologically found mature cystic teratoma-30x10x6 cm. Spindle cell thymoma exposed by anterolateral thoracotomy in 70 years old gentleman, very large tumour between upper and middle lobe of right lung and in front of helium of right lung, was firmly adherent to Supirior Venacava -small tear in Superior Venacava repaired by 6/0 prolene. Right mediastinal mass--FNAC showed benign cystic teratoma. During operation found inoperable--frozen section biopsy showed malignancy-further surgical procedure abandoned as it was densely adhernt to lung, pericardium and diaphragm (Figures 1-10).
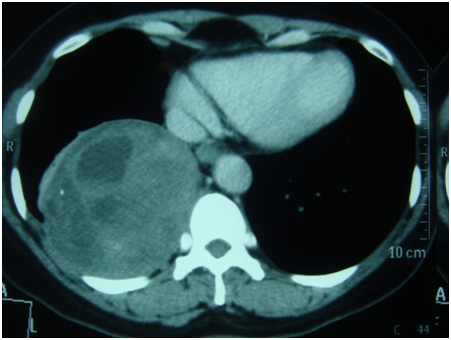
Figure 3 CT scan looks to be a complex hydrated cyst in posterobasal segment of right lower lobe-preoperatively found postero mediastinal cystic mass-histopathological examination showed schawannoma with cystic degeneration.
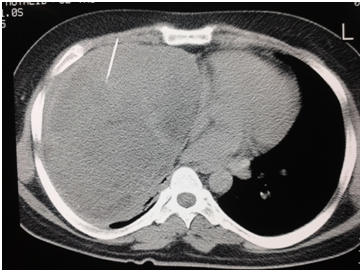
Figure 7 30 years gentle man:FNAC revealed Dermoid cyst, but peroperative frozen section biopsy showed myxoid liposarcoma.
Overall Five-year survival rate was 93.5%. In 1 case Recurrence of Fibrosing mediastinitis needed steroid therapy. 2 cases were inoperable and died due to diseases process as they were advanced malignant medistinal mass (fibro sarcoma and liposarcoma).
Tumors of the mediastinum represent a wide diversity of disease states. The location and composition of a mass is vital for differential diagnosis. The most common causes of an anterior mediastinal mass include the following: thymoma; teratoma; thyroid disease; and lymphoma. Masses of the middle mediastinum are typically congenital cysts, including foregut and pericardial cysts, while those that arise in the posterior mediastinum are often neurogenic tumors. The clinical sequelae of mediastinal masses can range from being asymptomatic to producing symptoms of cough, chest pain, and dyspnea.2 In our 31 patients locations of the tumour and presentation are same type. If left untreated, mediastinal tumors can cause serious health complications. As tumors grow, they will push against surrounding organs and tissues. Tumors that invade the heart or the vessels of the heart can cause death.
Tumors may also invade the spinal column. This may result in compression of the spinal cord. The location of tumors within the mediastinum varies according to the age of the patient. In children, tumors are commonly found in the posterior mediastinum. These mediastinal tumors often begin in the nerves and are typically benign. In adults, most mediastinal tumors occur in the anterior mediastinum and are generally malignant lymphomas or thymomas.3
Almost 40% of people who have mediastinal tumors experience no symptoms. Most of the growths are often discovered on a chest x-ray that is performed for another reason. When symptoms are present they are often a result of the compression of surrounding structures, such as the spinal cord, heart or the pericardium. Fine needle aspiration cytology is considered as adequate evaluation and when done under guidance of USG/ CT the results are very good. However core biopsies are preferable whenever lymphoma or thymoma is suspected.4
The tests most commonly used to diagnose and evaluate a mediastinal tumor include: Chest x-ray, Computed tomography (CT) scan of the chest or CT-guided needle biopsy surgical resection is the recommended treatment Extensive growth of the tumour which involve surrounding vital structures it was decided not to proceede for excision of tumour.5 While the determination for surgery is based on each patient’s particular medical situation, patients diagnosed with cancerous tumors or with tumors that are invading the area surrounding the mediastinum are most likely to be candidates for mediastinal surgery. Mediastinal tumors may reach large size before becoming symptomatic. Complete surgical excision (including adjacent invaded organs) mainly by open technique should be the rule for these patients as there is survival benefit.6 Complete excision was accomplished in all patients with benign lesions. Malignant lesions were usually partially resectable and carried a poor prognosis.7 2 patients in our study had poor outcome due to malignant medistinal mass (fibro sarcoma and liposarcoma).
Dr. Attawar Sandeep G, Dr. Muhammad Q. I. Talukder and Dr. Madhava Naik Janardhan.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.