Journal of
eISSN: 2373-6437


Research Article Volume 4 Issue 1
1Classified Anaesthesiologist, Department of Anaesthesia & Intensive Care, Bangladesh
2Advisor in Anaesthesiology, Department of Anaesthesiology, Bangladesh
Correspondence: Md Rabiul Alam, Classified Anaesthesiologist, Department of Anaesthesia & Intensive Care, Bangladesh, Tel 8801769000737
Received: August 19, 2015 | Published: January 7, 2016
Citation: Md Rabiul A, Md Mozibul H (2016) Off-Site Airway Management: Life-Saving or Life-Threatening? A Review of 74 Incidences. J Anesth Crit CareOpen Access 4(1): 00127. DOI: 10.15406/jaccoa.2015.04.00127
Introduction: Anaesthesiologists are considered as airway management experts in medical practice. They are frequently called upon to manage the airway of the suddenly critically ill patients at places outside the operation theatre (OT).
Objectives: It is intended to share the events, difficulties faced and to assist the newer anaesthesiologists in maintaining airway of critical patients at venues other than OT.
Methods: This retrospective observational study is done on 74 off-theatre emergency airway management calls attended at Combined Military Hospital (CMH) Dhaka, Bangladesh within a period over 6 months.
Results: Over 50 to 80 year-old age-group of both sexes was predominant (27%). Calls were mostly attended at Emergency & Casualty (32.4%) during indoor duties. Total off-hour calls were 64.9% and least but most serious calls were at dawn (10.8%). Emergency intubations were required for patients at or impending cardiorespiratory arrest (19%) due to head injury (14%), cerebrovascular accidents (11%) and massive myocardial infarction (2%). Requirement of airway management during non-surgical/interventional and imaging procedures was 21%. Observations revealed that more preparedness, availability of necessary armamentarium and efficient assistance are yet to develop at the vulnerable sites of the hospital to avoid a potentially disastrous emergency “Can’t Intubate, Can’t Ventilate” scenario.
Conclusion: The incharges concerned have to ensure the availability of properly equipped airway management tools and drugs in various wards and clinical procedural suites. Ward nurses and paramedics are to be made efficient enough and familiar with the management protocol by regular bedside hands-on training.
At extremely critical scenarios, anaesthesiologists are considered as airway management experts in medical profession. In addition to their anaesthesia practice, they are frequently called upon to manage the airway of the suddenly critically ill patients at places outside the operation theatre (OT).1 They are also often assigned to provide monitored anaesthesia care or conscious sedation during various medical interventional and radiological imaging procedures. The situations in those areas are obviously less well-controlled and unfamiliar to them than that of in the OT. Although the rescuing protocols are definitely lifesaving for the victims, but sometimes may become disastrous and life-threatening due to unpreparedness, equipment failure, poor assistance and ineffective over-try.2 So, quick assessment, right decisions and purposeful actions are to be taken very rapidly with accuracy in these scenarios.
This retrospective observational study was done on 74 events encountered by the author while attending the emergency calls for airway management of the critically ill patients outside the OT at CMH Dhaka over a period of 6 months. The venues were: Emergency & Casualty, Medical and Surgical HDUs, during patients’ transportation by ambulance, Radiology department, Endoscopy suites, Catheterisation Lab, Coronary Care Unit and different wards. The scenarios, difficulties faced, actions taken and recommendations are tabulated and narrated descriptively.
The demography of the patients is shown in Table 1. The age variation was from new-born to over 80 years of both sexes. Over 50 to 80 years old age-groups were predominant. Figure 1, Table 2 and Figure 2 are showing the preponderances of venues, timings of emergency calls and diseases of the critically ill patients respectively. Calls were mostly attended at the Emergency & Casualty (32.4%) while on duties. Office hour’s (0800 AM - 1430 PM) calls were 35.1% and the total off-hours’ calls were 64.9%. Least but most serious calls were at dawn hours (10.8%). Emergency intubations were required for patients at or impending c ardiorespiratory arrest (19%) due to head injury (14%), cerebrovascular accidents (11%) and massive myocardial infarction (2%). Requirement of airway management during non-surgical/interventional and imaging procedures was 21%. Difficulties faced, actions taken and recommendations are summarised and narrated in Table 3.
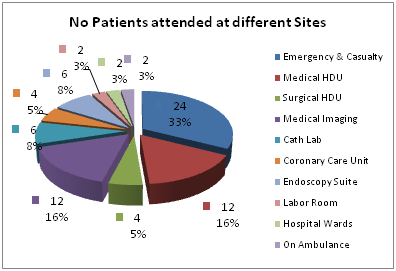
Figure 1 Pie-chart showing the number & percentages of patients attended at different sites. Note: Data of Critical Care Centre is excluded.
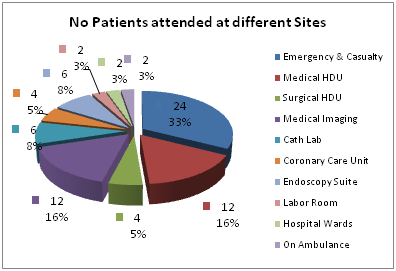
Figure 2 Doughnut-chart showing the diseases of the patients attended for emergency airway management.
Sex/Age |
Age Groups (Years) & % |
||||
0–1 |
02-Dec |
13-50 |
51 -80 |
Over 80 |
|
Male (n= 40) (54%) |
4(5.4%) |
8(10.8%) |
6(8.1%) |
12(16.2%) |
10(13.5%) |
Female (n=34) (45.9%) |
2(2.7%) |
10(13.5%) |
8(10.8%) |
8(10.8%) |
6(8.1%) |
Total (n=74) |
6 (8.1%) |
18 (24.3%) |
14 (18.9) |
20 (27.0%) |
16 (21.6%) |
Table 1 Demography of the critically ill patients for whom the emergency airway management calls were attended outside the operation theatres
Times |
At dawn (5:00-7:00 AM) |
Office hours (8:00AM-2:30PM) |
Evening (2:31-11:00PM) |
Midnight (12:00PM-2:00AM) |
Late night (2:00-5:00AM) |
Calls |
8 |
25 |
19 |
12 |
10 |
(n=74) |
-10.80% |
-35.10% |
-24.30% |
-16.20% |
-13.50% |
Table 2 Timings of the Emergency Calls for Airway Managements
Situations/Difficulties faced |
Actions taken |
Recommendations |
Rescuers are more busy with ventilation rather than effective chest compressions in case of cardiac arrest victims |
Appropriate importance given simultaneously to ventilation and purposeful chest compressions |
Recent and updated protocols for CPR (C-A-B) to be trained and practiced regularly by the health caregivers |
Stomach of patient is distended with gas due to improper/over-enthusiastic bag-mask ventilation/without using airway |
Correct AMBU support given using appropriate airway. N/G tube inserted immediately where possible |
Ward nurses and paramedics are to be trained and familiar on proper procedures of bag-mask ventilations using appropriate sized airway |
Intubation trolley and required drugs are not ready properly |
Tried to manage those instantaneously |
Everyday regular morning check is to be practiced |
Plates of the beds at the head-ends are not negotiable |
Adopted the improvised position of the patient with difficulties |
Provision for detachment of head-end plate of all hospital-beds is required |
Suction facilities on the spot is not available or not functioning properly |
Arranged quickly and managed |
Regular check-up and maintenance is necessary |
Unavailability of different sizes of ETT, stylet; larygoscopes light failure, cuff-leakage, lack of efficient assistance are not very uncommon |
Tried to manage, used the alternatives with difficulties |
Regular morning check-up drill in every wards has no alternatives |
Table 3 Situations/Difficulties faced, actions taken while attending the calls for emergency airway management outside the operation theatres and recommendations
At least one in four major airway events in a hospital are likely to occur outside the OT; i.e., in ICUs, Emergency & Casualty department, HDUs and at other venues.3 The outcome of these events is particularly adverse. Analysis has identified repeated gaps in care are: delayed identification of the patient’s at-risks, poor or incomplete planning, inadequacy of skilled staffs and equipment to manage these events successfully, and failed rescue due to lack of or failure of interpretation of capnography.4
Airway management outside the OT may be required for:
Airway assessment protocol and difficult airway algorithm have been formalized by the American Society of Anesthesiologists (ASA), which is revised periodically.6 The basis of the assessment is evaluation of factors that may hinder the displacement of the soft tissues of the mouth and neck and thus obscure the laryngoscopic view of airway. The full assessment requires evaluation of teeth, mouth opening, jaw, neck movement and deformities, but should take less than 2 minutes with regular practice. Approaches after assessment7 are:
In a hospital environment, all clinical nursing areas should have a resuscitation trolley consisting of the equipment for emergency airway management. The list of necessary equipment may be as in the Oxford Airway Box8 as following: suture materials, needles, cannulas (peripheral and central), syringes, gauzes, swabs, scalpel, dressing pack (galipot, drapes, needle holder, forceps), lubricants, gum elastic bougie, pen torch/headlight, suction catheters, Yankauer sucker, oro- and nasopharyngeal airways, varieties of ETTs with stylets and LMAs, percutaneous tracheostomy set, cricothyrotomy kit, AMBU bag capable of delivering 100%oxygen, functioning laryngoscope with a variety of blades, and drugs including adrenaline, lignocaine, atropine, glycopyrrolate, sedatives and musclerelaxants. In an urgent, rather than an emergency situation, a fibreoptic bronchoscope (FOB) may be obtained.
An adequate IV access is to be established first, as hypotension is a common consequence following intubation and inotropes may require. Measures to prevent aspiration is obligatory. In case of difficulties or failing, persistent attempts of laryngoscopy should be avoided. Intermittent oxygenation by a facemask with continued application ofcricoid pressure should be performed to prevent significant desaturation (<95%). Visualization of the larynx may be improved by changing the size and type (Macintosh to Miller) of laryngoscope blade and externally manipulating the larynx using the BURP (backward, upward, rightward pressure) manoeuvre.9
The most certain confirmatory test of successful endotracheal intubation is visualization of the tube as it passes through the vocal cords. Tube misting and auscultation may be useful but are not reliable.10 Visualization may not always be possible and other confirmatory tests have been employed. The most widely used tool in the OT is capnography, but unfortunately this facility may not be available at the off-sites. Other method is visualization of tracheal rings and carina using an FOB, but this scope may not be readily available.11 Both the cuff palpation and trans-illumination with a light wand have been used, but neither is superior to auscultation. Auscultation is substantially inferior tocapnography.12 Direct visualization with a laryngoscope or FOB thus remains the gold standard of confirmation.
Emergency airway management at any site is lifesaving for the moribund patients in clinical practice. Although the consequences are not so optimistic with pre-existing irreversible massive organ damage instead of following all prescribed protocols meticulously. But, the rescue measures unfortunately may become sometimes life-threatening due to improper assessment, actions and futile over-try in difficult scenarios. Moreover, off-theatre circumstances are often revealed quite odd and unfamiliar to the caregivers. Therefore, proactive preparedness, early detection and referral, correct decisions, purposeful actions and trained assistance are solicited for better outcomes.
None.
None.
None.

©2016 Md, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.