Journal of
eISSN: 2373-6437


Short Communication Volume 16 Issue 3
1National Cancer Institute (INCA) Senior Researcher, Brazil
2Anesthesiologist at the National Cancer Institute (INCA), Brazil
3Head of the Anesthesiology Service of the National Cancer Institute (INCA) Anesthesiologist, Responsible for the CET-SBA of the National Cancer Institute, Brazil
4INCA Anesthesiologist, Co-Responsible for the CET-SBA of the National Cancer Institute, Brazil
5Adjunct Professor of Anesthesiology at the UFG Faculty of Medicine, Responsible for the CET-SBA of the Hospital CRER, Brazil
6Professor of Anesthesiology at the UFG Faculty of Medicine, Responsible for the CET-SBA of the HCUFG, Brazil
Correspondence: Dr. Luiz Eduardo Imbelloni, National Cancer Institute (INCA) Senior Researcher, Av. Epitácio Pessoa, 2356/203, Lagoa, 22411-072- Rio de Janeiro, RJ, Brazil
Received: June 16, 2024 | Published: June 28, 2024
Citation: Imbelloni LE, Rivoli ALC, de Lemos Neto SV, et al. Tattoo in patients undergoing lumbar and thoracic subarachnoid puncture. Prevention behaviors. J Anesth Crit Care Open Access. 2024;16(3):69‒71. DOI: 10.15406/jaccoa.2024.16.00592
The number of patients with tattoos and which are operated is increasing significantly in recent years. Some complications, mainly in neuraxial anesthesia, have been reported are unconvincing due to the lack of real evidence-based material. Tissue coring and deposition of epithelial cells in the CSF is a known entity. However, the theoretical risk exists and the anesthesiologist questions whether to puncture the neuraxial in patients with a tattoo at the puncture site. More organic pigments are being used and the precise composition of tattoo inks remains unknown. As a conduct for asepsis and antisepsis during spinal puncture (lumbar and thoracic), 14 steps were described to avoid neurological complications during spinal anesthesia. This approach during anesthesia in the neuraxial area meant that I never had a neurological complication, nor the appearance of an epidermoid tumor. Thus, a total of 17 steps that must be followed exactly when performing the puncture on the back of tattoo patients. If there is no pigment-free skin area available, a superficial skin incision is the method of choice.
Keywords: Neuroaxial blocks; Tattoos; Tattooing; Complications; Tissue coring
In a recent Editorial "Understanding the simplest (spinal anesthesia), It is not so easy", I state that knowledge without practice results in an immense distance, and that knowledge with practice allows for a full understanding of spinal anesthesia (SA).1 In another article about the antiseptic solutions used to perform subarachnoid puncture (lumbar and thoracic), 14 steps were described so that in the year I completed 50 years of graduation with more than 470 articles published, and I did not have any neurological complications or death during SA.2 In this article to improve antisepsis during access to the neuraxial, which is properly protected with a bone structure and nine steps to reach the subarachnoid space, I can say that God or the evolution of human beings were extremely wise and careful in protecting the spinal cord. And I was one of the first Brazilian anesthetists to publish laparoscopic cholecystectomy with SA3 and thoracic spinal anesthesia (TSA) for several procedures.4
To verify the incidence of cells epithelial cells that reflux together with the first and third drops of cerebrospinal fluid (CSF) from patients undergoing SA with a 25G cutting tip needle with mandrel, squamous epithelial cells were identified in 35 (89.7%) of the samples from the first drop, in 34 (87.2%) of the third drop and in 24 (61.5%) of spinal needles.5 In another similar study with 50 patients in each group using three types of needles: 25G cutting, 25G pencil tip and atraumatic (non-cutting) with special curvature, it was found that with the atraumatic needle the number of cells transported was significantly lower compared to the cutting needles and pencil tip, but there was no significant difference between the first and third drops with the three needles.6
If a simple subarachnoid puncture with different types and gauges of needles is responsible for the appearance of epithelial cells in the CSF, imagine skin with different types of ink used in tattoos, especially in the thoraco-lumbar-sacral spine. Tattoos in Brazil are quite common and have been gaining more and more prominence in recent years. According to “Sebrae”, Brazil ranks ninth among the countries with the highest number of tattooed people, with 22% of the population having permanent body art.7 Accessing websites with different types of tattoo ink showed that it is specially developed to ensure that the color remains bright and vibrant for a long time.8 Furthermore, using the right ink also ensures that your skin does not react negatively to the tattoo. This is because tattoo ink is free from allergenic substances and does not contain heavy metals.8 Currently, more organic pigments are being used and the precise composition of tattoo inks remains unknown.
Epidural anesthesia and tattoo
There is a great difference between access to the epidural space and the introduction of a needle into the subarachnoid space, with several descriptions of epidermoid tumors after needle puncture during epidural anesthesia (EA) in parturients and spinal anesthesia (Figure 1,2). It shows that accessing the epidural space is different from accessing the subarachnoid space, where it is in contact with CSF and can disseminate epithelial cells.
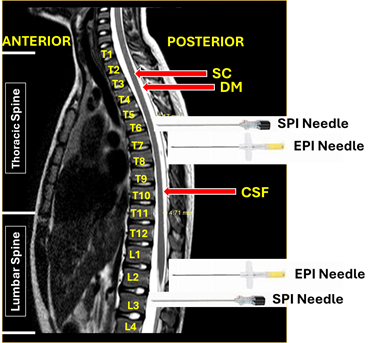
Figure 1 Magnetic resonance imaging of the thoraco-lumbar spine, with needle penetration into the epidural and subarachnoid spaces, both in the lumbar and thoracic regions.
(SC, Spinal Cord; DM, Dura Mater; CSF, Cerebrospinal Fluid).
In 2002, a published article was alerted to the theory of the risk of introducing exogenous pigments into the epidural space, after piercing a tattoo during epidural anesthesia in three parturients, which would lead to epidermal tumors and/or chemical arachnoiditis.9 Recently, a chronological review of 18 years of medical literature was published on the risks of introducing tattoo pigments through lumbar EA in obstetric patients, concluding that so far, nothing convincing of this complication has been reported following an EA through a tattoo.10
In two articles published about a survey with 162 anesthesiologists about tattoo and EA, showed that 57% had already been faced with this situation and that 60% would perform EA in the non-tattooed area, and 6% refused to use EA despite having a tattoo.11 In another study on EA in tattoo patients, 54 anesthesiologists showed that 57% of them would perform EA (58% without precaution and 42% with incision), 39% percent would not do so, either because of the risk of migration (66%) or simply as a precaution (43%), two-the third would provide an alternative to EA.12
Spinal anesthesia and tattoo
Iatrogenic intraspinal epidermoid tumors have been reported as sequelae of lumbar puncture. Acquired epidermoid tumors are thought to result from implantation of epidermal tissue into the subarachnoid space at the time of lumbar puncture. It is more common to see this complication of lumbar puncture if a stylette is not used during the procedure, because without the use of stylette, skin tissue can easily be detached by a hollow needle and implanted into the subarachnoid space.
Subarachnoid puncture to perform spinal anesthesia in patients with tattoos on the back, through which the needle will pass requires some considerations, and may represent a theoretical risk of taking the ink and cells to the CSF and could potentially lead to complications such as infection or formation epidermoid tumor.13 During all my spinal anesthesia on tattoo patients I believed in the real risk of complications arising from the introduction of the cell with ink, although it is not well documented, and the evidence is even theoretical, however numerous cases of epidermoid tumors have been published.13 Skin cells can be carried into the spinal canal during lumbar and thoracic puncture, rarely resulting in an intraspinal epidermoid cyst, and therefore, it is possible to introduce tattoo pigment into the spinal canal.
Conduct for access to the neuraxial block in a patient with tattoo
During access to neuraxial blocks, the anesthesiologist is faced with situations in which there is a potential risk of transverse infection, and it is important to recognize and minimize this risk, especially regarding antisepsis and the introduction of cells through puncture needles and the use of the introducer, for some types of needles. However, the actual risk of complications from the introduction of skin and tattoo ink occurring is not well-documented, particularly during SA. In practice, many anesthesiologists will assess the situation on a case-by-case basis, weighing the risks of proceeding with SA against the risks of alternative anesthesia methods, such as general anesthesia.
Studying 36 young male adult rabbits it was shown that the intrathecal injection of saline solution through a needle inserted into the tattooed skin can produce histological changes in the meninges of rabbits.14 Fragments of ink were trapped inside the spinal needles despite the presence of a stylus. In a letter to the Editor, the authors, who study the subject extensively in pregnant women, contested the results of the study on tattooed rabbits.15
In the same way where I showed 14 steps that I apply methodologically from the beginning of my studies with spinal anesthesia.2 This approach has meant that during my 50 years in the profession my patients have never had a neurological complication, nor the appearance of an epidermoid tumor. Therefore, by not using an introducer (a skin biopsy is performed) even with pencil point needles, I am adding another item to this approach, totaling 17 steps that must be strictly followed (Table 1).
|
N |
Conduct for neuroaxil block |
|
1 |
Entrance to the surgical center washing hands with soap |
|
2 |
Patient in the antisepsis puncture position with 70% alcohol or alcoholic chlorhexidine |
|
3 |
After antisepsis with a single layer, opening the tray for blocking |
|
4 |
Never dry the antiseptic with gauze and allow it to dry spontaneously. |
|
5 |
After opening the tray, placing the needle and sterilized local anesthetics |
|
6 |
Verification of the batch, date of manufacture and expiration date of anesthetics |
|
7 |
Aspiration of liquid from the ampoule |
|
8 |
Choosing the space to be punctured |
|
9 |
Infiltration with 1ml of lidocaine 1% with syringe and insulin needle |
|
10 |
Infiltration with 3 ml of lidocaine 1% in subcutaneous cellular tissue with a 27G needle |
|
11 |
Wait for it to take effect |
|
12 |
In patients with tattoos, skin incision is made to introduce the epidural or spinal needle |
|
13 |
Subarachnoid puncture with the chosen needle |
|
14 |
If Whitacre no need for introducer |
|
15 |
If it is Quincke, do not use an introducer |
|
16 |
Subarachnoid injection with chosen dose and local anesthetic |
|
17 |
If using adjuvant, use it in a separate syringe as it alters the baricity of the LA |
Table 1 Conduct for access to the neuroaxis in a patient with a tattoo on the back interesting to the spinal column
Tissue coring seems to be a common phenomenon during lumbar or thoracic puncture. Tissue coring and deposition of epithelial cells in the CSF is a known entity. Tattoos have increased significantly in the population, with an increase mainly on the back and often modeling the spine. During spinal puncture, pigments could be transmitted in deeper tissue layers and even in the spinal channel. In rare cases, burning or painful sensations were reported. Theoretically, there is a risk for a future development of inflammatory and granulomatous reaction in the spinal channel. The paucity of evidence in the current literature regarding neuraxial blocks through tattooed skin, I do not recommend exposing patients to this rare theoretical risk, but I do recommend choosing the another access no tattoo. If there is no pigment-free skin area available, a superficial skin incision is the method of choice.
None.
None.

©2024 Imbelloni, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.