Journal of
eISSN: 2373-6437


Research Article Volume 14 Issue 2
Medical Radiologist, Private Banking Health Fund, Bolivia
Correspondence: Dr. Delia Maria Sánchez Argandoña, Medical Radiologist, Private Banking Health Fund, La Paz, Bolivia
Received: February 08, 2022 | Published: March 8, 2022
Citation: Argandoña DMS, Carrasco OV, Aliendre JGV. Update on the management of the polytraumatized patient: the role of fast and extended fast ultrasound in acute management diagnostic and therapeutic algorithm. J Anesth Crit Care Open Access. 2022;14(2):50‒57. DOI: 10.15406/jaccoa.2022.14.00506
FAST US (ultrasound) is specifically a ruler scan. The detection of abnormal intra-abdominal free fluid is a finding that can help the diagnosis. The absence of free fluid on US FAST does not mean that there is no free fluid; it simply means that free fluid has not been detected by US FAST. In this circumstance, clinical evaluation or other alternative investigative modalities should be considered. This review describes how to perform a US FAST or extended FAST exam, with examples of common pathologies. Benefits are highlighted, along with limitations and shortcomings.1
Ultrasound (US) has become the main tool for the management of patients with acute trauma in recent decades, to the point that it can almost be considered an extension of the physical examination performed in a first evaluation. US has been practiced for almost 40 years on the European continent, however it has taken a little longer to fully integrate into the UK and North America. While tomography (CT) is a standard of care, US performed by trained operators is an essential diagnostic tool for immediate use and low risk.2
It was not until the 1990s that focused abdominal ultrasound for trauma (FAST) was developed as the primary goal of detecting free fluid in patients with blunt abdominal trauma. The initial focus of the ultrasound examination was a single view: the hepatorenal fossa (Morison's space). However, it was soon realized that a more complete examination of the abdomen improved the detection of free fluid.3,4 In almost all recent studies on the use of ultrasound for the detection of free fluid in patients with blunt abdominal trauma, the specificity of ultrasound is high.4
Medical Specialist in Radiology. a) Caja de Salud de la Banca Privada and Caja Nacional de Salud b) Professor Emeritus of the Faculty of Medicine of the Universidad Mayor de San Andrés and Postgraduate Professor in Critical Medicine and Intensive Therapy c) Intensivist Physician Intensive Care Unit of the Caja Petrolera of Health and Trauma Center Hospital Corazón de Jesús.
Benefits of ultrasound
Trauma patients can potentially deteriorate rapidly. Any examination modality must provide useful information with a high degree of sensitivity and specificity in a short time, without increasing the risk for the patient. In this regard, US FAST meets all of these criteria. In the patient who has suffered a trauma, who is hypotensive, has suffered abdominal trauma or in those who cannot obtain precise data about their condition that can be provided by themselves or by third parties, a US FAST can be performed as an adjunct to circulatory evaluation.3
The current trauma management guidelines in their respective chapters of both the ATLS 2018 Edition (Advanced Trauma Life Support), like the European guidelines (STOP Bleeding), consider US as a high-level recommendation in the initial examination for the diagnosis of free fluid. US FAST detects free intra- abdominal fluid, and in this context, the premise is that free fluid represents hemorrhage and that, after trauma, fluid will collect due to gravity to an area and volume that are adequate for its detection. The amount of fluid that can be visualized depends on the rate of bleeding, the position of the patient, and the skill of the operator.
Clinical evaluation alone has low sensitivity; 20% to 43% of patients with significant abdominal trauma will initially show normality on physical examination. In contrast, US FAST has been shown to have a sensitivity of 86% to 99% and a specificity of 90% to 99% for detecting hemoperitoneum.4
FAST US and CT evaluation have replaced diagnostic peritoneal lavage (DPL) as the initial diagnostic method to detect intra -abdominal hemorrhage, although DPL still plays a role in the unstable patient.
Choice of transducer and configurations
A low frequency (2 – 5 MHz) convex transducer should be used. This provides the benefit of a wide field of view and the ability to potentially penetrate up to 20 cm into the abdomen (high depth), depending on the constitutional habit of the patient. As this transducer has low temporal resolution when examining in the subcostal cardiac position, it is suitable for the detection of pericardial fluid. Most US equipment will use the abdomen setting when this transducer is selected, but if not, this feature must be chosen by the operator. The significant adiposity of the abdominal wall produces attenuation of the US beam, so the gain of the deep planes must be increased, in order to be able to evaluate the intra- abdominal viscera.
Exam technique
US FAST comprises four views, each one seeks to detect the presence of abnormal intra -abdominal hypoechoic free fluid, whose presence may explain the clinical condition of a patient who has suffered trauma. The 4 positions can be performed in any order, but a complete scan must include evaluation in each of them. Conventionally the display marker represents the right side, so the transducer must also be used in that position. Additional scans or views extend the basic US FAST exam and make it E – FAST. These are essentially views of the lower chest to look for signs indicating intrathoracic hemorrhage (Figure 1).
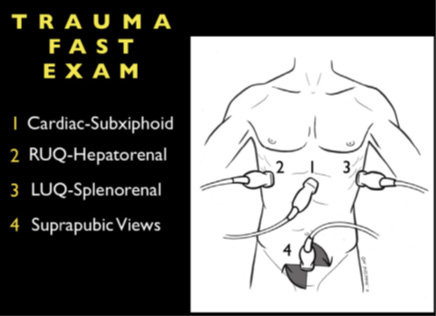
Figure 1 The 4 basic windows of the abdominal FAST exam: 1. Subxiphoid 2.
Hepatorenal 3. Renal splenus 4. Supra pubic.
Upper right quadrant
Free intra- abdominal fluid collects between the liver and the right kidney, a space known as the hepatorenal flexure or Morrison's space, and this is where this part of the exam focuses. The US transducer should be located in the midaxillary line, between the 11th and 12th ribs in the coronal plane, rotate the transducer slowly toward the plane of the kidney (the lower pole of the kidney is slightly anterior), and then tilt the transducer into the retroperitoneum (Figure 2).

Figure 2 Placement of the transducer with the marker towards the head to
visualize the hepato-renal space.
Once this view has been obtained, the transducer should be moved perpendicular and parallel to the ribs to view the entire hepatorenal space. If adequate visibility is not obtained in this orientation, the transducer should be moved anteromedially or to the transabdominal orientation, with the US beam pointing laterally.
How posteriorly one needs to scan to adequately visualize the kidneys (retroperitoneal organ) is often underestimated. Primarily liver trauma can be detected with lacerations, which can be seen with hematoma formation or hypoechoic abnormalities within the liver parenchyma. Hematomas may be visualized as confined and contained by the liver capsule or extending into the peritoneal cavity. Fluid in the pleural cavity can also be detected from this position and can be seen as hypoechoic areas between the right lung and the liver (with the diaphragm above it) (Figure 3).
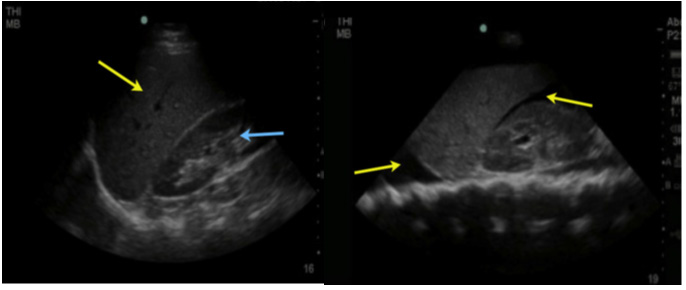
Figure 3A Figure 3B
Figure 3A Hepato -renal space without free fluid and in 3B: Presence of free fluid in the hepato-renal space (Morrison) Hypoechoic image surrounding the kidney and liver and above the diaphragm corresponding to hemothorax.
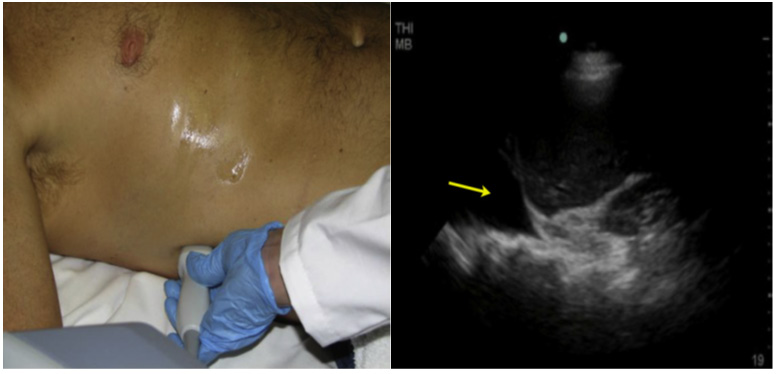
Figure 4A Placement of the sector probe with the mark towards the head to assess fluid above the diaphragm. 4B. Presence of anechogenic image above the diaphragm, which corresponds to hemothorax in the context of trauma.
Upper left quadrant
Fluid can collect in the space between the spleen and the left kidney, the splenorenal flexure, similarly to the right side, settling between the 2 organs. Its exploration is similar to that of the right side, except for the higher and posterior location of the left kidney due to the little displacement produced by the spleen, for this reason visualization is more difficult due to the acoustic shadows produced by the ribs and requires that the evaluation be performed during the patient's inspiration, without forgetting that the transducer must be in a more posterior position (Figure 5 A and B). A complete evaluation should include the space between the spleen and the left kidney in its entirety to look for free fluid. Contrary to the evaluation of the right side, it is very common for the fluid to be located between the spleen and the diaphragm, so this area should also be examined.
Splenic renal fossa; examination with a low-frequency transducer with a cephalad marker: it allows us to observe: splenic renal fossa and infradiaphragmatic space.
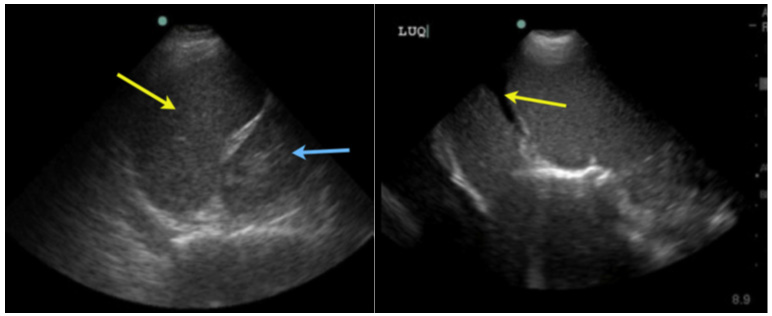
Figure 5A. Figure 5B.
Figure 5A Free renal splenic space (light blue arrow: left kidney, yellow
arrow spleen; 5B. Anechoic image in (yellow arrow) corresponding to intraabdominal
free fluid.
Damage to the spleen can also be detected and appear similar to damage to the liver.
Fluid in the pleural cavity can also be seen in the left lung base, and will be seen as a hypoechoic area over the spleen and diaphragm.
Pelvic position
The transducer should be placed in a transverse orientation (the mark on the right) just above the pubic symphysis. The US beam should be angled inferiorly within the pelvis to demonstrate the bladder, rectum and the space between them, the rectus vesical fornix, or the fornix of Douglas (Figure 6B). This is the lowest portion of the pelvis in which the fluid collects, having traveled through both paracolic grooves, and is seen as a hypoechoic area between the bladder and rectum on US.
The transducer is rotated to the sagittal plane, and the US beam must be moved sagittally to examine all of these areas for free fluid. Visualization is best with the bladder fully distended with urine, which provides an acoustic window to the rest of the pelvis.
In male patients, fluid can also be found lateral to the prostate, superior to the seminal vesicles and bladder wall. (Figure 6A).
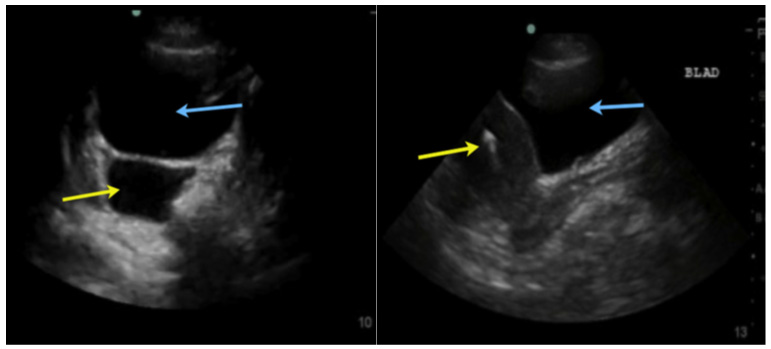
Figure 6A Retrovesical space in the male with free fluid: Bladder blue arrow, free fluid yellow arrow.
Figure 6B Vesicouterine space without free fluid Blue arrow: bladder; uterus yellow arrow.
In female patients, the fluid can also be visualized superior and posterior to the uterus, also superior to the bladder. Of note, the rectovesical space in women extends deeper into the pelvis compared to men. Finally, one should always look for the presence of a fetus in the womb.
Subxiphoid or subcostal position
The transducer is located below the xiphoid process, almost parallel to the abdominal wall to observe the content of the mediastinum through the left hepatic lobe. The transducer needs to be angled slightly to the patient's left. In this position, the fluid in the pericardial sac around the heart can be clearly seen as a hypoechoic ring (Figure 7).

Figure 7 Subxiphoid window: sectoral transducer, in the lower portion of the xiphoid process, directing towards the patient’s left shoulder.
The effect of fluid on the right ventricle can be seen, although temporal resolution is slow, unless an echocardiographic transducer is used, signs of ventricular compromise can confirm a clinical diagnosis of cardiac tamponade (Figure 7A).
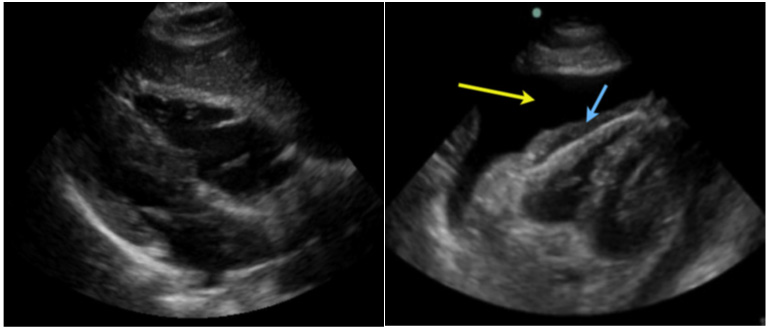
Figure 7A Anechoic image (*) that occupies the pericardium is evidenced, in a patient with closed chest trauma.
More recently, ultrasound has also been shown to be useful in diagnosing pericardial effusions in trauma patients.
The main reason for diagnosing pericardial effusions is to prevent trauma-induced patients from developing pericardial tamponade.
We incorporate the subcostal view of the heart as a part of the rapid examination in all patients with blunt abdominal trauma. This is useful in diagnosing pericardial effusions (Figure 7A).
Fast E (Extended) chest
Chest ultrasound has been shown to detect pleural effusions. In trauma patients, additionally ultrasound can be used to diagnose pneumothorax or free fluid within the chest in the setting of hemothorax trauma.
More recently, ultrasonography has also been shown to be useful in the diagnosis of pneumothorax. The parietal pleura adheres to the internal muscle of the thorax, while the visceral pleura adheres to the lung.6
During inspiration and expiration, the visceral pleura back and forth adjacent to the parietal pleural '' moves'' which is known as pulmonary sliding. The hyperechoic bright line represents the junction of the visceral pleural with the parietal pleura, which adheres to the lung as it moves and slides during normal inspiration and expiration, is seen on real-time ultrasound and is a normal finding (Figure 8). The absence of the sliding lung is a direct sign of pneumothorax, but not conclusive, the cardinal sign being the lung point that represents the transition between viable lung and pneumothorax.
Anterior chest
To complete the E–FAST exam, the chest is scanned anteriorly and bilaterally to exclude the presence of pneumothorax and hemothorax. Depending on the patient's body habitus, better resolution is obtained for this evaluation using a high-frequency, shallow-depth linear transducer (10 MHz linear probe) in the case of pneumothorax; and the convex or sector transducer (which have a lower frequency between 3-5 MHz and greater depth) to track hemothorax.
Placement of the linear transducer in the region of the anterior thorax between the 2nd and 3rd intercostal space in the midclavicular line (pneumothorax evaluation).
Both lungs are evaluated for the presence of lung sliding (lung sliding) whose presence rules out the presence of pneumothorax.6 To confirm the diagnosis of pneumothorax by moving the probe both inferiorly and laterally with the notch directed towards the head, looking for the pulmonary point sign that is pathognomonic of pneumothorax, which represents the transition point between the pulmonary parenchyma and air in the pleural cavity (pneumothorax), is seen depicted in B-mode; alternating pulmonary slippage with its absence; and in M mode interspersed as beach and stratosphere signs.
Also in M-mode, look for the beach sign (absent in pneumothorax) and the stratosphere sign found in pneumothorax.
US signs in pneumothorax: absence of pulmonary sliding, pulmonary dot sign, stratosphere sign, or barcode.
US signs that rule out pneumothorax: presence of B lines, presence of pulmonary sliding, beach sign.
In B-mode; Presence of normal lung slip (lung sliding); Yellow arrow pleural movement (visceral and parietal) and in blue date vertical lines in comet tails.
In M-mode; Sign of the Beach Blue arrow the waves of the sea: Corresponds to soft parts and in yellow the sand: corresponds to normal lung tissue.
In M-mode; Sign of the Stratosphere or Code of bars, corresponds to pneumothorax.
Hemothorax evaluation
When there is fluid in the pleural cavity (in the context of hemothorax trauma) an evaluation of the diaphragm can be performed (in the absence of fluid and in the presence of a fully aerated lung, the diaphragm is excluded and cannot be seen except for its lateral insertion). In this position, the detection of fluid is sensitive, managing to observe levels below 20-50 ml in some studies, and its presence provides the diagnosis of intrathoracic trauma with pleural hemorrhage.
Pleural effusion
The study, quantification and guidance for the thoracocentesis of pleural effusions are the oldest and most well-known applications of lung ultrasound due to the great sensitivity of ultrasound to detect small amounts of fluid at the pleural level with a diagnostic capacity superior to chest radiography. chest and very close to the tomography. This makes it an essential tool for making the definitive diagnosis of pleural effusion, allowing its differential diagnosis with that of atelectasis, which although a priori seems easy, it is not always so in an environment such as critical care areas where the patient cannot move. , the examination is limited and plain radiographs in recumbency are of poor quality. For the ultrasound study of pleural effusion, the following points must be taken into account:7
Errors and limitations
The absence of detectable free fluid does not indicate the absence of hemorrhage, similarly, not all free fluid that is detected is hemorrhage. Free intraperitoneal fluid can also be urine (bladder rupture), ascites (due to pre-existing comorbidity), fluid from a ruptured cyst (for example of ovarian origin), intestinal content (due to perforation or rupture), or amniotic fluid (in a pregnant trauma victim).
It is normal for some women during menstruation to have free intraperitoneal fluid.
Pleural fluid detected on an E-FAST exam may also represent the finding of pre-existing disease (exudate or transudate pleural effusion).
Any fluid that is detected should always be considered in the clinical context. In the right upper quadrant, the gallbladder, hepatic flexure of the colon, inferior vena cava, and hepatic veins may be mistaken for free fluid in the hands of an inexperienced operator. In the left upper quadrant, a completely fluid-filled stomach may appear to be free fluid, so care must be taken when describing fluid boundaries. Obtaining the subxiphoid view can be particularly challenging in the obese patient post-cardiac surgery or post-abdominal surgery. An air-distended stomach after air mask ventilation can cause significant difficulty in this view, as does the presence of intraperitoneal air.
Under these circumstances, formal echocardiography should be performed, the long axis being particularly useful. Epicardial fat can be confused with pericardial fluid, however it is usually not anechogenic and is usually only seen anterior to the right ventricle.
Limitations of ECO FAST
Patients with pre-existing ascites, iatrogenic free fluid (example patient on peritoneal dialysis), in women of childbearing age a small amount of free fluid could be found in the pelvic region, when the bladder is completely filled , detection of free fluid is that bruising may appear echogenic. Finally, there is often no free fluid associated with contained lesions of solid organs, such as the liver, spleen, or kidney.
Key points
The US FAST and E – FAST is an important tool for the patient who has suffered trauma. The extent of the physical examination should be considered, and when integrated with it, its speed and ability to detect the consequences of blunt or penetrating abdominal trauma has proven to reduce the time for admission to surgery and improve the survival prognosis.
We present a proposal for an algorithm, diagnosis and treatment of abdominal trauma that will be very useful in the Emergency and Intensive Care services.
|
Diagnostic peritoneal lavage |
|
|
Advantages |
Disadvantages |
|
Can be performed at the patient's side |
invasive |
|
can be done quickly |
Difficult in pregnancy or with many previous surgeries |
|
Highly sensitive for identifying intraperitoneal blood (approximately 20 mL with 100,000 red blood cells/mL) |
cannot be repeated |
|
|
Too sensitive, can lead to high laparotomy rate |
|
Tomography |
|
|
Advantages |
Disadvantages |
|
retroperitoneum damage |
It takes 30 – 60 minutes to complete the study |
|
Properly identifies specific injuries |
Requires a stable patient due to the relative isolation in the CT room |
|
High sensitivity and specificity |
|
|
It can detect free liquid greater than or equal to 100 – 250 m. |
|
|
US FAST |
|
|
Advantages |
Disadvantages |
|
Can be done quickly (< 3 minutes) |
dependent operator |
|
non-invasive hemodynamically unstable patients. |
Low detection of damage to hollow viscera or retroperitoneum |
|
Can be repeated (does not produce ionizing radiation) |
Obesity or subcutaneous air may make examination difficult |
|
Sensitive and specific for free fluid similar to diagnostic peritoneal lavage and CT |
May not detect injury to specific organs causing bleeding |
|
It can detect free liquid greater than or equal to 100 – 250 m. |
|
Table
Advantages and Disadvantages of FAST Ultrasonography compared to other complementary imaging methods.

©2022 Argandoña, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.