Journal of
eISSN: 2373-6437


Research Article Volume 6 Issue 3
1Cork University Hospital, Ireland
2Consultant Anaesthetist, Beaumont Hospital, Ireland
Correspondence: Imran Azher, Cork University Hospital, Apt No 7 Rosehaven Castleknock, Ireland, Tel 00353-894501411
Received: January 04, 2016 | Published: November 30, 2016
Citation: Azher I, Arfin SN (2016) Perioperative Control of Temperature - An Audit. J Anesth Crit Care Open Access 6(3): 00229. DOI: 10.15406/jaccoa.2016.06.00229
Inadvertant perioperative hypothermia is a common complication of perioperative period and is defined as core body temperature less than 36 degrees celcius. Hypothermia may be classified into three categories
Mild hypothermia – 34-36degrees.
Moderate hypothermia – 30-34degrees.
Severe hypothermia- <30degrees.
Hypothermia can develop pre, intra and post operatively. The incidence ranges anywhere between 60-90% of all surgical patients and results when body’s ability to maintain normothermia is diminished by the absence of protective reflexes such as shivering and piloerection due to anaesthesia and loss of heat during surgery.1
In this study we included 40 patients, ranging from age 16-and above, between ASA 1 and 5, undergoing short, intermediate and long surgeries. The classification of surgeries was done on the basis of duration of surgeries. Surgeries lasting less than 30minutes duration were classified into short surgeries, surgeries lasting 30minutes to 1hr and 30min as intermediate surgeries and surgeries lasting more than 1hour and 30minutes were classified as long surgeries. Patients less than 16 years of age were excluded from the study. All the patients were randomly selected.
In our study we have found out that a temperature recording was taken in all the patients preoperatively, which was in accordance with the nice guidelines. About 27.5% of the patients were hypothermic prior to induction, and in none of these patients pre-operative measures were taken to combat hypothermia. Off these 27.5% patients who were hypothermic prior to induction, 81.8% remained hypothermic at the end of the operation. Of all the patients involved in the surgery, 45% of the patients remained hypothermic post operatively in the recovery. Intraoperatively warming measures were used in 90% of the patients. Only 10% of the patients did not get any intraoperative warming measures. These included forced air warming devices, warmed iv fluids, both combined or none.
In terms of efficacy of the warming device a combination of forced air warming device and warmed iv fluids seem to be the most effective. Only 27% patients remained hypothermic in the recovery. Off those patients who just received forced air warming device as a intraoperative heating measure, about 50% of the patients remained hypothermic.
When no warming measure was used, that was in two patients both of them remained hypothermic. We also audited the percentage of patients who were hypothermic at the end of the surgery depending upon the classification of surgery as short surgeries, intermediate and long surgeries. Short surgeries lasted less than 30 min, intermediate anywhere between 30min to 90min and long surgeries lasting more than 90 minutes.
In our audit 50% of the patients undergoing minor surgeries remained hypothermic at the end of the surgery, about 53.8% of the patients undergoing surgeries of intermediate duration remained hypothermic and none of the patients undergoing major surgery were hypothermic (Table 1 & Figure 1).
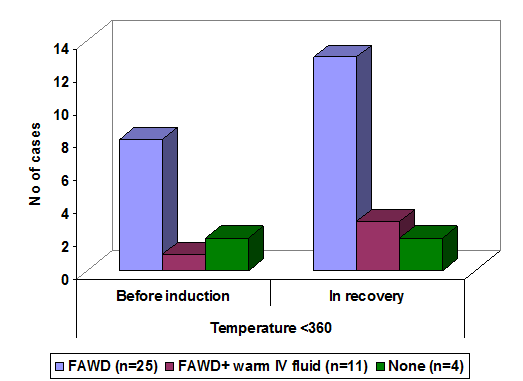
Figure 1 Showing temperature <360 before induction and in recovery according to method of worming in study group.
Methods of warming |
n |
Temperature <360 |
|
Before induction |
In recovery |
||
FAWD |
25 |
8 |
13 |
FAWD+ warm IV fluid |
11 |
1 |
3 |
None |
4 |
2 |
2 |
Total |
40 |
11 (27.5) |
18 (45) |
Chi-square |
3.14 |
1.93 |
|
P Value |
>0.05 |
>0.05 |
|
Table 1 Showing the patient numbers, the method of warming and the number of patients who were hypothermic prior to induction and the numbers that remained hypothermic in recovery
It is vital to maintain perioperative temperature within the normal accepted range. Inadvertent hypothermia is associated with a number of complications like increased risk of surgical site infections, delayed wound healing, which lead to increased hospital stay and increased cost to both the patient and the health service. We could like to compare our results with the NICE guidelines, which are the accepted gold standard.
Perioperative care
Preoperative phase
The preoperative phase is defined as the 1 hour before induction of anaesthesia, during which the patient is prepared for surgery on the ward or in the emergency department, including possible use of premedication. During this period, each patient should be assessed for their risk of inadvertent perioperative hypothermia and potential adverse consequences before transfer to the theatre suite. Patients should be managed as higher risk if any two of the following apply:
In our audit we have found that a risk stratification and the assessment of patients if they were high risk was not done in any of the patients. The patient's temperature should be measured and documented in the hour before they leave the ward or emergency department and If the patient's temperature is below 36.0°C, forced air warming should be started preoperatively on the ward or in the emergency department (unless there is a need to expedite surgery because of clinical urgency, for example bleeding or critical limb ischaemia). In our audit no preoperative forced air warming device was started in any of the patients who were hypothermic.
Intraoperative phase
The intraoperative phase is defined as total anaesthesia time, from the first anaesthetic intervention through to patient transfer to the recovery area of the theatre suite. The NICE guidelines recommended patient's temperature should be measured and documented before induction of anaesthesia and then every 30 minutes until the end of surgery. This was a norm in our centre and was done in all the patients included in the audit. Induction of anaesthesia should not begin unless the patient's temperature is 36.0°C or above (unless there is a need to expedite surgery because of clinical urgency, for example bleeding or critical limb ischaemia). This was not done in our centre. Patients who are at higher risk of inadvertent perioperative hypothermia and who are having anaesthesia for less than 30 minutes should be warmed intraoperatively from induction of anaesthesia using a forced air warming device. All patients who are having anaesthesia for longer than 30minutes should be warmed intraoperatively from induction of anaesthesia using a forced air warming device. The temperature setting on forced air warming devices should be set at maximum and then adjusted to maintain a patient temperature of at least 36.5°C.
All irrigation fluids used intraoperatively should be warmed in a thermostatically controlled cabinet to a temperature of 38-40°C. We did not look at this mode of warming the patient in our audit.
Postoperative phase
The postoperative phase is defined as the 24 hours after the patient has entered the recovery area of the theatre suite. The patient's temperature should be measured and documented on admission to the recovery room and then every 15 minutes. This is regularly done in our centre and was done in 100% of the patients in the audit. The NICE guidelines also recommend that Ward transfer should not be arranged unless the patient's temperature is 36.0°C or above. However we did not audit this in our study because it was logistically difficult to follow on the patients once they were in the recovery. The guidelines also recommend that the temperature should be measured and documented on arrival at the ward and every four hour hence forth. Our audit did not extend to beyond the operation theatres and the recovery and hence we failed to audit this.
None.
The authors declare there are no conflicts of interest.
None.

©2016 Azher, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.