Journal of
eISSN: 2373-4396


Migration of central line catheter into the heart is a rare complication. We present a case of Port-A-Cath migration in a patient who presented with history of trauma to the chest .It was confirmed by chest radiography and considered as the first reported Port-A-Cath from BARD disconnected from its septum, migrated into the heart and exposed bare to the right ventricle that was retrieved percutaneously using Trans-catheter loop-snare technique.
Keywords: port-a-cath migration, trans-catheter loop-snare technique, central venous line
Central line catheters are frequently used in patients who require long-term courses of intravenous infusions such as chemotherapy or parenteral nutrition. The most common complications of central line catheters include catheter malposition, pneumothorax, and hemorrhage and catheter embolization. Long-term complications include infections, thrombosis, extravasations, catheter disconnection and migration.1 We present a case of Port-A-Cath migration in a patient who presented with history of trauma to the chest.
Five year old boy, a known case of acute lymphoblastic leukemia (T cell ALL) has started to receive chemotherapy using a Port-A-Cath which was inserted surgically (BARDPORT®, 10.8mm diameter, USA) (Figure 1). A chest radiograph has documented the normal position of the Catheter postoperatively (Figure 2). The patient received regular courses of chemotherapy following catheter insertion with no encountered problems.
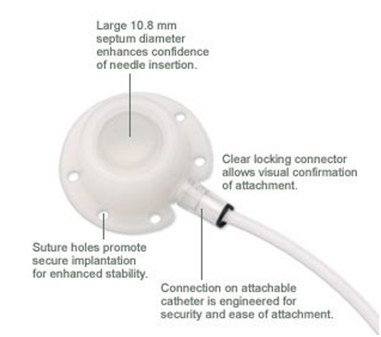
Figure 1 N=57; Epidemiological distribution of the pathological fractures, traumatic fractures, and nonunion.
Nine months later and during routine follow-up, the patient presented with a history of trauma to the chest at the site of the Port-A-Cath which was found non-functioning and a chest radiograph showed that the catheter had been disconnected from the injection port and migrated into the heart (Figure 3). The patient was asymptomatic, admitted to the hospital and was kept under close monitoring. Disconnection of the catheter was suggested, so surgical intervention was performed and the injection port was removed successfully but due to difficult access it was recommended to remove the catheter by percutaneous retrieval technique after discussion with interventional cardiologist.

Figure 3 Shows the whole length of Port-A-Cath disconnected from its septum & migrated into the heart making a large curve in the right ventricle.
The child was electively intubated and ventilated with general anesthesia. Initial attempts at snaring the Port-A-Cath through the right internal jugular vein were not successful (Figure 4). Therefore, the heart was accessed through the right femoral vein with 6F pediatric introducer sheath. Then 6F CORDIS MPA2 catheter was used to cross to the right ventricle outflow tract where the tip of the Port-A-Cath was located (Figure 5).
The Port-A-Cath was snared by 15mm loop (AMPLATZ GOOSE NECK). The snared Port-A-Cath could not be pulled into the MPA2 catheter. Consequently, both MPA2 catheter and snared Port-A-Cath were pulled through outside the heart with tight control on the snare to prevent it from slipping (Figure 6). There was no encountered resistance while pulling the Port-A-Cath, with stable hemodynamics. The child was extubated in the cardiac catheterization laboratory and recovered well from the procedure. A cardiothoracic surgeon has attended the operative theatre in case of any possible complication.
Central venous access devices are gaining much more importance in clinical medical practice for the infusion of antibiotics, cytotoxic drugs, blood products and parenteral nutrition. Due to the complication of many antineoplastic drugs being given by peripheral lines, recent technological advances facilitated the administration of these drugs via the central lines.2 Port-A-Cath is a totally implantable vascular access device which allows for infusion of drugs .It consists of two-part port system which are a separate catheter and a fixed chamber (injection port). Haindl3 reported that disconnection between the catheter and the port is most likely to result from the patient's body movement,3 the fact which is still not well recognized by most of the clinicians.4
Complications following venous port implantation include malposition, pneumothorax, hemorrhage, catheter embolization, infection, thrombosis, extravasation, and catheter fracture. A recent report of 1500 patients receiving a subcutaneously implanted venous access system revealed that only 13% had implant-related complications.5 Chia-Lo6 reported that although it is rare, catheter disconnection and cardiac migration are potentially dangerous complications with estimated frequency of 0.1% and had reported three cases of catheter disconnection after implantation of 1000 totally implantable venous devices.6
Port-A-Cath migration may be due to trauma at the site of the port, previous compression of the catheter with shoulder movements, repeated manipulation and vigorous injection of fluid into the port. In our study we report a rare complication of migrating central line most probably due to trauma at the site of the port followed by disconnection of the catheter from the injection port which may be attributed to week connection between both parts and inadequate securing of the catheter at the time of insertion. Frequent symptoms associated with catheter migration include neck pain, shoulder pain, chest pain, ear pain, palpitations. Many patients are asymptomatic probably because the usual site of migration is the right ventricle and pulmonary artery, and there are few sensory endings in the endocardium and vascular endothelium.7
Fortunately our patient was asymptomatic at the time when the catheter was found disconnected. In one case reported, interventional radiology attempted to retrieve the catheter through right femoral catheterization but this was unsuccessful, because of the vein occlusion. Further exploration revealed that left femoral as well as right and left internal jugular veins were also occluded. The Patient was then referred to cardiothoracic surgery. Under general anesthesia, a median sternotomy was made and the catheter was trapped 8. Another case was reported, presented with non-functioning line after 5months of insertion of Port-A-Cath and in this case the catheter was removed successfully by open neck surgery.9
To our knowledge, this is the first reported Port-A-Cath from BARD disconnected from its septum, migrated into the heart and exposed bare to the right ventricle that was retrieved percutaneously using snare following a difficult attempt to approach via the internal jugular vein or through an open neck surgery. There were concerns over the Port-A-Cath entanglement with the tricuspid valve or intraventricular structures during the process of pulling it uncovered. But probably the silastic nature of the Port-A-Cath makes it less likely to get entangled. Years of experience have proven that central venous catheters are superior to peripheral venous catheters for the delivery of chemotherapy. With such widespread use of this system, we should keep in mind all potential complications of the port system. Prevention and early detection are the cornerstone for the management of catheter disconnection and migration. The possibility of catheter disconnection should always be considered and a chest x-ray should be performed immediately. Moreover prevention should include instructing the patients to minimize heavy physical activities that involve the shoulder. To avoid open surgery, the percutaneous retrieval technique is preferred because it is simple, inexpensive and relatively low-risk.10
None.
Author declares there are no conflicts of interest.
None.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.