Journal of
eISSN: 2373-6437


Review Article Volume 12 Issue 4
1Anesthesia and Critical Care Medicine Lotus Med Group Tijuana BC, México
2Plastic Surgeon Lotus Med Group Tijuana BC, México
3Anesthesia resident Centro Médico Nacional Siglo XXI Instituto Mexicano del Seguro Social México City
4Anesthesia Grupo Multidisciplinario Clincob Villahermosa Tabasco, México
Correspondence: Víctor M. Whizar-Lugo, Anesthesia and Critical Care Medicine, Lotus Med Group Tijuana BC, México
Received: August 28, 2020 | Published: September 19, 2020
Citation: Whizar-Lugo VM, Campos-León J, Íñiguez-López KL, et al. Update on anesthesia for patients undergoing post-bariatric body contouring surgical procedures. J Anesth Crit Care Open Access. 2020;12(4):143-151. DOI: 10.15406/jaccoa.2020.12.00450
Individuals who have undergone bariatric surgery and have lost a considerable amount of weight tend to seek consultation with plastic surgeons for body contouring surgery. This growing population is overweight, and they still have some of the co-morbidities of obesity, such as hypertension, ischemic heart disease, pulmonary hypertension, sleep apnea, iron deficiency anemia, hyperglycemia, among other pathologies. They should be considered as high anesthetic risk and therefore, should be thoroughly evaluated. If more than one surgery is planned, a safe operative plan must be defined. The anesthetic management is adjusted to the physical condition of the patient, the anatomical and physiological changes, the psychological condition, as well as the surgical plan. Anemia is a frequent complication of obesity and bariatric procedures and should be compensated with appropriate anticipation. Pre-anesthetic medications may include benzodiazepines, alpha-2 agonists, anti-emetics, antibiotics, and pre-emptive analgesics. Regional anesthesia should be used whenever possible, especially subarachnoid blockade, since it has few side effects. General anesthesia should be left as the last option and can be combined with regional techniques. It is prudent to use conscious sedation for facial and neck surgery, maintaining strict control, especially with respect to the airway management. Thromboprophylaxis is mandatory and should continue for several days after the operation.
Keywords: Post-bariatric, plastic surgery, body contouring, anesthesia
Medical and surgical weight reduction programs for morbidly obese patients have proliferated rapidly. Consequently, a new type of patient has emerged and become a challenge for the anesthesiologist, yet has received little attention in the contemporary literature. This special group of patients with exaggerated weight loss in relatively short periods of time seeks the help of plastic reconstructive surgeons to improve their deteriorated and at times grotesque body image. Body contour surgery should be deferred at least one year after stabilization of weight loss to allow improvement or cure of co-morbidities and maximum skin contracture.1 About 84.5% of patients losing weight through gastric bypass request body contour surgery. The majority of these patients are young, divorced females.2 A study by Gusenff3 showed that only 11% of gastric bypass patients underwent plastic surgery, of which 47% underwent multiple surgeries. Certain socioeconomic factors appear to be responsible for the lower incidence of body contour surgery in this group of patients.
The body dimorphisms suffered by these patients are related to redundancy of loose, amorphous excess skin as well as subdermal fat accumulation in such areas as the face, neck, breasts, torso, abdomen, pelvis, gluteus, and extremities. The folds of excess skin become damaged by intertrigo, hyperkeratosis, mycosis, acanthosis nigricans and cellulitis. These body changes interfere with daily activities, provoke isolating behaviors and frequently cause awkwardness in their sexual relationships. These changes negatively impact the patient’s quality of life and, if appropriate management is not instituted, they may fall into old behaviors which will lead them back to extreme or morbid obesity, a vicious cycle characteristic in such patients.
When these patients undergo body contour surgery, their lives change significantly: better personal, social and cultural adaptation, increased productivity and changes in their state of health.4–6 Body contouring surgery could be associated with better maintenance of weight loss.7
Aesthetic and reconstructive surgical options available to patients with massive weight loss are multiple and diverse, and can be tailored to each person in the same way that a dress or suit is tailored to one’s exact measurements. Surgical solutions are not similar to conventional plastic surgery, where interventions are directed to specific zones. In patients with maximum weight loss, the goal is to design a new body contour in such a way as to drastically improve their image.
Some of the pathologies associated with morbid obesity are not resolved through simple weight loss; on the contrary, some of them, such as inadequate nutrition and anemia, tend to persist or even be exacerbated, which places patients at increased anesthetic and surgical risk. Persons with massive weight loss should therefore be approached with the co-morbidities of morbidly obese patients.8
Obesity and overweight are defined as an abnormal or excessive accumulation of fat tissue that may be hazardous to the individual’s health. It is treated as a chronic illness caused by multiple factors which are associated with premature death due to multiple systemic pathologies. The World Health Organization (WHO) defines overweight as a body mass index (BMI) between 26 and 29, and obesity as a BMI above 30. When the BMI is between 30 and 39 it is called simple obesity. A BMI between 40 and 49, or above 35 with a comorbid condition, it is known as morbid obesity. When the BMI exceeds 50 it is known as super obesity.
BMI, calculated by dividing the individual’s weight in kilograms by the square of their height in meters. BMI is a simple indicator of the relationship between the weight and the height that is used to identify overweight and obesity in adults, among individuals as well as in populations. The WHO has mentioned that in 2016 more than 1.9 billion adults aged 18 years and older were overweight. Of these persons, over 650 million adults were obese. 39% of adults aged 18 years and over (39% of men and 40% of women) were overweight. Overall, about 13% of the world’s adult population (11% of men and 15% of women) were obese in 2016. Obesity also affects children; 41 million children under 5 years were overweight in 2016.9
The worldwide prevalence of obesity nearly tripled between 1975 and 2016. This pandemic is not limited to first world countries, and is proliferating in countries with limited resources, especially in urban settings. Mexico has the second highest incidence, exceeded only by the United States (OECD Health Data 2017) with 70.8 million people suffering the effects of overweight and obesity in both countries. This means that one in three Mexicans is overweight or obese, of which 5 million are adolescents. The condition also affects those over 60 years of age, among which population the incidence of obesity is 60%.10 Just as in other countries, in Mexico large cities do not have a monopoly on obesity, it has been found among indigenous groups living in impoverished conditions.11,12
Anatomic and physiologic changes in obese individuals. Obesity, especially morbid or super obesity, involves diverse organs and systems, in such a way as to represent a complex pathological entity that challenges anesthetic and surgical procedures. The pulmonary, cardiovascular, gastrointestinal and metabolic changes are by far the factors that most increase the surgical and anesthetic risks. Other changes involve the airway and the propensity for venous thrombosis and, therefore, the risk of embolism and death. Table 1 lists some of the pathologies associated with or facilitated by excess weight.
|
Insulin resistance, type 2 diabetes mellitus, metabolic syndrome |
Colon, endometrial, renal, gallbladder cancers |
|
Hyperlipidemia |
Infertility, menstrual changes |
|
Coronary artery disease |
Complications of pregnancy |
|
Arterial hypertension |
Gallstones |
|
Congestive heart failure |
Gastroesophageal reflux |
|
Pulmonary hypertension |
Nonalcoholic fatty liver disease |
|
Cerebrovascular disease |
Osteoarthritis |
|
Obstructive sleep apnea |
Urinary incontinence |
|
Hyperuricemia, gout |
Depression |
|
Premature death |
Sarcopenia |
Table 1 Pathology associated with obesity
Because of its importance, some changes of obesity are described, especially those alterations that do not recover quickly after bariatric surgery, or those changes secondary to the restrictive and malabsorptive nature of the various bariatric procedures and that could have harmful perioperative effects.
Nutritional and endocrine changes. The nutritional and endocrinological changes of obesity are well known. Multiple deficiencies of vitamins, minerals and trace elements have been studied. Some results are still controversial and require more research. Lewis et al published a systematic review on vitamins deficits,13 and contrary to what was expected, they did not find evidence of deficiencies of vitamin A, B1, C or E. Patients with gastric bypass have a reduced gastric capacity, with diminished intestinal absorption, and suffer from iron, folate and B12 deficiencies. A study of 30 Mexican patients taking multivitamin supplements found that 54.5% still had iron deficiency, 27.3% had cobalamin deficiency and 63.6% had anemia 3 years after Roux-Y gastric bypass.14
Other metabolic deficiencies found in bypass patients include vitamin A (11%), vitamin C (34.6%), 25-OH vitamin D (7%) and vitamin B6 (17.6%).15 It is well known that Roux-en-Y gastric bypass and biliopancreatic diversion with duodenal switch, produce substantive changes in the bone metabolism that finally induce a high risk of fractures. There is a pronounced deterioration in bone mass at the axial skeleton, as well as at the appendicular skeleton, resulting in a detrimental effect on trabecular and cortical microarchitecture and estimated bone strength. These bones modifications appear early and continue even after weight loss plateaus and weight stabilizes. Apparently, these skeletal effects of bariatric surgery are presumably multifactorial, and mechanisms may involve nutritional factors, mechanical unloading, hormonal causes, and changes in body composition and bone marrow fat. There are no data on the long term skeletal changes due to the sleeve gastrectomy.16–18 It is also important to mention that obesity is accompanied by a decrease in skeletal muscle mass and function (sarcopenia). 25-hydroxyvitamin D is low in obese patients compared to normal weight subjects. A recent study found that 25-hydroxyvitamin D level is inversely correlated with percentage of fat mass, but cholecalciferol supplementation had no effect on percentage fat mass.19
There is peripheral insulin resistance, as well as diminished concentrations of growth hormone, lower testosterone levels, changes in ovarian cycles and early menopause. Hypothyroidism must be evaluated as a cause of overweight and be meticulously considered after weight reduction surgery as it may interfere with anesthesia/body contouring surgery. Guan et al.20 reviewed 24 publications on the effect of bariatric surgery on thyroid function and found a significant decrease in TSH, FT3 and T3 without significant change in the levels of FT4, T4 and rT3. These authors mention that bariatric surgery had a favorable effect on overt and subclinical hypothyroidism, with a reduction in thyroid hormone requirements after the operation. Another study found decrease of TSH 12 months after bariatric surgery.21
Cardiovascular and pulmonary changes. Obesity is a risk factor for cardiovascular diseases. The common co-morbidities such as arterial hypertension, deep vein thrombosis (DVT), pulmonary embolism (PE), diabetes mellitus and hyperlipidemia, further increase this risk. Obesity-hypoventilation syndrome, which in its most drastic presentation is known as Pickwick’s syndrome, is present in 10% of extremely obese patients. It involves carbon dioxide retention, hypoxemia and may be associated with pulmonary hypertension and right heart failure secondary to increased right ventricular afterload. Fortunately, the majority of obese patients with massive weight loss improve these cardiopulmonary conditions. There is a tendency toward cardiac rhythm changes, probably facilitated by such diverse factors as cardiac hypertrophy, hypoxemia, hypokalemia (due to the use of diuretics), coronary artery disease and a hyper adrenergic state.
Changes in pulmonary function are attributed to an increased intraabdominal pressure, as well as the mechanical effects of excess weight of the thoracic wall, resulting in reduced vital capacity, inspiratory capacity, total lung volume and functional residual capacity.22 These changes are accompanied by closure of small airways and changes in ventilation/perfusion. There are increased metabolic demands due to an excess of metabolically active adipose tissue, and an increase in the consumption of oxygen as well as the production of CO2. This means they require a greater minute ventilation, which may further increase oxygen consumption. A reduced functional residual capacity, in conjunction with an elevated rate of oxygen consumption, results in reduced time to desaturation during apnea produced during anesthetic induction and endotracheal intubation. Obstructive apnea is a sine qua non condition of super morbid obesity, although it can also occur in subjects without overweight. The development of apnea results from the complex dynamic interaction between anatomical risk factors and compensatory neuromuscular reflexes.23 It has been found that bariatric surgery significantly improves obstructive sleep apnea (OSA); the mean apnea-hypopnea index before surgery was 40 events per hour and seven events per hour after surgery (mean reduction 80%, P 0.004), There was also an improvement in oxygen saturation (SpO2) before and after surgery (90% and 94% respectively, P 0.008).24 The systematic review done by Quintas-Neves and co-workers25 analyzed apnea-hypopnea index, apnea index and respiratory disturbance index and found improvement of these OSA severity parameters 1 to 2 years after the bariatric surgery. The interventions with a combined malabsorptive and restrictive mechanism, like Roux-en-Y gastric bypass, were more efficient in resolving and improving OSA than merely restrictive ones, like laparoscopic adjustable gastric banding. Another study found that OSA improvement does not always occur after laparoscopic Roux-en-Y gastric bypass, around three quarters of the moderate to severe OSA patients had no or mild OSA, whereas one quarter (25.9%) still had moderate to severe OSA. Age≥50 years, preoperative apnea-hypopnea index ≥30/hr, excess weight loss <60%, and hypertension were predictive factors for this persistent postoperative apnea-hypopnea index AHI≥15/hr.26 In agreement with these data, all exobesic patients who underwent bariatric surgery requiring body contour surgery should be evaluated and treated according to the preoperative guidelines of people with OSA.
Esophageal and gastrointestinal modifications. There is a decrease of the esophageal and gastric peristalsis as well as impairment of lower esophageal sphincter relaxation. Patients with gastric sleeve or bypass have a reduced gastric capacity.27 These alterations can facilitate gastroesophageal regurgitation and bronchial aspiration during general anesthesia or i.v. sedation, and produce aspiration pneumonia. Patients with gastric banding tend to regurgitate more frequently. Jean et al.28 compared patients with laparoscopic adjustable gastric banding or Mason's vertical gastroplasty (n 66) vs a control group (n 132) and found that pulmonary aspiration was significantly higher (P<0.006) in the postbariatric group (4 patients: 6%) than in the nonbariatric group (0 patient). When this factor is combined with difficult intubation, anesthetic induction becomes a very high risk.
Kidney and liver function. Obesity favors chronic glomerulopathy which is independent of dyslipidemia, diabetes and hypertension related to obesity. It occurs with early stages of glomerular hypertrophy with or without secondary segmental focal glomerulosclerosis, and is characterized by an abnormal glomerular filtration rate, that are often not diagnosed.29 Although there is controversy, bariatric surgery seems to improve renal function reversing glomerular hyperfiltration rate and albuminuria. This improvement in renal function occurs six months or more after any type of bariatric surgery.30,31
75% up to 100% of the morbidly obese population have non-alcoholic fatty liver disease and 33% have nonalcoholic steatohepatitis. The Roux-en-Y gastric bypass and sleeve gastrectomy significantly improve liver alterations, although there is a worse glycemic control.32,33
Bariatric surgery should be considered in the following three situations adults with BMI ≥40, adults with BMI ≥35 who have obesity related co-morbid conditions and are motivated to lose weight but have not responded to behavioral treatment, with or without pharmacotherapy, to achieve sufficient weight loss for target health goals, and adults with BMI 30-34.9 with diabetes or metabolic syndrome (evidence for this recommendation is limited).34 The procedures of bariatric surgery have gradually evolved; from the initial metabolic surgery attributed to Kremen in 1954, the first gastric bypass in 1967 to the gastric sleeve; the surgery most used currently.35 Bariatric surgery improves many of the functional, anatomical and metabolic alterations, as well as improving the quality of life.36–38 Although the long-term results are variable and not conclusive, it has been mentioned that all types of bariatric surgery reduce weight, BMI and various co-morbidities better than medical procedures to lose weight. When compared to each other, some surgeries resulted in greater weight loss and improvement of co-morbidities than others. The results were similar between Roux-en-Y gastric bypass and sleeve gastrectomy, and both procedures had better results than adjustable gastric bands. For people with a very high BMI, biliopancreatic diversion with duodenal switch resulted in greater weight loss than Roux-en-Y gastric bypass. The duodenojejunal bypass with sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass had similar results. Isolated sleeve gastrectomy produced better weight loss than adjustable gastric banding after three years of follow-up. The results related to weight loss were similar between laparoscopic gastric imbrication and laparoscopic sleeve gastrectomy in one trial. In all studies, the rates of adverse events and reoperation rates were generally poorly reported.37
Patients who have undergone bariatric surgery often seek consultation with plastic surgeons with the goal of rebuilding their body contour, recover self-esteem, and to improve psychosocial function (4-7). Regions such as the face, neck, arms, breasts, abdomen, buttocks and thighs look grotesque as seen in figure 1 and 2. Of 37,806 who had bariatric surgery, 5.58% underwent body contouring surgery. In this study, the average time of plastic surgery after the band, bypass or sleeve was 1134.83 ± 671.09, 984.70 ± 570.53 and 903.02 ± 497.31 days, respectively (P <0.0001).39 These patients have deformations that often require more than two surgeries since their skin looks suspended with adipose panicles that sometimes favor bacterial or fungal infections. Due to chronic overweight the skin has lost its elastic capacity and does not retract after considerable weight loss (Figure 1,2).40
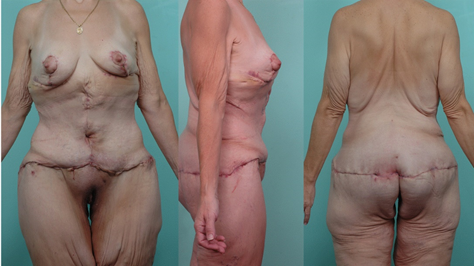
Figure 2 Changes after surgery of the body contour: mammoplasty, liposuction and circumferential abdominoplasty with anchor technique or "Fleur de Lys" performed in a single surgical time. The images correspond to the patient of figure 1.
All alterations and changes secondary to obesity and those that happen after bariatric surgery must be meticulously studied before planning body contouring surgeries. For example; antihypertensive, hypoglycemic, lipid-lowering drugs should be adjusted, although some patients will benefit if they continue taking statins. The aforementioned deficiencies of micronutrients should be corrected according to established guidelines, especially the anemic syndrome. Keep in mind OSA, pulmonary hypertension, cardiac ischemia, dumping syndrome, the possibility of fractures due to osteoporosis, and so on.
Although the combination of two or more surgeries of the body contour is not ideal, when multiple combinations are planned (mommy makeover) they must be performed under strict safety protocols to avoid complications.8,41
It has been found that body contour surgery favors better control of the weight of people who previously had undergone bariatric surgery, especially after Roux-en-Y gastric bypass.7,42,43 It is possible that a better corporal aspect and psychological improvement are factors that stimulate patients to continue with adequate diets to lose more weight.
The surgical procedures that people with massive weight loss need are many and generally are performed over several surgical interventions, with prolonged surgical times and in unusual surgical positions which may compromise blood supply and/or innervation to certain regions. In addition to the changes described in previous paragraphs, these factors alone are reason enough to consider increased risk when compared to healthy patients undergoing aesthetic procedures. Table 2 lists the more common procedures.
|
Surgery |
Brief Description |
|
Abdominoplasty / Belt lipectomy |
Surgical resection of excess skin and abdominal fat. It may be limited to the anterior abdominal wall, extend to the flanks or be circumferential. |
|
Lower body lift |
A modified abdominoplasty that extends up to T6 and occasionally includes liposuction |
|
Thigh lift |
Skin resection with or without liposuction, with regional pexia |
|
Breast lift or mastopexy |
Resection of excess tissue with relocation of nipple |
|
Torsoplasty |
Resection of excess skin of the upper back and sub axillary region |
|
Gluteus |
This region begins at the iliac crests. Pexia is performed with or without autologous fat injection |
|
Arm lift or brachioplasty |
Resection of excess tissue with or without liposuction. Usually encompasses the upper arm but may include the whole limb. |
|
Face, neck, forehead |
Face lift |
|
Liposuction |
Percutaneous extraction of fat. Ultrasound or laser may be used as adjunct. It is a complementary procedure during other surgeries and in rare occasions is the only surgery in the previously obese patient. |
Table 2 Reconstructive plastic surgical procedures
It is advisable to establish a surgical plan according to the physical conditions of each patient, their aesthetic goals and the achievable surgical possibilities, as well as the physical constraints of the surgical center and the abilities of the surgical team. Some patients should be handled in the hospital rather than an outpatient surgical center or short term surgical clinic. This point is frequently undervalued by the surgical team as well as the patients. Figures 2-4 show body contouring surgeries that are frequent in patients with massive weight loss.
Brachioplasty with surgical reduction and mastopexy is a frequent surgical combination that can be executed either with general anesthesia or a cervicothoracic block. In our practice, this type of patient is managed with balanced general anesthesia. The lift of the thighs, is an intervention with an intermediate surgical time that we usually manage with subarachnoid anesthesia using hyperbaric bupivacaine or ropivacaine, combined with clonidine. We consider these cases as high risk since the patients usually have multiple co-morbid conditions (especially lower limb venous insufficiency), surgical times are prolonged with significant bleeding. The procedure also requires placing the patient in the prone position for a long period of time.
Patients who underwent bariatric surgery and later seek plastic procedures are more tolerant than non-obese people, since their dimorphisms are more difficult to resolve and they are willing to accept that surgeries should be fractionated and scheduled over time, which guarantees greater safety and better aesthetic results. Their evaluation and management should be complete, involving various specialists. When evaluating these patients, it is important to remember that, while one group of patients will experience improvement or even resolution of the co-morbid conditions that accompany obesity,44 a variable percentage will continue to suffer the consequences of some co-morbidities, as well as the side effects associated with bariatric surgery. One study of 152 French patients subjected to gastric banding, in whom the BMI dropped from 44.3 to 29.6, showed that diabetes mellitus remitted in 71%, arterial hypertension remitted in 33%, and sleep apnea in 95% of cases.45 The most important co-morbidities that should be studied in previously obese patients undergoing plastic surgery are: arterial hypertension, arteriosclerosis, hyperlipidemia, type 2 diabetes, chronic anemia, degenerative osteoarthritis, COPD, pulmonary hypertension, varicose veins and cholelithiasis.
Not all people with massive weight loss are good candidates for reconstructive plastic surgery. In addition to the physical assessment, it is important to make an extensive evaluation looking for psychological or psychiatric disorders, and even for dysmorphic disorders.46,47
Previous medications. All medications taken by the patient should be investigated: physician prescribed, self-prescribed, homeopathic and herbal products. Some herbal medications and teas contain active ingredients that may interact with drugs administered perioperatively, or may facilitate bleeding or arrhythmias. It is important to determine which medications should be continued until the day of the surgery and which should be discontinued with sufficient anticipation, such as MAO inhibitors, aspirin, warfarin and anorexics. Fen-phen, an anorexic comprised of fenfluramine and phentermine, was popular until 1997, when it was removed from the market because studies showed it produced multiple cardiac valve disease and long term or irreversible pulmonary hypertension.48 Unfortunately, this drug is still used in some countries, therefore is imperative to determine if there is a history of using it.
Airway. Evaluation of the airway should follow the usual recommendations for any patient, since it has been demonstrated that obesity per se does not significantly increase the difficulty of intubation, except in the case of the morbidly obese. Patients with significant weight loss have not been studied with respect to the difficulty of intubation. In our practice we have not noted specific difficulties. When a difficult airway is suspected it is advisable to position the patient with a cushion behind their head to maximize the distance between the chin and the thorax to facilitate laryngoscopy and intubation. All instruments recommended for the management of a difficult airway should be on hand. Conscious patient intubation is a safe alternative when appropriate instruments are not available. When possible, use regional anesthesia (Table 3).
Parameter |
Observations |
History and physical |
A general clinical review with physical exam done by the anesthesiologist prepares them to anticipate problems such as difficult airway, vertebral abnormalities, mental disorders, disorders of the family environment and the possibility of litigation |
Consultation with another specialist |
It is prudent to know the opinions of the bariatrician, pulmonologist, cardiologist, endocrinologist, surgeon, and psychologist in the search for polypharmacy, drug interactions, etc. |
Electrocardiogram |
Arrhythmias, ischemia, enlargement or dilation |
Chest X-ray |
Useful in smokers, suspicion of TB, neoplasm, emphysema, kyphosis, pulmonary hypertension |
Echocardiogram |
Mandatory study in patients with severe arterial hypertension, ischemia, dilated myocardiopathy |
Spirometry |
Utility has not been demonstrated; however it is recommended in chronic lung disease and smokers |
CBC |
Diagnosis of subclinical anemia |
Coagulation tests |
PT, aPTT, INR and bleeding time are mandatory in all patients, especially those using anticoagulants, those with hepatocellular damage and those with malnutrition. Thromboelastography to evaluate a prothrombotic state. |
Special blood tests |
Evaluation of kidney, liver and metabolic function, electrolytes and vitamin deficiencies, Iron levels |
Urinalysis |
Hematuria, proteinuria and changes in urine density |
HIV, hepatitis, drugs, pregnancy |
Order based on data in the history and previous experience. It is prudent to request an HIV test to protect medical and paramedical personnel. |
Table 3 Parameters to include in the pre-anesthetic evaluation of patients with massive weight loss scheduled for plastic or reconstructive surgery
Cardiovascular system. Arterial hypertension is common. Ask the name and dose of all antihypertensive medications, and keep the patient on these medications until the day of surgery. A resting EKG is useful and should be performed on all patients, independent of their age, based on the previously described cardiopulmonary abnormalities. Through the EKG various parameters can be evaluated, such as right and left ventricular hypertrophy, atrial enlargement, arrhythmias, ischemia and previous infarcts. A stress test, though advisable, is not always possible given the physical conditioning of these patients and osteoarticular limitations which present obstacles to the test. Echocardiography is recommended to evaluate cardiac function, especially ventricular ejection fraction. It is imperative to evaluate the lower extremities for edema and venous insufficiency, since the latter may increase the risk of thrombosis and venous embolism.
It has been shown that six months after bariatric surgery patients continue with a hypercoagulation state which can favors DVT/ PE, so it is mandatory to exhaustively study this possibility. Traditional coagulation tests and thromboelastography are recommended.49
Respiratory system. Undiagnosed pulmonary hypertension may cause serious complications during anesthesia, especially during induction. It should be suspected if the patient presents dyspnea, fatigue or syncope during exercise. This clinical picture is secondary to the right ventricle being unable to compensate for the increased demand presented by exercise. An EKG and chest x-ray are useful, though they do not conclusively support the diagnosis. Emphysema, asthma and OSA should be investigated, as well as a history of primary or second hand smoking.
These surgical procedures are elective and therefore offer ample opportunity to do a complete pre-anesthetic evaluation, in which the anesthesiologist should thoroughly review the patient’s chart and the patient themselves, actively seeking the previously enumerated co-morbidities. These pathologies should be optimally controlled prior to establishing a surgical plan. The anesthetic plan is based on this preoperative evaluation and the initial surgical plan. Any anesthetic technique may be applied to these patients, in accordance with the preoperative evaluation and surgical plan. Nevertheless, it is prudent to follow the recommendations for anesthesia in the obese patient since, as previously discussed, patients with massive weight loss are similar to overweight patients.
Just as a surgical intervention is planned, an anesthesiological plan should also be established. In our unit a routine has been established that can be adapted to each patient once they have been evaluated and the surgical plan has been discussed. For procedures below the level of T5-T6 neuroaxial block is used (spinal, epidural or combined). For procedures involving only thoracic dermatomes we prefer general anesthesia, though some patients having breast surgery are managed with cervicothoracic epidural blocks. In some patients with borderline hemoglobin levels or mild anemia who are scheduled for combined surgery involving the abdomen, thoracic wall and arms, neuroaxial block is used for the inferior segments, complemented by general anesthesia for the breast and arm portions of the surgery. Facial surgery is performed using conscious sedation or, in rare instances, general anesthesia.50
Preanesthetic medications. While the use of benzodiazepines in the obese patient is controversial, we recommend giving these patients sublingual lorazepam or midazolam an hour prior to the induction of anesthesia. Oral clonidine 0.1 mg facilitates sedation, dry mouth and provide hemodynamic stability during endotracheal intubation and reduces the need for local and general anesthetics. It is advisable to administer antiemetic and H1 receptor blockers, and avoid the use of opiates. We have recently introduced melatonin as part of the pre-anesthetic medication scheme.
Monitoring. Clinical and electronic vigilance is the base of good anesthesiological technique. For non-invasive arterial pressure (NIBP) monitoring, an appropriate cuff should be chosen that covers 2/3 of the arm, since smaller cuffs give elevated readings. Reliability of NIBP is poor in gynecoid type obese patients, whereas obese patients of the android type tend to give reliable readings. Ideally, invasive arterial pressure measurements are used. Oxymetry and capnography are mandatory, as is continuous EKG monitoring, with all precordial leads whenever possible. It is important to monitor airway pressure and calculate pulmonary compliance. Airway pressures greater than 40 cm H2O are high risk.
Venous access. Venous access may be difficult. When it is not possible to place an 18-G catheter, it is advisable to begin with a smaller catheter and change it as early as possible. Another alternative is the placement of a central venous line, which at times can be difficult.
Drugs dose. Calculation of the dose of the different medications used in anesthesiology is based on body weight in the majority of cases. This is not always appropriate, especially in the case of lipophilic drugs. Obesity represents a challenge when attempting to establish an optimum dose, an especially difficult challenge when the medication in question has a narrow therapeutic index, as is the case with the majority of the drugs used in anesthesia. The factors which intervene in the distribution of drugs into various tissues include body composition, regional blood flow and the affinity of the drug for plasma proteins and tissue components. Drugs with a low lipid affinity should be dosed based on the patient’s ideal body weight. Distribution of a drug between lean tissue and fatty tissue is influenced by obesity, and it has been said that the loading dose should be based on total body weight. Medications with a narrow therapeutic index should be used prudently and the dose should be adjusted to achieve plasma concentrations within the recommended therapeutic window.51
Mechanical ventilation. Tidal volume should be calculated based on ideal body weight. A tidal volume of 8-12 mL/kg with a respiratory rate of 8 to 14 will avoid hyper- and hypo-capnia.52 Tidal volumes greater than 12 mL/kg increase airway pressure and risk barotrauma. The use of PEEP with prolong inspiration times may improve oxygenation by recruiting and maintaining open more alveoli.
Regional anesthesia. Anatomic relationships that serve as references during diverse regional anesthetic techniques, especially neuroaxial bocks, are difficult to locate in these patients due to skin laxity and residual excess adipose tissue, making regional anesthesia a technical challenge. Frequently, longer needles are required to reach the epidural or subarachnoid space. When a peridural block is planned, it is prudent to insert the catheter a few extra centimeters into the epidural cavity since lax skin leads to increased mobility. Remember that a lower dose of local anesthetic is required due to the epidural fat and dilated epidural veins. Regional anesthesia is the preferred technique because it has been demonstrated that it reduces the likelihood of atelectasis, venous thrombosis and possibly pulmonary embolism. Bleeding is also reduced in comparison with general anesthesia. The addition of coadjuvant medication to local anesthetics optimizes the quality and duration of anesthetic block and neuroaxial analgesia. For procedures below the level of T5-T6 we recommend spinal anesthesia with hyperbaric bupivacaine or ropivacaine, 15 and 22.5 mg respectively, combined with 150, 300 or up to 450 µg of clonidine.53 This technique has a duration of 5 hours, and the most common side effect is easily managed arterial hypotension.
General anesthesia. When general anesthesia is to be used, it is important to preoxygenate and denitrogenate the patient. It is also important to anticipate the possibility of a difficult airway. Induction is facilitated with hypnotic medications, propofol being the most commonly used. It is advisable to use non-depolarizing muscle relaxants with a rapid onset and short duration of action to facilitate endotracheal intubation. Real-time ultrasound of the trachea is an accurate, feasible, and fast method in confirming endotracheal tube placement. Maintenance with desflurane or sevoflurane facilitates hemodynamic stability and rapid anesthetic recovery. In our practice we complement general anesthesia with fentanyl or sufentanil in bolus or continuous infusion.
Combined techniques. As previously mentioned, it is possible to combine regional and general anesthesia in cases of surgery involving multiple body segments. The total dose of all medications used should be closely monitored, especially local anesthetics, to avoid acute toxicity. The maximum tolerable dose of lidocaine should not exceed 1000 mg.
Post-anesthetic precautions. The majority of anesthetic accidents occur during the postoperative period; hypoxia, respiratory failure, recurarization, hypothermia and acute myocardial infarction are some of the reported incidents. All patients should continue with monitoring (EKG, oxymetry, NIBP and clinical vigilance), especially those who have undergone extensive surgery, with transoperative use of opioids and/or muscle relaxants. The patient should receive supplementary oxygen using nasal prongs, adequate analgesia, and the thorax should be elevated to 30 degrees to facilitate ventilation. Precautions against and observation for signs of venous embolism should be continued.
Complications among this type of patient are more frequent than anticipated and both anesthesia and surgery are determining factors. Undesirable anesthetic incidents are related to the physical condition of each individual, the changes previously described, the prolonged time of anesthesia, positions which impede circulation, ventilation and hypothermia. The following paragraphs describe the most relevant complications.
Pulmonary embolism. Thrombotic events are the main complication, whether or not they involve embolism. For example, abdominoplasty has a 1.1% risk of DVT, a complication attributed to the plication of the rectus abdominis, which in turn increases the intra-abdominal pressure, reduced venous return, causing venous distention and thrombosis. Huang et al.54 found other factors that increased intra-abdominal pressure, such as degree of bed flexing, abdominal bandages and general anesthesia. A prospective study by Gravante et al.55 of patients who underwent abdominoplasty and flank liposuction found an incidence of PE of 2.9%. All patients had received thromboembolism prophylaxis. These authors found a significant relationship between fat extraction of more than 1500 g and time of anesthesia exceeding 140 minutes. Another group of investigators (56) studied 138 post-bariatric patients undergoing body contour surgery (abdomen, back, arms and thorax) and found three patients with DVT requiring anticoagulation and one death due to PE. This implies a 2.9% risk of thromboembolism, the same as reported by Gravante.55 The BMI of patients with thrombosis was 48.5 vs 31.8 for patients who did not present this complication. It is important to establish a plan of venous thromboembolism prophylaxis that includes elastic stockings, intermittent compression pneumatic pump, heparin and early ambulation. The program should be applied commensurate with the degree of risk factors.
Bronchoaspiration. The anatomic and physiologic changes of bariatric surgery may facilitate bronchoaspiration during anesthesia. A study by Jean et al.57 compared 66 post bariatric patients (gastric banding and vertical gastroplasty) with 132 controls and found that, among the former group, pulmonary aspiration was significantly increased (4 patients, 6%, p<0.006). All four cases of aspiration belonged to the gastric banding group. These authors believe that bronchoaspiration should be considered a significant risk. We have only seen one case of gastric regurgitation in our practice, without bronchoaspiration, in a patient with a gastric band who underwent facial surgery under conscious sedation. The expandable chamber of the gastric band in this patient had been full and was immediately emptied. It is advisable to empty this chamber prior to induction of anesthesia, use anti-Trendelenburg position, avoid mask-ventilation, and use rapid sequence induction strategy with endotracheal intubation and fully awake extubation.58
Hypothermia. Hypothermia is a common event in plastic surgery patients due to the long period of time in which they are exposed to the cold environment of the surgical room. Shivering, increased oxygen consumption, myocardial ischemia and changes in coagulation are some of the complications reported due to a critical perioperative drop in body temperature. One study of plastic surgery patients showed that maintaining transoperative normothermia helps patients maintain normal coagulation. In unprotected patients the temperature dropped 20C and both the thromboplastin time as well as bleeding time increased significantly.59 Patients undergoing liposuction of large volumes receive high doses of epinephrine, lidocaine and i.v. solutions that produce important cardiovascular and thermoregulatory changes. Kendel et al.60 found a change in the cardiac index (57%), heart rate (47%) and mean pulmonary artery pressure (44%). Central venous pressure remained unchanged. Maximum epinephrine levels were observed 5 to 6 hours after induction of anesthesia, and a significant correlation was found between the epinephrine levels and transoperative cardiac index (r=0.75). All patients suffered hypothermia, with a mean temperature of 35.5oC.
Surgical complications. For its interest, only some of the perioperative complications are mentioned. Although many researchers have mentioned risks inherent to this group of patients, we only found one study that investigated risk factors affecting postoperative outcome; Parvizi et al.61 evaluated 205 patients who underwent dermolipectomy under general anesthesia; smoking combined with the age, a BMI higher than 30 kg/m2, and the amount of removed tissue lead to significantly more wound healing problems in nearly all patients. Irrespective of the quantity of tissue removed, no main risk factor for complications could be identified. These authors found major complications that required operative revision and/or antibiotics in 10.2 %, including 2.9 % cases of infections. Forty-one percent had trivial complications, such as seromas, hematomas, wound healing problems, and wound dehiscence. It has been mentioned that post-surgical infections are more common in patients with massive weight loss undergoing body sculpting surgery. A retrospective study of 222 patients undergoing abdominoplasty or panilectomy showed an incidence of surgical incision infection of 12%, hematoma 6% and seroma 14%. Patients with weight loss had incision complications with an incidence of 41% vs 22% in the control group.62 A recent study63 including 153 patients who underwent a total of 198 body contour surgery after bariatric surgery mentioned that 55.5% had complications (major complications was 13%, and for minor complications 87%). Complication rates according to the type of surgery were circumferential abdominal lipectomy, 55.7%; extended abdominal lipectomy, 53.7%; cruroplasty, 69%; breast surgery, 57%; and brachioplasty, 40%. Patients who presented with bleeding enough to require transfusion (P = 0.000) and with weight of the resected tissue greater than 2700 g in abdominoplasty (odds ratio, 3.26; 95% confidence interval, 1.48-7.1) had a higher complication rate. There were no PE incidents in this study.
The proportion of obese people continues to grow throughout the world and this has favored the increase of bariatric surgery, and proportionally also increases the demand for surgical procedures of body contouring. As anesthesiologists, we are obliged to know each and every one of the changes produced by obesity and after bariatric surgery, since these anatomical, functional and psychological modifications can interfere with the anesthesiological management. Anesthesia plays a decisive role in the advancement of transformational plastic surgery among these persons. They have special risks due to the unresolved problems of obesity, as well as plastic / reconstructive procedures, which usually require prolonged anesthesia time. Teamwork is the cornerstone of success in the integral treatment of these patients. The anesthesiologist-surgeon-patient interaction should be scrupulously planned, and alternatives should always be considered, for the safety of the patient.

©2020 Whizar-Lugo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.