Journal of
eISSN: 2373-6437


Case Report Volume 13 Issue 6
1Department of Surgical Medical Emergency, Hospital General Regional 02 IMSS Dr. Guillermo Fajardo Ortiz, México
2Department of Traumatology and Orthopedics Hospital General Regional 02 IMSS Dr. Guillermo Fajardo Ortiz, México
3Private practice, General Medicine, México
4Neonatal Intensive Care Unit, UMAE Hospital de Ginecología y Obstetricia Dr. Luis Castelazo Ayala, México
Correspondence: Dr Jorge Melchor-Amador, Hospital General Regional 02 IMSS Dr. Guillermo Fajardo Ortiz, Calz. de las Bombas 117, Coapa, Girasoles I, Tlalpan, 14310 Ciudad de México, CDMX, Tel 5536777923
Received: November 27, 2021 | Published: December 29, 2021
Citation: Melchor-Amador JR, Mota-González E, Amador-Ayestas SM. Polymerized type I collagen improves the mean oxygen saturation and efficiently shortens symptom duration and hospital stay in adult hospitalized patients with moderate to severe COVID-19: Randomized controlled clinical trial. J Anesth Crit Care Open Access. 2021;13(6):193‒199. DOI: 10.15406/jaccoa.2021.13.00495
Background: Abnormal blood-oxygen levels and breathing rates are strong predictors of poor hospitalized patient outcomes.
Objective: To evaluate the safety and clinical efficacy of intramuscular administration of polymerized type I collagen (PTIC) in adult hospitalized patients with moderate to severe COVID-19 on mean oxygen saturation and symptom duration.
Design, setting, and participants: This randomized, placebo-controlled clinical trial recruited 54 adult hospitalized patients with confirmed COVID-19 diagnosis from June 2020 to May 2021. Patients received intramuscularly 1.5 ml of PTIC (12.5 mg of collagen) or placebo every 24 h for seven days. The primary outcome was oxygen saturation >92% on room air without supplemental oxygen. The secondary outcome was the duration of symptoms.
Results: Twenty-two/54 (41%) were male, with a mean age of 43.5±11.9 years. Oxygen saturation >92% on room air without supplemental oxygen was achieved by 23/26 (89.0%) and 15/28 (53.6%) of patients under treatment with PTIC or placebo, respectively (P=0.010). Dyspnea, cough, and chest pain improved from day 4 of treatment vs. baseline (P<0.05). Hospital stay was reduced by 2.77 days in PTIC vs. placebo group (P=0.048). The Neutrophil-to-lymphocyte ratio (NLR) (predictive biomarker for moderate-severe COVID-19) decreased to statistically significant levels (P<0.001 and P=0.009, PTIC and placebo, respectively). No serious adverse events were detected.
Conclusion and relevance: In the study, 89% of the patients under PTIC treatment had mean oxygen saturation >92% compared to 53.6% in the placebo group. A shorter duration of the symptoms was determined. A significant decrease in NLR was found in post-treatment with PTIC. The study is limited by a small sample size and short follow-up duration, and determination of clinical efficacy would require larger randomized trials with more definitive outcome measures.
The pandemic of coronavirus disease (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the most significant global public health crisis during the last decades. As of August 13, 2021, Mexico has become the second nation with confirmed cases regarding SARS-CoV-2 related deaths in North America.1 It has been reported that up to 42% of hospitalized patients will develop acute respiratory failure/acute respiratory distress syndrome (ARDS) and require ICU admission, with an in-ICU mortality rate of 52%.2 The SARS-CoV-2 infection seems to trigger peculiar innate and adaptative immune responses. Profound lymphopenia and increased neutrophil-to-lymphocyte ratio are associated with clinical severity, and elevated serum levels of pro-inflammatory cytokines, also characterized as cytokine release syndrome, have been reported as potential mediators of respiratory/multiple organ failure.3 Thus, there is an urgent need to find anti-inflammatory drugs to mitigate inflammatory organ injury in viral pneumonia. Some immunomodulatory drug trials have been performed,4 such as the RECOVERY trial. It has been demonstrated that in hospitalized patients with COVID-19, the use of dexamethasone resulted in lower 28-day mortality among those receiving either invasive mechanical ventilation or oxygen alone.5 For this reason, the search for therapeutic strategies that modulate inflammation and avoid, as far as possible, the long-term sequelae of the infection is still fertile ground.
A potential drug for immune modulation is polymerized type I collagen (PTIC). It is a g-irradiated mixture of pepsinized porcine type I collagen and polyvinylpyrrolidone in a citrate buffer solution. At 37ºC and neutral pH, the molecule does not form a gel, like collagen. The covalent bond between the protein and the PVP modifies its electrophoretic, physicochemical, and pharmacological properties.6 The PTIC has been shown to induce negative regulation of pro-inflammatory cytokine production (IL-1β, TNF-α, IL-8, IL- 17, IFN-g, PDGF and TGF-β1),7 of adhesion molecule expression, ELAM-1, VCAM-1 and ICAM-1, of the enzyme cyclooxygenase (Cox) -1 through the modulation of the transcription factor NF-kB in inflamed tissues. Moreover, PTIC has been shown to induce positive regulation of IL-10 and regulatory T cells.8-17 The systemic effect has been determined by intramuscular or subcutaneous administration of PTIC to patients with active rheumatoid arthritis, as a therapeutic co-adjuvant with methotrexate (pilot and phase II studies), improving the count of swollen joints, morning stiffness, an ACR 50 in 57% of the patients and inducing remission in 30% of the patients. PTIC is safe and well-tolerated in long-term treatment, without adverse effects.13
This study was design to evaluate the safety and efficacy of intramuscular administration of PTIC in adult outpatients with moderate COVID-19.
Study design
It was an open randomized, controlled clinical trial in adult patients with moderate to severe COVID-19.
Participants
Fifty-four patients were recruited from the Hospital General Regional 2 del Instituto Mexicano del Seguro Social (IMSS) from June 2020 to May 2021. Trial candidates were identified when they were hospitalized. The diagnosis was based on suggestive symptoms (fever, headache, cough, or dyspnea, plus at least another symptom such as malaise, myalgias, arthralgias, rhinorrhea, throat pain, conjunctivitis, vomiting, or diarrhea) and a positive real-time reverse-transcription polymerase chain reaction result for SARS-CoV-2.
Individuals were asked to provide information, including demography (data of birth, job, educational level, previous contact with infected individuals, date of onset of symptoms, etc.), preexisting conditions (including a history of hypertension, diabetes mellitus, cardiovascular disease, cerebrovascular disease, hypertriglyceridemia, dyslipidemia, etc.) and symptoms. Exclusion criteria included hypersensitivity to PTIC or any of its excipients. All patients that have participated or were participating in other clinical trials, patients that have been admitted to the hospital prior to randomization, patients that have been discharged, or were planned to be discharged, pregnant or breast-feeding patients, patients with chronic kidney disease as determined by calculating an estimated glomerular filtration rate (eGFR), decompensated cirrhosis, congestive heart failure (New York Heart Association class III or IV), patients with cerebrovascular disease, autoimmune disease, cancer, multiorgan failure or immunocompromised (solid organ transplant recipient or donor, bone marrow transplant recipient, AIDS, or taking immunosuppressant biologic drugs). Patients without written informed consent obtained from the patient or the patient’s legal representative were also excluded. Patients were evaluated every day during the treatment by the physician.
Intervention
Participants received a dose of 1.5 ml of PTIC or Fibroquel® (12.5 mg of collagen) or placebo every 24 h intramuscularly for seven days. As concomitant therapy, the use of paracetamol and oxygen was only allowed.
Data collection
Epidemiologic, demographic, contact and exposure history, clinical presentations, laboratory tests, treatment, and outcome data were collected from inpatient medical records. Laboratory data collected for each patient included complete blood count, coagulation profile, serum biochemical tests (including renal and liver function, electrolytes, lactate dehydrogenase, D dimer, and creatine kinase), serum ferritin, and biomarkers of infection at baseline, 4 and 8 days (1-day post administration of the last dose of the medication).
Primary and secondary end points
The primary outcome was an oxygen saturation of 92% or higher on room air without supplemental oxygen. For secondary endpoints, a reduction of symptoms, by at least 30% compared with baseline on a scale of symptom severity (0 = symptom is not present, 1 = mild, 2 = moderate, and 3 = symptom is very severe), and the time to recovery, defined by discharge from the hospital were considered as clinically relevant.
The primary and secondary endpoints were measured using participants’ self-reported responses and corroborated by the physician evaluation at 8- (1-day post administration of the last dose of the medication).
Adverse events and serious adverse events were recorded each day via physician and participant self-report.
Ethical considerations
It was conducted in compliance with the Declaration of Helsinki [20], the Good Clinical Practice guidelines, and local regulatory requirements. All participants provided written informed consent before randomization.
Statistical analysis
A descriptive analysis of the sample was performed. Continuous variables are expressed by mean and standard deviations (normal distribution), median and range, and proportions for categorical variables. Mann-Whitney Rank Sum Test was performed to determine differences between groups for continuous variables. Wilcoxon signed-rank test was performed to determine differences intragroup for continuous variables. Statistical analyses were performed using the Sigma Stat 11.2 program (Aspire Software International, Leesburg, VA, USA). Data are P values less than or equal to 0.05 were considered significant.
Demographic and clinical characteristics
Fifty-four adult hospitalized patients with moderate COVID-19 were enrolled in the study. The patients' mean (±SD) age was 43.6 ± 11.9 (range: 18-73) years. Twenty-two patients (41%) of the population were male (Table 1). The most common coexisting conditions were systemic arterial hypertension (22.3%) and pneumopathy (10.8%). Thirty-eight percent of the patients were overweight (Table 1).
|
|
Baseline |
Post-treatment |
|||||
|
Characteristic |
All Subjects |
Polymerized type I |
Placebo |
P-value |
Polymerized type I |
Placebo |
P-value |
|
Comparability of randomized groups |
|
|
|
||||
|
Age (years), mean ± SD Median Range |
43.6 ±11.9 41 18 - 73 |
44.1 ±10.1 41 29 - 73 |
43.1 ±13.4 40 18 - 643 |
ns |
|
|
|
|
Sex, Male, n, (%) |
22 (41) |
12 (46) |
10 (36) |
ns |
|
|
|
|
Overweight, n, (%) |
11 (20) |
6 (21) |
5 (18) |
ns |
|
|
|
|
Oxygen Saturation |
|
|
|
|
|
|
|
|
pSO2<92% (%) |
20 (37) |
8 (31) |
12 (43) |
ns |
23 (88) |
15 (54) |
0.024 |
|
pSO2; mean ± SD Median range |
89.1±6.9 90 60 - 98 |
87.3±8.8 90 60 - 94 |
90.9±3.82 91 81 - 98 |
ns |
93.4±2.0 94 90 - 98 |
91.1±3.9 92 80 - 98 |
<0.001 |
|
Laboratory variables |
|
|
|
|
|
|
|
|
Complete blood count |
|
|
|
|
|
|
|
|
Leukocyte count (x10^3/µL), mean ± SD Median Range |
10.3±3.8 9.4 5.1 - 23.0 |
10.5±3.6 9.8 5.1 -17.7 |
10.2±4.0 9.1 5.2 -23.0 |
ns |
11.5±3.6 9.8 4.7 -17.4 |
10.4±6.7 9.1 5.1 – 39.0 |
0.040 |
|
Lymphocyte count (%), mean ± SD Median Range |
10.9±6.4 10.7 1.5 -30.7 |
9.9±6.0 10.0 1.5 – 27.3 |
11.9±6.7 12.7 2.0 – 30.7 |
ns |
16.7±6.1 16.5 3.1 – 45.8 |
21.7±11.0 20.1 1.7 – 40.0 |
ns |
Neutrophil count (%), mean ± SD Median Range |
71.0±14.4 71.1 41.5 - 95.6 |
74.9±14.7 75.8 41.5 – 95.6 |
67.4±13.3 70.2 43.0 – 88.1 |
ns |
71.1±10.6 69.6 47.0 – 87.0 |
65.3±12.2 64.9 42.1 – 95.0 |
ns |
|
Neutrophil-lymphocyte ratio (NLR), mean ± SD Median Range |
11.4±12.4 6.4 1.7 – 56.5 |
13.2±14.3 7.6 2.3 – 56.5 |
9.7±10.2 5.5 1.7 – 44.1 |
ns |
4.6±2.5 3.9 1.2 – 11.1 |
6.9±10.7 3.2 12.0 – 51.9 |
ns |
|
Ferritin (ng/mL) Mean ± SD Median Range |
801.1±1030.1 398.0 43.2 – 4100.0 |
907.3±1012.7 907.3 137.0 – 4100.0 |
661.6±1068.9 220 5.1 -23.0 |
ns |
757.0±1012.6 301.0 40.0 – 3450.0 |
443.3±934.2 128.5 50.1 – 3800.0 |
0.05 |
|
D-dimer (ng/dL) Mean ± SD Median Range |
1155.0±1637.5 536.5 50.0 – 7300.0 |
1171.2±1634.5 670.0 155.0 – 7300.0 |
1134.5±1698.4 306.0 50.0 – 5100.0 |
ns |
1696.6±2381.3 602.0 100.0 – 8300.0 |
1018.2±1748.0 248.0 57.3 – 5190.0 |
ns |
|
Summary of Comorbidities |
|
|
|
|
|
|
|
|
None n, (%) |
29 (54) |
12 (47) |
17 (59) |
|
|
|
|
|
One, n, (%) |
23 (42) |
12 (47) |
11 (39) |
|
|
|
|
|
2 or More, n, (%) |
2 (3.7) |
1 (4) |
1 (4) |
|
|
|
|
|
Clinical Comorbidities |
|
|
|
|
|
|
|
|
Hypertension, n, (%) |
6 (11) |
3 (12) |
3 (10) |
|
|
|
|
|
Diabetes, n, (%) |
2 (4) |
1 (4) |
1 (4) |
|
|
|
|
|
Congestive heart failure, n, (%) |
1 (2) |
0 (0) |
1 (3) |
|
|
|
|
|
Chronic respiratory disease (emphysema), n, (%) |
3 (6) |
1 (4) |
2 (7) |
|
|
|
|
|
Symptoms |
|
|
|
|
|
|
|
|
Dyspnea, n (%) Δ =100(Baseline-Post-treatment)/Baseline (%) |
54 (100) |
26 (100) |
28 (100) |
ns |
10 (4) 82 |
28 (100) 19 |
<0.001 |
|
Cough, n (%) Δ =100(Baseline-Post-treatment)/Baseline (%) |
54 (100) |
26 (100) |
28 (100) |
ns |
17 (65) 62 |
28 (100) -6.8 |
<0.001 |
|
Chest pain, n (%) Δ =100(Baseline-Post-treatment)/Baseline (%) |
54 (100) |
26 (100) |
28 (100) |
ns |
24 (92) 60 |
28 (100) 18 |
<0.001 |
|
Headache, n (%) Δ =100(Baseline-Post-treatment)/Baseline (%) |
54 (100) |
26 (100) |
28 (100) |
ns |
26 (100) 32 |
28 (100) 35 |
ns |
|
Rhinorrhea, n (%) Δ =100(Baseline-Post-treatment)/Baseline (%) |
54 (100) |
26 (100) |
28 (100) |
ns |
26 (100) 2 |
28 (100) 8 |
ns |
Table 1 Baseline demographic and clinical characteristics of the trial population and study endpoints
SD, standard deviation; ns, non-significant
Primary outcome
At baseline, mean oxygen saturation readings were 89.1 ± 6.9 (range: 60 – 98; Figure 1D). At day 1 post-treatment, mean oxygen saturation readings were 93.2 ± 2.04 (range: 90 - 98; P<0.001; Figure 1D) and 91.1 ± 3.9 (range: 80 – 98; Figure 1D); and the percentage of subjects with oxygen saturation readings ≥92% were 89.0% and 53.6%, for PTIC and placebo respectively (P=0.010; Figure 1D). The first statistically significant increase of oxygen saturation readings (Figure 1D) in PTIC was determined on day 2 of treatment. The PTIC significantly increases the odds ratio 5.750 times to reach the endpoint compared with placebo (P=0.024).
Secondary outcomes
Symptom improvement was evaluated every day and compared with baseline. Cough, dyspnea, and chest pain decreased at statistically significant levels during day 4 of PTIC treatment (Figure 1G, H, and I).
No differences in temperature, respiratory and heart rates, systolic and diastolic blood pressure were sound at baseline vs. every day of treatment of PTIC or placebo or between groups of treatment (Figure 1A, B, C, E, and F).
Patients in the PTIC group had a shorter time to recovery than patients in the placebo group (8.12 ± 1.70 vs. 10.89 ± 4.32 days; P=0.048).
Invasive mechanical ventilation, supplemental oxygen, hospitalizations, and deaths
All patients under PTIC or placebo treatment received oxygen without invasive mechanical ventilation (via nasal cannula or reservoir mask) for 7 weeks (3 to 15 L/min).
Two patients under PTIC treatment died six weeks post-treatment due to complications associated with pulmonary fibrosis and bacterial and fungal superinfection. In comparison, three patients of placebo treatment died on day 4 of treatment and at 3- and 7-days post-treatment due to acute adult respiratory distress syndrome.
Neutrophil-to-lymphocyte ratio (NLR)
At day 1 post-treatment vs. baseline, neutrophil count decreased in PTIC and placebo treatment (P<0.001 and P=0.009, respectively; Figure 1L).
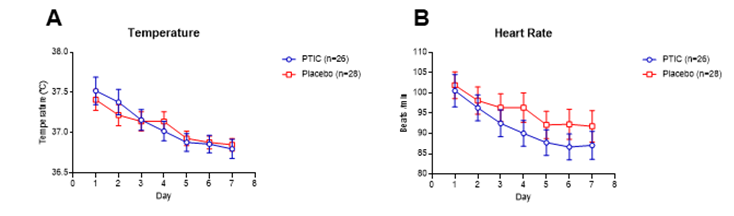
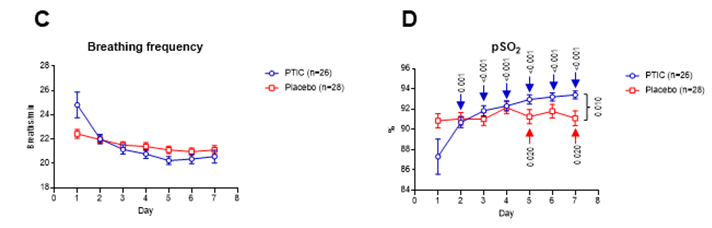
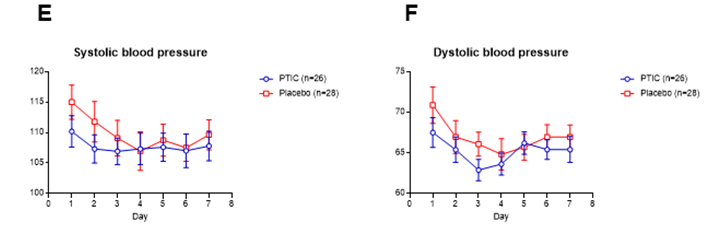
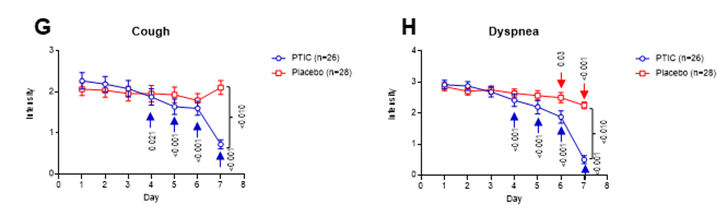
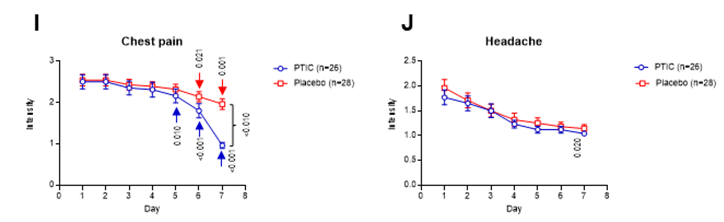
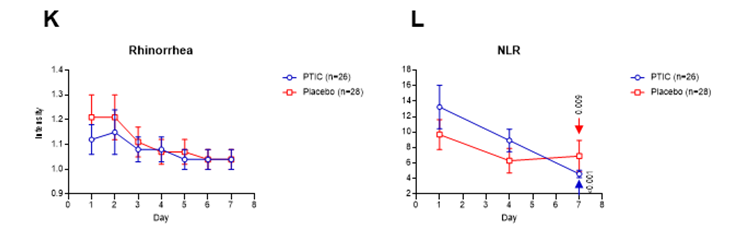
Figure 1 The intensity of symptoms during treatment of patients with symptomatic COVID-19 treated with polymerized type I collagen or placebo (PTIC). (A) Temperature, (B) heart rate, (C) breathing rate, (D) pSO2, (E) systolic blood pressure, (F) diastolic blood pressure, (G) cough, (H) dyspnea, (I) chest pain, (J) headache, (K) rhinorrhea, and (L) NLR index. The intensity of the symptom was evaluated on a 4-point rating scale (0 = without symptom, 1 = mild, 2 = moderate, 3 = severe). Blue lines represent the group of patients under polymerized type I collagen treatment (PTIC). Red lines represent the group of patients under placebo treatment. Results depict mean ± standard error of the mean. Blue arrows show the day when the treatment reached a P < 0.05 compared to the baseline for polymerized type I collagen treatment. Red arrows show the day when the treatment reached a P < 0.05 compared to the baseline for placebo.
Ferritin and D-Dimer
No differences in D-dimer levels were found among the PTIC and placebo groups at baseline (Table 1). Nonetheless, ferritin levels were higher in PTIC vs. placebo group (Table 1).
Medication at baseline
All patients were treated with acetaminophen, antivirals, antibiotics (azithromycin, ceftriaxone, clarithromycin, or levofloxacin), anticoagulants, and dexamethasone.
Adverse events
In the study, no serious adverse events were detected. PTIC was safe and well-tolerated during the study. Patients had pain at the application site lasting less than 15 to 20 min.
Intramuscular PTIC was associated with better oxygen saturation values when compared to placebo. Also, PTIC shortened symptom duration. On day 8 of treatment with PTIC, a higher mean oxygen saturation value and a higher proportion of patients retaining oxygen saturation values ≥92% were observed, as previously reported by Carpio-Orantes et al.18 This could be related to a decrease in dyspnea and chest pain, as well as cough. Similar results regarding long-term mean oxygen saturation value were reported by Méndez-Flores S, et al.19 An unadjusted accelerated failure time model showed that the PTIC group achieved the outcome 2.70-fold faster (P<0.0001) than placebo. Moreover, they have been described the down-regulation of the IP-10, IL-8, M-CSF, and IL-1Ra levels in the PTIC group vs. baseline and placebo group. Symptom duration in the PTIC group was reduced by 6.1±3.2 days vs. placebo. No differences in adverse effects were observed between the groups. Thus, the PTIC treatment down-regulated IP-10, IL-8, M-CSF, and IL-Ra levels could explain the PTIC effect on the higher proportion of patients with mean pSO2≥92% and a shorter duration of symptoms vs. placebo.19
It is important to mention that the treatment with PTIC decreased NLR in a higher proportion than placebo. NLR is a biomarker of inflammation progression that can be measured during routine hematology. Previous studies have exhibited that higher NLR is associated with clinical deterioration and mortality for COVID-19 patients.20 Thus, a decrease in NLR suggests a better outcome for patients treated with PTIC and indicates that the PTIC exerts a down-regulation of inflammation.
Based on the decrease of NLR in patients under treatment with PTIC, we infer that the medication fits with the profile of anti-inflammatory drugs, such as dexamethasone, colchicine, and Janus kinase inhibitors.5,21-24 Nonetheless, in contrast to dexamethasone, an immunosuppressor, PTIC is a down-regulator of inflammation. For this reason, we suggest that PTIC does not affect serum viral load or the risk of acquiring other infectious agents, water and salt retention, blood pressure, glycemia, muscle weakness, gastrointestinal bleeding, and psychological disturbances, as observed with corticosteroids.25 However, this must be confirmed in further studies. Moreover, PTIC was safe and well-tolerated.
Most COVID-19 patients show benign disease course where patients overcome viral inflammation by a robust but not overreactive immune response.26 The potential advantages of PTIC for symptomatic patients’ treatment of COVID-19 include its safety, low cost, and intramuscular administration.
Moreover, a 7-day course or PTIC was superior to the placebo in treating hospitalized patients with COVID-19. This benefit was seen in the number of days to recovery (mean, 8.12 days, compared with 10.89).
This study has several limitations. First, it was a small open study, and it was conducted within a single geographic area, so these findings should be regarded as preliminary. The study needs to be replicated in larger trials with a more heterogeneous study population. Second, there was a small number of endpoint events, which made the findings fragile. We did not collect information on virologic measures to prove that PTIC does not increase the viral load. Finally, if PTIC is determined to be effective for treating symptomatic COVID-19, the underlying mechanisms need further clarification.
Summing up, in this open-label study of adult hospitalized patients with moderate to severe COVID-19, PTIC was safe and had clinical efficacy for the treatment of hypoxemic COVID-19 patients.
The authors declare no competing interests.
The authors thank the patients who agreed to participate in the present study, all the employees involved in the treatment, follow-up, and implementation of this study protocol, and all the Hospital General Regional número 2 of the Instituto Mexicano del Seguro Social. We appreciate the participation and collaboration of the ALEPH Consulting & Data Science team.

©2021 Melchor-Amador, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.