Journal of
eISSN: 2373-6437


Case Report Volume 1 Issue 6
1Depertment of Anesthesiology and Intensive Care, American Hospital, Albania
2Department of Anesthesiology and Intensive Care, Universitary Center of Trauma, Albania
Correspondence: Gentian Huti, Head of the Department of Anesthesia, Intensive Care and Emergency, American Hospital, Tirana, Albania, Tel 00355689025991
Received: August 10, 2014 | Published: December 4, 2014
Citation: Huti G, Arapi B, Bilaj M, Abdyli A, Vaso A (2014) Spinal Anesthesia in Laparoscopic Cholecystectomy in a 75 Years Old Patient with Congestive Heart Failure NYHA III . J Anesth Crit Care Open Access 1(6): 00036. DOI: 10.15406/jaccoa.2014.01.00036
Laparoscopic cholecystectomy (LC) is a relatively common surgical procedure which is generally performed under general anesthesia. We report a case of a 75-year old female patient presented to our emergency with cholecystitis acute symptoms. She had been diagnosed formerly with pneummonia and pleuritis and she was a heavy smoker. Other risk factors included diabetes mellitus type II, left nephrectomy and age. Two months before presenting to our hospital she had a coronary angiography and had a revascularization of LAD artery with PCI and a DES implanted.
Echocardiography show ed an EF of 15-20%, apical aneusysm and an adhered septal thrombus. After the surgery consult the patient was recommended for a surgical removal of the gallbladder under laparoscopic approach. Upon arrival at the operating room routine monitoring was established. The patient liedon theright lateral side so that spinal anesthesia could be performed. A 24G spinal needle was used to enter the subarachnoid space at the T6-T7 intervertebral space under complete aseptic technique. Bupivacaine 0.25% 3.5ml was injected so that a sensory loss up to T4 dermatome was achieved. The procedure lasted for about 60 minutes without any complications.
Keywords: Spinal Anesthesia, Laparoscopic Cholecystectomy, Pain, Cardiac Patient
LC, Laparoscopic Cholecystectomy; LAD, Left Anterior Descending Artery; RCA, Right Coronary Artery; ECG, Electrocardiograme; PCI, Percutaneous Coronary İntervention; DES, Drug-Eluting Stent; EF, Ejection Fraction
Laparoscopic cholecystectomy (LC) is a relatively common surgical procedure which is generally performed under general anesthesia. However in some specific cases we, as anesthesiologist, are forced to look for different methods such as epidural or spinal anesthesia in order to perform the above mentioned procedure. We are all aware of the benefits of this procedure performed under laparoscopic approach. Advantages of LC such as less pain and short hospital stay make it the treatment of choice for cholelithiasis.1 From the observation of the results in several studies it is observed that spinal anesthesia is a very feasible and safe anesthetic method to be used in this procedure resulting in a very good postoperative management of the patient.2 To the best of our knowledge there are relatively few cases of cardiac compromised patients who have been operated using spinal anesthesia as an anesthetic method and have had a satisfactory perioperative management with a good postoperative outcome.
A 75-year old female patient presented to our emergency room with shortness of breath, weakness and fatigue. She refered to be in similar condition for at least 1 month. On examination she looked ill with shortness of breath while resting. She had been diagnosed formerly with pneummonia and pleuritis and she was a heavy smoker. Other risk factors included diabetes mellitus type II, left nephrectomy and age. Two months before presenting to our hospital she had a coronary angiography and had a revascularization of LAD artery with PCI and a DES implanted. On admission ECG was abnormal with ST elevation in anterolateral leads and with a prolonged QT segment (Figure 1).
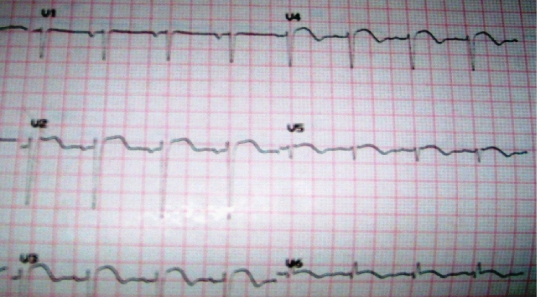
Figure 1 ECG of the patient showing ST elevation in anterolateral leads with a prolonged QT segment.
We performed an echocardiography in which apical akinesia and apical aneurysm were found. EF was 25%. A coronary angiography performed and a second stent implanted on mid RCA while the stent at LAD was found patent without any stenosis. The patient was discharged after 3 days in a much better condition. Nearly 2 months later she presented again at our hospital with fatigue and weakness. She complained of abdominal pain localized in right hypochondrium. She waslooking malnourished and had lost almost 10 kg last 2 months. She looked very pale with periferic edema especially on lower extremities. We performed an abdominal echo which showed a gallbladder full of stones with normal walls and no edema. Left kidney was absent and right one slightly hypertrophic.
On ECG heart rate was 102 bpm, sınusal tachycardia with fusion complexes with ST segment elevation in V1-V5 leads and negative T wave on V2-V6 leads. Echocardiography showed an EF of 15-20%, apical aneusysm and an adhered septal thrombus. Hemodynamics on admission was 85/50 mmHg with weak peripheral pulses on palpation. The hemodynamic status was improved after dopamine infusion at 5γ/kg/min. After the surgery consult the patient was recommended for a surgical removal of the gallbladder under laparoscopic approach.
The preoperative examinations were as follows: CK-MB 16.3 U/L, BUN 22 mg/dl, Creatinine 0.62 mg/dl, Hgb 11.3 g/dl, RBC 3.73 x 106 ųL, WBC 5.8 x 103 ųL, Hct 34.4 %, PLt 179 x 103 ųL, Troponine 0.06 ug/L, ALP 75 U/L, ALT 30 U/L, Amylase 25 U/L, AST 31 U/L, GGT 15 U/L, Direct Bilirubine 0.13 mg/dl, Total Bilirubine 0.62 mg/dl, Calcium 7.63 mg/dl, Sodium 131 mmol/L, Magnesium 1.71 mg/dl, Potassium 3.4 mmol/L, Total protein 4.34 g/dl, Albumine 2.2 g/dl, PT 79%, INR 1.14, APTT 34.6 sec, ESR 6 mm/h.
Upon arrival at the operating room routine monitoring was established. Measured blood pressure was 110/70 mmHg under dopamine stimulation with 5γ/kg/min and heart rate 125/min with oxygen saturation on oxygen mask of 99%. A 16G i.v and a 18G radial arterial cannulation were established under local anesthesia with ametop. Left internal jugular vein was cannulated under local anesthesia with lidocaine 2% and triluminal catheter was inserted for central venous pressure monitoring and for injecting resuscitation drugs if required. The patient liedon theright lateral side so that spinal anesthesia could be performed. A 24G spinal needle was used to enter the subarachnoid space at the T6-T7 intervertebral space under complete aseptic technique. Bupivacaine 0.25% 3.5ml was injected so that a sensory loss up to T4 dermatome was achieved. Noradrenaline infusion at a dose of 0.02γ/kg/min was started immediately after the spinal anesthesia was performed. This is not a routine protocol but was specifically given to this patient being very helpful in maintaining a satisfactory hemodynamic status after applying spinal anesthesia.
During the surgical procedure the patient was stable with blood pressure around 105/60 mmHg, heart rate of 130 bpm, SpO2 98% with nasal oxygen 6L/min. Intraabdominal pressure was maintained aroud 8 mmHg in order to minimize the effects of pneumoperitoneum on cardiovascular system. The procedure lasted for about 60 minutes without any complications. 900 ml of saline 0.9% and 50ml of human albumine 20% were given during the procedure. Urine output was 400 cc (unstimulated). The patient left the operating room in a good condition with heart rate 133/min, blood pressure 108/60 mmHg, under stimulation with dopamine 5γ/kg/min and noradrenaline 0.02γ/kg/min, SpO2 98%. She was satisfied with the outcome and refered she had not experienced any discomfort, pain or shortness of breath during the operation.
Laparoscopic cholecystectomy has the advantages of causing less postoperative pain and requiring a short hospital stay, and therefore is the treatment of choice for cholelithiasis. Laparoscopic cholecystectomy under spinal anesthesia with low-pressure pneumoperitoneum can be performed safely and satisfactorily without major complications by experienced surgeons.3 In several studies spinal anesthesia is a safe choice in these types of procedures. Postoperative follow-up shows that all patients are satisfied and they are keen advocates of spinal anesthesia.4
In cardiac compromised patients the use of regional anesthesia has become more frequent with the evolving of anesthetic and monitoring techniques during the surgical procedure.5 It seems regional anesthesia may be alternative method to general anesthesia for laparoscopic cholecystectomy in patients with cardiopulmonary disease. However the safeness of this technique should be evaluated with more cases undergoing the above mentioned procedure under this anesthetic method.6
We may say that spinal anesthesia is a safe anesthetic method to be used in these patients by experienced and qualified anesthesiology teams. However cardiac compromised patiets undergoing spinal anesthesia need to be evaluated properly and treated correctly in the preoperative period for a better perioperative outcome. A patient with a limited cardiac reserve and pulmonary problems tends always to be a great challenge to us as anesthesiologist.
None.
None.
Authors declare that there is no conflicts of interest.

©2014 Huti, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.