Journal of
eISSN: 2373-6437


Review Article Volume 16 Issue 5
1Department of General and Visceral Surgery, National Hospital of Niamey, Niger
2Pediatric Surgery Department, Amirou Boubacar Diallo National Hospital, Niger
3Thoracic and Cardiovascular Surgery Department, Niamey General Reference Hospital, Niger
4General Surgery department, Maradi General Reference Hospital, Niger
5Trauma department, National Hospital of Niamey, Niger
6Anesthesia and resuscitation Department, National Hospital of Niamey, Niger
Correspondence: Boka Tounga Yahouza, Resident Doctor of Surgery General, National Hospital of Niamey, Niger, BP 238, Tel +22798597850
Received: October 01, 2024 | Published: October 18, 2024
Citation: Boka TY, Sidi MIH, Rabiou S, et al. Post-traumatic diaphragmatic rupture: two observations at the National Hospital of Niamey. J Anesth Crit Care Open Access. 2024;16(5):135‒137. DOI: 10.15406/jaccoa.2024.16.00604
Introduction: Trauma to the diaphragm is rare, accounting for 3.6% of injuries sustained in road accidents. They are the result of violent trauma and most often occur in the left dome.
Observations: The two patients were young adults (18, 55), male, and all victims of road traffic accidents resulting in firm trauma to the thorax. All patients had left basithoracic lesions. Both patients were diagnosed intraoperatively based strong clinical and radiological suspicion. The diaphragm ruptures presented by our patients were found on the left, with intra-abdominal viscera ascending into the thorax. Therapeutically, an emergency exploratory laparotomy was performed. The approach was abdominal for two patients, and the surgical procedure involved lowering the herniated organs and suturing the diaphragm for both patients. Postoperative management was straightforward.
Conclusion: Post-traumatic diaphragmatic hernia is a particular injury in traumatology. It most often occurs in the setting of polytrauma. Its seriousness derives from its complications and associated lesions, which can be life-threatening.
Keywords: closed thoracic trauma, diaphragmatic rupture, polytrauma.
Traumatic rupture of the diaphragm is a rupture of the diaphragm more or less associated with intrathoracic ascension of post-traumatic abdominal viscera and is only encountered in 0.5 to 5% of thoraco-abdominal trauma.1 Diaphragmatic ruptures are present in 0.8 to 5% of polytrauma patients. In 80 to 90% of cases, they follow a road accident. They can also be found during assaults with firearms or knives.1,2 These ruptures are sometimes difficult to diagnose with routine examinations, but are now facilitated by diagnostic video-thoracoscopy, which can detect even a breach of less than 1 cm.2 Preoperative diagnosis of diaphragmatic rupture remains difficult in a Sahelian context . Treatment is surgical and the abdominal route is the reference route for left rupture and thoracotomy for right diaphragmatic dome breach.3,4 The severity of multiple trauma is attested by the ISS (injury severity score). An injured person is considered serious from an ISS score greater than 16.1,3 We report two cases of left diaphragmatic ruptures in post-traumatic diagnosed and treated in a Sahelian context, the aim of which was to describe the diagnostic and therapeutic modalities of the two cases diagnosed and treated in our context.
Observation 1
This was a 55-year-old patient, with no known pathological history, admitted to the emergency room for thoraco-abdominal trauma following a road accident. On clinical examination, the patient was conscious with good general condition. He was hemodynamically stable. Dyspnea was noted with a respiratory rate of 27 cycles/min, and oxygen saturation (SPO2) was 92% on room air. Dermabrasions were noted on the left hemithorax, asymmetry of the thorax and a decrease in the expansion of the left thorax. Auscultation found an abolition of vesicular murmurs in the left pulmonary field with a perception of hydro-aeric sounds. On abdominal examination, the abdomen was soft and painless. Hydro-aeric sounds perceived on abdominal auscultation. On additional examinations; an Emergency chest X-ray showed effacement of the left diaphragmatic dome, with passage of intra-abdominal viscera into the thorax strongly suggesting a diaphragmatic rupture. The left lung was pushed up and to the right (Figure 1). The thoraco-abdominal CT scan was requested but not performed. The biological assessment (hemogram, azotemia and creatinine) was normal. The patient was blood group O rhesus positive. We considered the diagnosis of a traumatic rupture of the diaphragm with repercussions on the ventilatory function and we indicated surgical management. Under general anesthesia, the approach was made via the left subcostal abdominal route. Exploration revealed the presence of the stomach and spleen ascended into the left hemithorax through a 4 cm diaphragmatic breach (Figure 2). The placement of a gastric tube allowed the stomach to be emptied and respiratory function to be improved. A lowering of the stomach and spleen ascended intra-abdominally is performed. The placement of chest drains preceded the diaphragmatic suturing by interrupted stitches with non-absorbable thread and the placement of a chest drain opposite the suture. The postoperative course was simple with the removal of the drain on day 5. The patient was discharged from the hospital on day 7 postoperatively in good health. Over a 6-month follow-up, no complaints were reported by the patient who had resumed his daily activities.
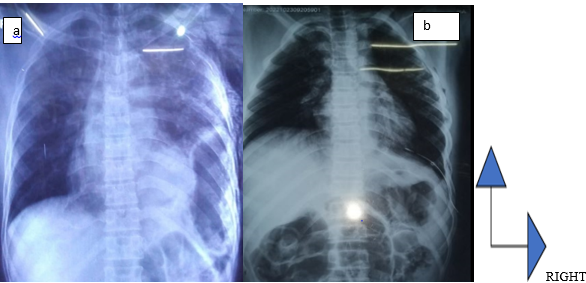
Figure 1 Emergency chest X-ray showing a left intrathoracic hydroaeric image with the ascension of the diaphragmatic dome (a). Postoperatively, the disappearance of the hydroaeric image without re-amplification of the left hemi-lung (b).
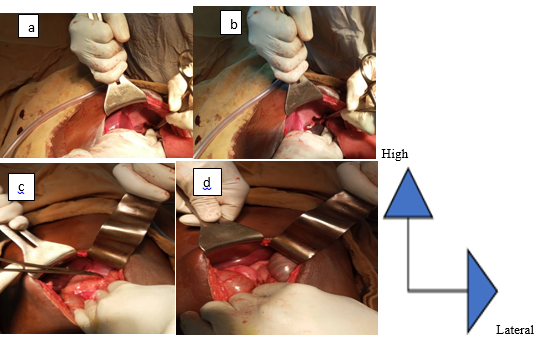
Figure 2 Intraoperative image showing the left diaphragmatic defect (a and b after reduction of the herniated viscera, c and d before reduction of the herniated viscera).
Observation 2
An 18-year-old patient with no known pathological history, was admitted to the emergency room for multiple trauma associating: closed thoraco-abdominal trauma, firm trauma of the left arm and a closed trauma of the contralateral leg. On admission, he was conscious, well-oriented in time and space with Glasgow 15/15. The patient was noted to be unstable in terms of hemodynamics (BP = 90/60 mm Hg and HR = 124 beats / minute) and ventilation (FR = 32 cycles / minute and spo2 = 88 % in room air). There were also dermabrasions on the left hemithorax and opposite the left hypochondrium, asymmetry of the thorax, and decreased amplification of the left thorax. On auscultation, vesicular murmurs were absent in the left pulmonary field replaced by hydro-aeric sounds. On abdominal examination, the abdomen is soft and painless to palpation and hydro-aeric sounds are heard on abdominal auscultation. Examination of the musculoskeletal system reveals a fracture syndrome of the left arm and a fracture syndrome of the right leg. The frontal chest X-ray had objectified a hydro-aeric image occupying the left hemi-thorax and pushing the diaphragmatic dome upwards. The mediastinal structures were pushed towards the contralateral side. The X-ray of the left arm had objectified a closed fracture of the humerus and the X-ray of the right leg objectified a closed fracture of both legs. The chest CT scan was not performed. The biological assessment was unremarkable. We performed surgical exploration by supra-umbilical median laparotomy. The exploration found a 7 cm rupture of the fleshy portion of the left diaphragmatic dome and abdominal viscera (greater omentum, stomach). We proceeded to reintegrate the organs with a suture of the diaphragmatic defect by separated stitches with non-resorbable thread 0. Osteosynthesis was performed at a later time for limb fractures. The postoperative course was simple. Chest X-ray on postoperative day 2 showed the disappearance of the initial lesions (Figure 3b). The chest drain was removed on postoperative day 4. The patient was discharged from the hospital on postoperative day 5. After 6 months, no complaints were reported by the patient.
Diaphragmatic rupture is a rare lesion in trauma patients but can be observed in multiple trauma patients or thoraco-abdominal trauma patients.5-9 Its frequency is 3.7% and is thought to be linked to the violence of the impact of the trauma.4,10 Since age is a risk factor for trauma in general, in our context traumatic rupture of the diaphragm is obviously found in young subjects for our two patients as well as the data from the literature.4,11 Traumatic rupture of the diaphragm is frequently found in male subjects.3,4,11 Both patients in our series were male. This male predominance could be explained by the socio-professional activity making men more exposed than women. In 90% of cases, post-traumatic diaphragmatic ruptures (PTDR) are consecutive to road accidents like the cases of our observations.12 The position of the liver on the right makes it protective and diaphragmatic continuity solutions occur three times out of four on the left.12,13 The passage of the abdominal viscera into the thorax induces a reduction in the diaphragmatic stroke with impairment of the ventilatory function.14 Eight to nine patients with diaphragmatic rupture have associated injuries. These include rib fracture (64%), splenic injury (53%), pulmonary contusion (45%), liver injury (36%) and others.15 Our two patients had a rupture on the left with a hernia occurring spontaneously after the trauma. The second patient was a multiple trauma patient combining thoraco-abdominal trauma and limb trauma. Diagnosis of diaphragmatic injuries is difficult preoperatively in the absence of reliable CT scans and video-thoracoscopy. Hence the need for CT scans in cases of thoraco-abdominal injuries. It is performed preoperatively in only 30 to 50% of injured patients.10,16,17 In our context, the CT scan was not performed in the two patients, nor was videothoracospy. The associated intra-abdominal lesions primarily concern the herniated organs and the organs of the supramesocolic level, and this is comparable to those found in the literature.4,10,18 Laparotomy was the surgical approach used in our series, in accordance with the data in the literature. The surgical approach for unstable patients as well as for stable patients is generally the median laparotomy due to the high frequency of associated abdominal injuries (fracture of the spleen, liver, gastric perforation, etc.).4,18 Thoracoscopy requires pulmonary exclusion, it does not provide good comfort to the operator. Laparoscopy in the lateral position is possible in a patient in good hemodynamic condition, without head trauma and without associated injury that could decompensate quickly.6 The diaphragmatic rupture was located on the left for both patients, consistent with literature data of around 60%, this high incidence of traumatic rupture of the left diaphragm is explained by the buffer effect that the liver causes at the level of the right hemidiaphragm.7,18 Bilateral diaphragmatic rupture is exceptional, around 1 to 5%.7,8 The abdominal viscera (stomach, spleen, small intestine or colon) attracted by thoracic aspiration engages in the breach of 60% of ruptures of the left dome, immediately or after a delay of a few hours or even a few days.5,19 Overall mortality is high and varies from 3 to 60% depending on the series.20,21 It is related to associated injuries when it is part of a picture of polytrauma, to cardio-respiratory failure or to a surgical complication in the event of strangulation of organs aspirated into the thorax. Morbidity is approximately 40%. They are dominated by respiratory sequelae.20,21 Recurrences remain unquantified but are said to be rare. For our two patients, the evolution was favorable without any complaints over a 6-month follow-up.
The two cases we reported were in two young adult males following a road accident with direct impact to the thorax. The diagnosis most often requires a preoperative CT scan and diagnostic videothoracoscopy. For the two cases we reported, the diagnosis was strongly suspected preoperatively and confirmed intraoperatively. The treatment was exclusively surgical and consisted of suturing the defect following a laparotomy.
The authors declare that there are no conflicts of interest.

©2024 Boka, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.