Journal of
eISSN: 2373-6437


Review Article Volume 3 Issue 6
1Intensive Care Unit, Hospital General de Tijuana, ISESALUD, México
2Anesthesia and Intensive Care Unit, Hospital Angeles Tijuana, México
3Plastic Surgeon, México
4General Practitioner, México
5Facultad de Medicina, Tecnológico de Monterrey, México
Correspondence: Víctor Whizar-Lugo, Intensive Care Unit, Hospital General de Tijuana, ISESALUD, Av. Centenario 10851, Zona Rio, Tijuana B.C., México, Tel +52664-6848905, Fax +52-664-6848906
Received: November 26, 2015 | Published: December 30, 2015
Citation: Whizar-Lugo V, Flores-Carrillo JC, Campos-León J, Parra-Beltrán P, Azamar-Llamas D (2015) Perioperative Care of Tourist-Patients. J Anesth Crit Care Open Access 3(6): 00119. DOI: 10.15406/jaccoa.2015.03.00119
Medical tourism is an ancient activity that was recently reactivated. It is a multidisciplinary complex matter that involves governments and private health care as well as lay people interested in facilitating this activity. The beginning of the XXI century has enabled this phenomenon and mmedical tourists intentionally travel from their hometown to a different country to receive medical care. This growing international phenomenon has multiple legal, ethical, political, economic and medical facets. Minimal literature exists on this topic, including legal, ethics, cost, quality, postoperative care and complications for medical tourists. Anesthesia in these patients is a challenge that has not been properly investigated; it has many important aspects such as suitable pre-anesthetic communication, characteristics ofotherraces with a wide range of illness and pharmacological response, physiological changes during prolonged trips like DVT/PE, the possibility of surgical-anesthesia complications and many more. Numerous questions remain unanswered and there is a need to review our anesthesia techniques.
Keywords: medical-tourists, anesthesia care, medical facets, surrogacy, paramedics
Marco Polo was a tireless globetrotter that was able to get through big challenges for his time, an era in which being a traveler represented daily routine dangers. Now people are able to travel to outer space where the challenges to be overcome are fairly different. Today we travel to the furthest places on earth in a comfortable seat, air-conditioned, in a car, in a fast train, a bus or an airplane. Travelers arrive to their destinations and stay in luxurious places, with similar or better amenity that they have in their homes, eat safely cooked food, get vaccines against endemic diseases, watch the local traditions and rituals from safe places and occasionally interact a moment with them. When a traveler becomes a medical tourist the environment is different; they will meet a team of professionals with a different accent, maybe not in the same language, in some cases a translator will be needed, medical facilities with different architecture from the ones they have in their country, nurses and paramedics that don’t understand them when they need something, maybe even share a room with a local patient or another medical tourist case, the food may have different ingredients and flavors, the staff will have their own customs and places with different odors. When arriving to the operating room everyone will speak a language that they will not understand, and will receive mere sympathetic smiles trying to console them. This scenario will most likely repeat in the recovery room. Due to the rapid global growth of medical tourism, this has exceeded the expectations of the common tourist agencies, the administrators, the doctors, and also the governments. The legal aspects of this activity are not entirely clear; neither relevant medical study in the international scientific literature can be found.
Medical tourist-patients represent a significant challenge that has not been studied in anesthesiology. These are people that have traveled for hours, from other countries and that usually have not received a surgical or pre-anesthetic assessment. They must be evaluated in a fast and correct way to determine if they are in condition to go through the procedure they have traveled for. Frequently these patients have uncommon or unknown diseases for the local physician, although these medical condition do not contraindicate anesthesia, it can modify the perioperative pharmacologic management as well as the results in the short, medium and long term period of time.
We found no scientific information on this subject, so this review includes the most important aspects that the anesthesiologist should know about when tourist-patients that have traveled from distant sites undergo scheduled or urgent surgical procedures. The goal of this review article is to cover the lack of information in this growing field of anesthesiology by grouping the available concepts and our experience in a possible theoretical frame work.
Medical tourism is an activity as old as the practice of medicine. It comes from civilizations as ancient as the Sumerians, when around the year 4000 B.C. they recognized the curative properties of the hot springs and built locations to heal the sick in these places. In the bronze age, 2000 B.C. the tribes near the mountains of what today is Sank Moritz Switzerland, recognized the benefits of bathing in the hot springs rich in iron. In France and Germany there have been found tools like the ones found in Switzerland, linked to pilgrims between these places. The ancient Greeks where the firsts ones to settle the bases for a big medical tourism when they built temples in honor of the god of medicine –Asclepius- which became the firsts health centers, where people from the known world traveled looking for a cure of their illnesses. Another Greek example from the year 300 B.C. is the Epidaurus with gymnasium, snakes farm, temple of dreams and thermal baths. The Sanctuary of Zeus and the Temple of Delphi were other Greek sites where the pilgrims traveled pursuing for cure. India is another millenarian place where medical tourism has taken place for more than 5000 years; yoga and Ayurveda were the principal attractions that favored the continuous streams of pilgrims in the search of alternative cures, practice that continues to this day. The Roman Empire also contributed to medical tourism centers with their hot springs and hot water baths called thermals, which were popularized within the elite individuals as healing centers. The Middle Easth as a long and old history as a medical tourism destination; here is where the modern hospitals have their origin. At the beginning of the Islamic culture, in the year 1248 A.D. the Mansuri Hospital was built in Cairo, with a capacity of about 8000 people, and quickly became a healing destiny for thousands of foreigners, regardless of race or religion. During the Renaissance there were new places in Europe and the word SPA was created, from the Latin Salude per Agua, places like Ville d’Eaux and Town of Waters were famous throughout Europe in the XIII century when hot springs rich in iron attracted people like Peter The Great and Victor Hugo. In the XVI century the European elite rediscovered Sank Moritz, Ville d’Eaux, Baden-Baden, Aachen and other hot springs with curative properties. The post-Renaissance period also had medical tourism centers in England. In this period the French Michel Eyquem of Mantaigne created the concept of luxury trips and apparently also helped with the first guide of spas for medical tourism.7,8 The discovery of America brought new places for medical tourism where herbalist knowledge and multiple places with curative hot springs. The temazcal, a pre-Hispanic custom has been since then a form of traditional medical therapy in which they combine heat, water, medicinal plants, psychological equilibrium and, sometimes, mystical rituals that include a Chaman or quack doctor. Although this kind of thermal baths have been found in Canada, United States of America, Mexico, Guatemala and El Salvador, it constitutes a typical motive of medical tourism to Mesoamerica.9,10
In the 1960s the hippie movement that started in San Francisco, California gave origin to the first trips to the Far East, especially to India and countries in Latin-America, where these people and their homologues in Europe went looking for alternative ways of living that included yoga, Ayurveda, Vedanta, and herbal therapy.11 Among other products, the hallucinogenic mushrooms in Oaxaca, Mexico became world famous. After the 1980s, these events summed to the high costs of medicine in developed countries, forced patients to look for a cure outside of their countries. The XXI century began with a promising decade for this kind of activity, and has expanded practically too every health care related activity, including medicine and dentistry.
The search for diagnostic and treatment alternatives that patients and their families make today is motivated by multiple and varied reasons: from the lack of medical services in their place of residency, to the alternative non-orthodox medicine that offer miraculous treatments for terminal disease or chronic illness. Between these two poles exist an infinite of reasons that make people look for medical or surgical attention outside of their hometown; affordable prices, improved quality, payment plans, readiness attention, lack of resolute capacity, recommendations, and special offers by entrepreneurs, medical groups, freelance doctors, or hospitals with or without known prestige. In 2008, some insurance companies in United States of America considered the alternative possibility to offer non-urgent medical care in other countries, and some of these companies are considering medical procedures abroad as an integral part of the coverage plan, which would lower health care costs without deterioration of its quality.11,12
Medical tourism is a multimillionaire business which has motivated federal hospitals and private institutions to officially promote it.12 This hasfavored its growth and it is one of the reasons why in 1997 the Joint Commission International was created to check and certify the attention of medical tourists, based on the quality standards they have recommended. The exact number of medical tourists is unknown.8 For example, in 2007 there were about 300,000 medical tourists that travel from the United States to several countries in the world, in 2010 there were calculated more than 1,000,000 patients looking for some kind of medical service outside of this country,whileanestimate of 250,000 patients look for medical attention in this country. In the UK approximately 50,000 citizens look for medical attention outside the country, mainly for plastic, orthopedic, ophthalmologic and fertility surgical procedures. In 2004, the International Bumrungrad Hospital in Bangkok, Thailand received 400,000 medical tourists, from which 55,000 of them were American,13,14 Malaysia received 130,000 patients and India 150,000, a number that grows every year by 30%. Thailand receives around 400,000 medical tourists every year and Costa Rica about 150,000.15
Searching places for medical tourism
Modern medical tourism can be divided in two main periods: before and after the Internet. In the beginning medical tourism was limited to big medical centers in developed countries to which the tourist-patients traveled with plentiful economic support to have high risk procedures like cardiac, orthopedic, oncologic and organ transplant surgery. The Mayo Clinic in the United States of America is a traditional third level center that gets visits from people all over the world. Another group that existed for more than three decades are hospitals and clinics located in countries where it is legal to use non-orthodox treatments, especially for oncologic illnesses or incurable chronic diseases. A third group, of more recent formation, are the small clinics and second level hospitals that identified the profitable potential of tourists searching for a cure. This variety of medical tourism was promoted in a direct way from these centers, utilizing pamphlets, radio, television and other methods of publicity. An additional common method was the tourism promoters who were in chargeof the dissemination of thesehealing modalities. Word of mouth had a small percentage in the promotion of this kind of tourism.
With the creation of the Internet in the 1970s this form of marketing is now the most important way of promotion, that had grown exponentially, so patients have more options to choose from, making it easier to select where to go and receive medical attention. There are more than 3,250,000 websites dedicated to the promotion of medical treatment with a countless number daily visits. Lunt et al.16 described six kinds of websites:
Most of them have graphic information with photographs and videos, testimony of patients, blogs, virtual visits to the facilities and additional recreational sites. The prices of the offered procedures are part of the information, so are the qualifications of the medical staff, but rarely contain information on anesthesia. Other interesting topic is the medical tourism that exists between border cities located in developed and less developed countries. By example, the United States of America and Mexico, where the migration of medical tourists has been favored by the nearness, availability, quality, and reduced costs of the medical care. There are national and international societies that promote medical tourism. The International Society of Travel Medicine (http://www.istm.org/) integrates scientists, administrators, politicians, leaders, and lay people from different countries interested in medical tourism. These organizationshave courses, conferences and general information, but anesthesia issues are not discussedwithintheir meetings. The Journal of Travel Medicine that is published since 1994 has no publications on anesthesiafor medical tourist patients.
The concept of medical tourism
Medical tourism creates a broad environment with many ethical, legal, professional and administrative unanswered questions. It is an activity that has facilitated doctors, nurses, technicians and other health professionals from the non-developed countries to be trained in first world hospitals, and has positively impacted the health systems of the countries of destination. In general, the tourist-patients can be classified in 5 groups.12-14
Pre-anesthetic assessment
Pre-anesthetic evaluation is fundamental for every anesthetic procedure and must be done in all patients.20,21 In the traveling patients this assessment is more difficult because they are not able to meet their anesthesiologist with plenty of time, resulting in a pre-anesthetic evaluation made in a rushing environment when the patient arrives to the surgical facility or even inside the operating room, which predispose to inappropriate assessment increasing the probability of perioperative incidents. Sometimes the pre-anesthetic assessment is not even done, which is a fault to the safety of the patient. Due to the increase in the number of tourist-patients, the anesthesiologists must look for an appropriate moment and space to evaluate in a proper and meticulous manner these patients, while establishing an empathic patient-companion-anesthesiologist rapport. It is ideal that when the patient has already decided to travel to be operated, they ought to get a complete pre-anesthetic evaluation in their place of origin, or get in touch with the doctor that will be the anesthesiologist during the procedure. This communication can be achieved by mail, by phone, or by the Internet. The latter is preferable because in this way the patient and the doctor will have the document of assessment in their e-mails, and those can be printed to be part of the clinical record for subsequent uses. When these communication medium are used for the pre-anesthetic assessment, the anesthesiologist must ask everything he would normally inquire and the patient must answer broadly to these questions, with emphasis in the diseases and the pathologies more relevant of the site of origin. This conduct avoids unexpected surprises when the patient and the anesthesiologist physically meet in the definitive pre-anesthetic consult. Another cybernetic way to accomplish the pre-anesthetic assessment is through Skype. This modality is more dynamic, in real time and can be written, printed and added to the clinical record. With Skype you can also establish a voice conversation, with or without video, which makes it faster. This modality allows the patient and the anesthesiologist to meet each other and to establish a very similar medical-patient relationship similar to the traditional face to face interview.
All of these modalities to implement a remote assessment have the advantage of being able to detect if there is any medical contraindication to perform the surgery or the anesthetic procedure, and this can be treated in their patient’s place of origin, before they schedule their trip, avoiding unnecessary expenses and risks. The typical patient is the one that has chronic anemia, smokes, has diabetes mellitus, a heart or lung disease, chronic kidney failure, asymptomatic urinary infections, etc. There are uncommon pathologies that require anticipated preoperative preparation like the patients who take medications or herbal products that modify coagulation. The patients with addiction to drugs, hepatitis, or AIDS, requiring special treatment. One must never forget about the endemic diseases of the countries of origin like malaria, yellow fever, avian flu, dengue, typhus, to mention a few.
During the pre-anesthetic assessment the informed consent must be signed. This document does not protect us from a lawsuit, but it is an important normative part of the clinical record. It is recommended that the informed consent is available in English, inthe native language ofpatient, and in the language of the destination country.
Pre-anesthetic medication
The objective of the pre-anesthetic medication is to reduce anxiety, to give pre-emptive analgesia, to reduce the volume and acidity of the gastric secretions, to increase the tone of the inferior esophagogastric sphincter in order to reduce gastro esophageal reflux and the incidence of pre-anesthetic nausea and vomit, and also to facilitate cardiovascular stability during endotracheal intubation and during the whole anesthesia, as well as to reduce the amount of anesthetics.21,22 In order to achieve these objectives it is necessary for the pre-anesthetic medications to be administrated with enough time.
Types of surgery
The surgeries for tourists-patients include a broad list of procedures. The more usual are plastic, bariatric, cardiac, orthopedic, ocular, dental procedures, and fertility treatment as shown in Table 1. This kind of surgical treatments are divided in outpatient surgeries, cases were the patient goes to a recovery home/hotel the next day and a third group that includes the patients that must be hospitalized for several days. These options must be explained to the patients before or at their arrival, founded in a selective and meticulous analysis of the patient physical condition, kind of surgery, as well as of the surgical time.
Procedures |
Outpatient |
Short stay |
Hospitalization |
Intensive care |
Cardiac |
- |
- |
++++ |
++++ |
Obesity |
+++ |
+++ |
++ |
+ |
Ocular |
+++ |
++ |
+ |
- |
Orthopedic |
- |
+++ |
+++ |
+ |
Plastic |
+++ |
++ |
+ |
+ |
Dental |
+++ |
- |
- |
- |
Fertility treatment |
+ |
+++ |
+++ |
- |
Table 1 Surgeries and outpatient facility-hospital management for tourist-patients
Obesity surgery has been modified in the past 5 years when placement of a gastric band was the most common procedure, and its results have favored the growth of procedures such as the gastric sleeve and gastroyeyunal bypass, both laparoscopic procedures.23,24 In plastic surgery the most common procedures are liposuction with or without fat transfer of the sucked fat tissue, breast implants, facial rejuvenation surgery and body cont our procedures for people who have lost weight.24-26
Ambulatory and short stay patients. These patients are usually ASA 1 or 2, with minimal invasive surgery, with short or medium time duration (1-4 hours). The risk of anesthesia in patients with a normal physical condition is considered to be minimal; nevertheless, there are some studies that show that this is not entirely true, so these patients may have severe complications.27
Inpatient. This group of tourist-patients includes those with prolonged procedures or high risk surgeries because of comorbidities. The risks ofanesthesiaare higher thaninthe previous group.
Types of anesthesia
The role of anesthesia in tourist-patients has not been studied. In our experience we have found that the task of the anesthesiologist is as big as the responsibility of the rest of the specialists that take part in the whole care of these patients. Anesthesiology is a high risk specialty, and the probability of negative results exists for each patient. Anesthesia mistakes or incidents can be catastrophic, which would imply medical, legal, economic and administrative matters. When someone searches information in the Internet about the anesthesia techniques for surgical procedures for tourist-patients, will only find vague data that mention if the procedure is made with general anesthesia, local anesthesia or even with no anesthesia. At other times the surgeons tend to give information about the anesthesia based on the scheduled surgery and not on the pre-anesthetic evaluation, frequently without considering the real anesthetic risk. The patients get an idea that can be either correct or incorrect, but when we have to modify this belief about the ideal type of anesthesia, the patients can be reluctant to change, arguing the mistaken information they had received. The information and choice of anesthesia management must be made by the anesthesiologist and based on the aspects that we use when we approach our local patients: a) ASA physical state, b) type and duration of surgery, c) type of hospital or surgical facility d) experience of the anesthesiologist. This decision will be influenced by other specific aspects of each tourist patient like:
Post-anesthetic recovery
In many outpatient surgery units and short stay facilities there are not sufficient equipment and staff to take care of the post anesthetic recovery area, which often endangers the lives of these patients. The guidelines for these sites mentioned mandatory minimum equipment, personnel and drugs, although there are countries were this type of medical facilities are not even regulated. It is extremely important that these areas are adequately monitored, including continuous ECG, noninvasive blood pressure, pulse oximetry and capnography. It is desirable to have the ability to provide ventilatory support as seen in the Figure 1. Similarly, there should be nursing and anesthesiologist staff dedicated only to take care of these patients. Another aspect is the optimal transport necessary for complicated patients, which should be available to carry patients to be treated –if necessary- in nearby hospitals (Figure 1).

Figure 1 Morbid obese patient with a difficult airway. The intubation could not be performed with the available equipment (endotracheal tube, laryngeal mask, combitube). She was kept with non-invasive ventilation until full recovery. The surgery was postponed and was later intubated with the help of a bronchoscope. With permission from www.anestesia-dolor.org
The immediate recovery must be evaluated by the anesthesiologist or a trained nurse using scales such as Aldrete32 or White et al.33 At the time of discharge from recovery room it is vital to use scales that meet theelements mentioned intable.31 An anesthesiologist or trained nurses are responsible of assessing the patient and certifying that they fulfill the criteria for discharge. In cases when there is doubt, the patients must be retained or sent to a hospital; the patients with a moderate or severe bleeding, with intense nausea or vomit, uncontrolled post operatory pain, prolonged surgery (>4 hours), liposuction of more than 6 litters, or major surgery are candidates to stay in hospital/surgery facility for more than 24 hours. The patients who travel alone, even though the conditions are optimal for recovery from an outpatient surgery facility must be considered possible candidates to stay in the surgical facility or with a nurse in the place where he/she is going to recover, it could be a hotel or a post operatory recovery house.
Anesthetic complications
Anesthesiology is one of the medical specialties with greater technological and pharmacological advances, while it is also considered as high risk for both the professional and the patients. The anesthetic complications become even more important in tourist-patients as these people are far away from their home and a peri anesthetic mishap can mean drastic changes in the patient-family-friends planthat has been developed; from expensive hospital costs, high costs due to delays in the return trip, even death. The image 2 corresponds to a tourist-patient who traveled 6198 km and developed incidental post operative irreversible cortical blindness (Figure 2).
Complications from anesthesia obey four different issues;
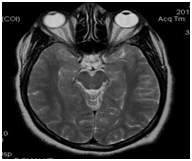
Figure 2 MRI showing post-anesthesia-surgery cortical edema in a tourist-patient. The blindness was permanent. With permission of www.anestesia-dolor.org
The morbidity and mortality rates are approximately the same in countries that have a similar life expectancy. The anesthetic community of a given country reduces its anesthesia morbidity and mortality data to an acceptablerange for their societies using techniques according to their medical culture and historical traditions,34 a situation that is not expected by the medical tourists who travel from a first world country withreduced anesthesia and surgery morbidity to an undeveloped country with a higher rate of post-anesthetic events. Preventive measures are mandatory to lower complications of anesthesia and must regulate our professional activity to bring down our statistics on morbidity and mortality.35
Specific problems
The anemic patient: We are used to anesthetize patients with normal values of hemoglobin and hematocrit and reject those cases with anemia, a conduct endorsed by the official norm/guidelines of most anesthesia societies. However, we know that anemic patients with cardiovascular stability can be safely anesthetized, which has questioned the magical figures of normality in these parameters in surgical patients. A group of tourist-patients have anemia associated to their underlying disease, by example the patients with history of bariatric surgery,26 chronic kidney failure, sickle cell disease, and the ones with extreme diets to lose weight, to mention a few. These patients with mild or moderate anemia can be operated electively. In the post-operatory period be treated with iron, folic acid, and erythropoietin to avoid blood transfusions. The recovery may take longer and this mandates a longer stay in a foreign country. The regulation to use blood restricts the direct purchase in some countries. On the other hand, there is a possibility of acquiring some blood transfusion related diseases, even if the risk is low, it continues to be a global threat, especially for hepatitis C,36,37 so blood-salvage techniques are strongly recommended.
Recent prolonged trips: Most of the tourist-patients travel long distances by airplane, car, train, or boat, which may favors the asymptomatic formation of blood clots in the inferior limbs and/or pelvis, especially when traveling by airplane. This condition hasbeen well describedand named economy-class syndrome or travel thrombosis.38,39 Deep vein thrombosis (DVT) and pulmonary embolism (PE) are related to prolonged flights of more that 6-9 hours and this is more obvious in flights longer than 12 hours. Although there are insufficientdata to determinethe true incidence of DVT/PE, an increase reports regarding flight induced medical incidents has occurred.40-42 There are few reports ofparadoxical embolism through an intra-cardiac communication.43 Some groups have described guidelines and recommendations for reducing this remote possibility.44,45 These patients arrives to the hospital or surgical facility a day before or even the same day of their intervention after a long tiresome travel, fatigue, with prolonged fast, wanting to sleep and frequently with time zone change that affects their circadian cycles.46 Almost 2 billion people use commercial flights each year and most of them do not know the potential medical risks associated with long trips, some of them facilitated by the cabin ambient and physiologic factors that favor mild hypoxia and gas expansion, which can predispose flares of chronic diseases and later be related to medical events during or after the flight,47 or throughout the surgery-anesthesia procedures. Randomized studies with ultrasound showed a measurable trend to asymptomatic DVT in the lower limbs after prolonged flight, condition that is reduced with elastic compression stockings. DVT are more common during the first week after the flight and the risk disappears after the second week. The calculated risk is 2-4 times greater in long distance travelers when compared to non-travelers, even though the average absolute risk is very little (approximately 1 event in 2 million travelers with a mortality of 2%). Traveling in economy class or first class apparently doesn’t affect this probability. Other factors that predispose to DVP/PE during long flights are being female, use of contraceptives, recent surgery or trauma, previous thrombotic events, venous insufficiency, pregnancy, overweight, older age, and thrombophilia. Gallus48 mentions the theoretical possibility that patients with Factor V Leiden and mutation in the prothrombin gen are at a higher risk to develop DVP or PE than normal people. However there are not enough studies to establish the potential risk of these patients. The hereditary thrombophilia are more frequent in white non-Hispanic, although they are present in other races as well. In Latin-American people with previous DVT or PE this mutations may be present in up to the 8%.49 Recently we observed two tourist-patients with Factor V Leiden, one of them developed PE after surgery.50 The physical factors related to these events are prolonged venous stasis associated with long periods of immobility, exposure to cabins with low humidity, and low concentrations of oxygen.51 During the process of establishing a medical program for this patients it is important to instruct them to stick to the prophylactic guides to prevent DVT and PE that airlines recommend like performing exercises with their feet and legs, walk frequently through the cabin alleys, as well as using adequate elastic compression stockings, avoid alcohol and dehydration during the flight. The importance of DVP/PE in short flights or in prolonged trips by car, train o boat is unknown.
Fomites: It has been shown that people with long hair, wigs or hair extensions are polluting factors to water pools52 and may have a role in the transmission of infectious diseases, a principle that is valid for this type of tourists patients in the operating room (Figure 3), in particular those having several days without cleaning their hair. This possibility of contamination has not been studied and is not usual considered as a potential risk for infection, even in surgery of the head, face or neck.

Figure 3 Two Afro-American patients with hair extensions, which act as a reservoir for bacteria and may contaminate the surgical site and recovery room. With permission of www.anestesia-dolor.org
Sexual preferences: Sexual preferences are other current issues that should be considered and respected by the entire health care team. Inappropriate comments about it are negative and represent a violation of the patient’s rights. Aesthetic and sex change surgical procedures in this group of people have been growing in many countries. Medical tourism team, including the anesthesiologist, is obliged to respect and work with these patients appropriately. As with other patients, we should perform tests for sexually transmitted diseases, if the results are positive it is required to take special precautions to avoid accidental infection of the medical and paramedical staff. In some countries these tests require patient. The positivity of these tests is not a reason to reject these patients.
Race and pharmacological response:It has been shown diverse pharmacological responses related to the human race; it is not the same anesthetize a Caucasian patient using the same drugs with as Hindu, a Latin American mestizo, a Native American, an African American, or Asian person. There are many pharmacogenetic studies comparing pharmacological responses of hundreds of drugs, many of which have a variability of response where genetic factors are involved according to different ethnic groups.53,54 These has been demonstrated in anesthesia and analgesia, where pharmacological responses may vary from one ethnic group to another.55 For instance, Dahaba56 demonstrated that rocuronium has a different potency and duration in Australian, Chinese, and North American patients. Vale and Delfino57 mentioned that Afro-American patients have a decreased topical effectiveness of local anesthetics (EMLA), an increased hypnotic effect of propofol and greater toxicity to acetaminophen, decreased hypotensive effect of the antihypertensive drugs related to renin, a lesser response beta2 antagonist, among some other pharmacological differences. Several investigators have found that black Senegalese African and Brazilians take longer to wake up than Caucasian when propofol-fentanil are used.58,59 Cepeda et al.60 studied the response to intravenous morphine in Caucasian, USA native Indian and Latin-American and found that natives Indian were more susceptible to morphine depressor effects; nevertheless the Latin-American and Caucasian had more elevated levels of morphine-6-glucoronide. There are sporadic reports of redheads having a greater incidence of surgical and anesthetic complications, however a recent review of the literature showed that the phenotype of this people can grant them a greater requirement of anesthetics, without a higher risk.61
Airway management: Difficult airway can be a problem if not previously diagnosed and properly managed. There are several algorithms for proper handling of these cases; ASA guideline is widely known the most complete and has frequent updates. When difficulties are anticipated to properly secure the airway it is necessary to have all the equipment necessary to warrant a successful management, as well as at least two trained anesthesiologists. Figure 4 shows a morbidly obese tourist female patient in which we failed to secure the airway at the first time. The patient was rescheduled one month later and intubated with difficulty using a flexible bronchoscope (Figure 4).

Figure 4 Morbid obesity with difficult airway. We were unable to secure the airway with the available devices (endotracheal tube, laryngeal mask, Combitube). She stayed on noninvasive ventilation in the recovery area. Surgery was postponed and she returned a month later. The patient was intubated with difficulty using a bronchoscope. With permission www.anestesia-dolor.org
The remote possibility of malignant hyperthermia should always be asked during the preanesthetic assessment. It is ideal to have dantrolene, or at least to have it available in the near hospital. Although it has been shown that regional anesthesia is safe in these patients62 there is a remote possibility of malignant hyperthermia. In many countries there is no dantrolene or it is very difficult to acquire it, so preventive measures should always be taken.
Specific challenges
Anesthetize tourist-patients means facing important challenges, sometimes even more difficult than the anesthesia procedure itself. As physicians, it is our obligation to be part of a friendly environment for these people who have traveled thousands of kilometers in search of improving their health or physical appearance. The psychological conditions, fear of the unknown, the possibility of failure of the medical team in a distant country are just some topics that we must always consider. The language is by far the first challenge. Most medical tourists come from English speaking countries or places where English is a second or third language, which forces us to speak and understand this language; the betterwe communicatein their language, better comprehending them, which earnsus the trustof patients.We must remember that it is our obligation to establish this communication and not the responsibility of the tourist-patients to speak our language.
Absolute respect to their believes and customs is another facet we ought to consider. The migrants from the middle east, the far east, the former Soviet Union, Africa, and other places that have arrived to the English speaking countries not only have they preserved their customs, their religions and ancestral believes. But they also kept their diseases (sickle cell disease, hereditary thrombophilia, porphyria, mitochondrial diseases, myopathies, etc.), The Muslims that live in the English speaking countries represent a typical group with different customs and believes compared to western societies.
Another challenge is the long term follow up of these patients. As anesthesiologists we should know the immediate, mediate and long term evolution of these cases as a matter to improve our anesthetics procedures. Unfortunately the anesthesiologists rarely have an opportunity or interest to follow this type of patients, so it is wise to establish communication from the moment of the preanesthetic visit until patients have returned to their country of origin. The Internet is by far the most feasible way to determine the outcome of tourist-patients. A particular challenge is to anesthetize tourist-patients with maladies that we are not familiar with. When a patient has this situation, it is mandatory to know about the disease and its plausible interactions with the anesthesia; since the disease itself or the medications the patient takes to control it may interfere with our management. It doesn’t matter if the surgery is delayed. Figure 5 shows a patient with Meleda’s disease, a hyperkeratosis of palms and feet, a very rare disorder that can be accompanied with severe cardiac alterations, including sudden death.63

Figure 5 Morbid obesity with difficult airway. We were unable to secure the airway with the available devices (endotracheal tube, laryngeal mask, Combitube). She stayed on noninvasive ventilation in the recovery area. Surgery was postponed and she returned a month later. The patient was intubated with difficulty using a bronchoscope. With permission www.anestesia-dolor.org
Bad results. As anesthesiologists we have the obligation to watch for the wellbeing of our patients, but occasionally the results can be catastrophic. What should we do when there is a malpractice problem? When the quality of care is not appropriate and a lawsuit is possible? Where would the trial be? How long do we have to answer the malpractice claim? Is there the possibility of an international lawsuit? Does our malpractice insurance covers these cases? These are some of the questions we may be asked in the case of an anesthesia catastrophe (Figure 5).
Relationship with the surgeon and the rest of the healthcare team
The medical staff, paramedics, and administrators that attend these types of patients must work as a perfect team to keep the safety of each patient -this is the main goal- besides the results from the surgery. The ethic and professional attitude of the healthcare team is the only way to give results of excellence in a modern hospital environment with first class equipment.64,65 The anesthesiologist is only a part of the human team and must be professional that follows the rules and guidelines of a certified practice, at the time that he or she becomes a vigilant of the rest of the team to make sure that everyone follows these rules.
The professional responsibility is shared in all of the procedures performed during surgical interventions: things as simple as the placement of a nasogastric tube in bariatric surgery can produce catastrophic situations if they are not performed in a correct manner.66 It is necessary to avoid vicarious liability between the medical staff and the rest of the personnel that participate in the care of patients, in order to avoid responsibilities of another person, especially when non trained personnel exist. The vicarious responsibility has been reported between surgeons and anesthesiologists because of negligence of one of them.67
Medical tourism is part of the globalization of health care that had its beginnings in ancient times and has gained great importance these days. These are people who have traveled great distances, have been vaccinated when it was required, they obtained a visa, overcame their anxieties and reach the doctor at the chosen site in search of healing or a better looking. They give us the opportunity to provide anesthesia services to people with different nationalities, different customs and diverse diseases to which we are used to treat in our local patients. This unusual environment makes us reassess own standards of care, to improve safety measures, and to adjust our methods of anesthesia placing always their safety at first. The safety of the surgical tourist-patient has several facades: the patient, the characteristics of their trip, the site of intervention, the procedure, the surgeon, the anesthesiologist, and especially the post operatory care. Every one of these elements has a specific role in the whole process of warrantying the success of the medical intervention, independently from the surgery. Patients are afraid of anesthesia more than surgery, so it is mandatory to be involved in the care of each tourist-patient who visit us in our workplaces, and give them confidence and professional service of excellence.
None.
None.
None.

©2015 Whizar-Lugo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.