Journal of
eISSN: 2373-6437


Review Article Volume 10 Issue 4
Anesthesiologist, Pain Fellow, Milad Hospital, Iran
Correspondence: Helen Gharries, Anesthesiologist, Pain Fellow, Milad Hospital, Sattarkhan, District2, Tehran Province, Iran, Tel +989129306577
Received: June 20, 2018 | Published: July 23, 2018
Citation: Gharries H. Is ultrasound guided spine injection safe? J of Anes & Criti Care Open Access. 2018;10(4):131-138. DOI: 10.15406/jaccoa.2018.10.00377
Ultrasound has gained recognition within the field of pain intervention owing to its definite advantage of visually localizing the specified target and additionally owing to perceived advantages of safety, accuracy, and potency. Ultrasound permits satisfactory imaging of the posterior parts of the spine and paraspinal soft tissues. Despite the introduction of newer and less consuming time’s methods with the possibility of intravascular injection, there is still insufficient clinical evidence to prove the safety of the ultrasound as a sole image guide intervention, especially for transforaminal injection. It is essential to considering safety tips and be aware of complications that are typically terribly unpleasant and cause unwanted social and legal consequence. The most important injection warnings are damage to the spinal cord and nerve roots, intravascular injection and vascular damage, loss of consciousness, paraplegia and incontinence. The object of this review article is to discuss the untoward dangerous complication which can happen after ultrasound-guided spine injections and explain how to diagnosis and manage them. Further technical and equipment advancements are needed to improve and reduce the existing limitations associated with the ultrasound-guided spine injection technique until that time the multimodality imaging guidance is safer.
Keywords: spine, injection, ultrasound, pain management
US, ultrasound; FBSS, fail back surgery syndrome; LAST, local anesthetic systemic toxicity; C, cervical; T, thoracic; L, lumbar; S, sacral; CSF, cerebrospinal fluid; DRG, dorsal root ganglion; AP, anteroposterior; ASA, anterior spinal artery syndrome; PDPH, post dural puncture headache; SAP, superior articular process; IVF, intervertebral foramen; ESI, epidural steroid injection
Ultrasound (US) has gained recognition within the field of pain intervention owing to its definite advantage of visually localizing the specified target and additionally owing to perceived advantages of safety, accuracy, and potency. Ultrasound permits satisfactory imaging of the posterior parts of the spine and paraspinal soft tissues. There are many advantages of ultrasound-guided spine intervention and the most important one is lack of radiation exposure (Table 1). Ultrasound is an excellent tool in “visualizing” and hence “avoiding” vascular injury especially during cervical spine procedures.1 Studies on ultrasound-guided spine injection and CT scan confirmation of the needle tip showed feasibility and validity of ultrasound in spine injections.2–6 Despite the introduction of newer and less consuming times methods7 with the possibility of intravascular injection, there is still insufficient clinical evidence to prove the safety of the ultrasound as a sole image guide intervention, especially for transforaminal injection.4,8–10 The ultrasound-guided scanning will not show intravascular injection (the first injection of the test dose just will show no distribution of drug around the goal).
Advantages of ultrasound guided spine injection |
No xrays hazard |
Presentation of vessels and tissues |
Visualize the pleural and lung movements |
Portable ability |
Easily maneuver of ultrasound probe to give different axial and longitudinal view |
Applicable and practical in the outpatient clinical setting |
No limitation in difficult position |
More practical in difficult surface anatomic landmarks |
Get view of anatomical differences |
Increase first pass needle success rate |
Table 1 Advantages of ultrasound guided spine injection
Ultrasound-guided spine injection has limitations and interventionist must be cautious and responsive to these limitations (Table 2). They should consider safety tips and be aware of complications that are typically terribly unpleasant and cause unwanted social and legal consequence. The most important injection warnings are damage to the spinal cord and nerve roots, intravascular injection and vascular damage, loss of consciousness, paraplegia and incontinence.11 The object of this review article is to report possibility of untoward dangerous complication with ultrasound-guided spine injections and provide prompt and timely diagnosis to prevent irreversible damage.
Possible limitations for the ultrasound guided spine injections |
The inability to correctly visualize the target in obese individuals |
The inability to accurately detect intravascular injection in such deep injections |
A longer procedure time for novice |
The potential need for larger gauge needles to improve visualization. |
Image quality in the elderly patient population |
Inaccuracy of skin marking especially in FBSS |
The learning curve for ultrasound imaging of the spine |
The inability to correctly visualize the target in obese individuals and FBSS |
The inability to accurately detect intravascular injection in such deep injections |
A longer procedure time for novice |
The potential need for larger gauge needles to improve visualization. |
Image quality in the elderly patient population |
Inaccuracy of skin marking |
The learning curve for ultrasound imaging of the spine(sacrum) |
Table 2 Possible limitations for the ultrasound guided spine injections
The spinal cord is a long, thin, tubular bundle of nervous tissue and support cells that extends from the medulla oblongata in the brainstem to the lumbar region of the vertebral column. The brain and spinal cord together make up the central nervous system. The spinal cord is the main pathway for information connecting the brain and peripheral nervous system. Spinal injections are delicate and dangerous. Spine injection has many complications (Table 3).12 There are also complications due to the incorrect injection in the non-epidural space which is especially warning after ultrasound-guided spine injection. Knowledge about such complications, time of presentation, signs and symptoms and supporting control is mandatory before starting every spine injection (Table 4).
Complication of spine injection |
Post procedural pain |
Anterior spinal artery syndrome(ASA) |
Embolism lead to paraplegia or quadriplegia, nystagmous, confusion and coma |
Directed injury of the spinal cord |
Dissection of the vertebral artery and breakup of blood brain barrier causes ischemia and brain death followed by high pressure in the cranium |
Neurological complains caused by directing nerve damage |
Transient blindness followed by temporarily increase of intraepidural pressure |
Pneumothorax |
Meningitis ,vertebral osteomyelitis, discitis) |
Bleeding (epidural hematoma) and retroperitoneal hematoma |
Allergic reaction |
Dural puncture and following headaches |
Intravascular injection (in the sacral zone there is a high possibility of intravascular injection because of high vascularity |
Arachnoiditis |
Consequent of steroid injection , like suppression of cortisone level for up to 2 weeks and increase in blood glucose level |
Vasovagal reaction |
Ataxia especially for cervical block |
Epidural lipomatosis |
Cauda equina syndrome |
Table 3 Spine injection complication
Meningeal space |
Clinical presentation |
The onset |
Sign & Symptom |
Subdural space
Subarachnoid
Local anesthetic toxicity via systemic absorption or accidental
Spinal cord or Root injury
Intravascular injection |
Subdural block
Spinal block Post dural puncture headache PDPH
Total spinal block(although it is more possible after epidural injection)
|
Gradual/delayed onset (1030 or 1520 minutes)
Minutes Typically occurs hours to days
The onset is fast approximately minutes after the injection however, delay up to 30 minute IV injection results in rapid onset and
Immediately and delay onset (hours)
Minutes ,days |
Extensive sensory block with minimal motor block, hypotension (more than with epidural, less than with spinal)and in worst case scenario, intracranial tracking leads to dyspnea and loss of consciousness Deep and prolong motor and sensory block Headache is severe and described as "searing and spreading like hot metal," involving the back and front of the head, and spreading to the neck and shoulders, sometimes involving neck stiffness. It is exacerbated by movement, and sitting or standing, and relieved to some degree by lying down. Nausea, vomiting, pain in arms and legs, hearing loss, tinnitus, vertigo, dizziness and paraesthesia of the scalp are common Complete bilateral sympathetic, sensory and motor blockade below a certain level. The patient suddenly became apneic, unresponsive, and totally flaccid, with bilateral dilated nonreactive pupils,hypotension and bradycardia Classically, systemic toxicity begins with symptoms of CNS excitement such as the following: circumoral and/or tongue numbness ,metallic taste ,lightheadedness ,dizziness ,visual and auditory disturbances (difficulty focusing and tinnitus) disorientation ,drowsiness ,With higher doses, initial CNS excitation is often followed by a rapid CNS depression, with the following features: muscle twitching ,convulsions ,unconsciousness ,coma ,respiratory depression and arrest, cardiovascular depression and collapse Neurogenic shock with severe pain ,bradycardia and hypotension Spinal cord infarction,cell necrosis and ischemia and serious functional deficit and clinically presented as ASA syndrome. ASA syndrome characterizes by a sudden bilateral loss of pain and temperature below the spinal lesion level, with the preservation of vibration and position sensation, loss of motor function (usually paraplegia) and absence of urine and stool control |
Table 4 Misleading spine injection and its consequences
Subdural block
The spinal cord protected by layers of tissue or membranes referred to meningeal membranes. There are also some spaces between these layers; epidural space which is outer layers between flavum ligament and dura mater, subdural space that is a virtual space between dura and arachnoids (it is more prominent in FBSS) and subarachnoid space which includes CSF. Spine intervention therapeutically performs in the epidural space (e.g. radiculopathy) and injection in other spaces (subdural, arachnoid) lead to injection complication.Ultrasound is a valuable modality for close monitoring of these spaces to inject directly into epidural space and prevent unwanted injection to other layers or injury to the spinal cord and nerve root although itis not enough (Figure 1).
Subdural space is a potential space between arachnoids and dura, which contains serous fluid. This spreads across the cranial cavity throughout the distribution of meanings, covering all nerve structures. Space ends in the lower boundary region of the S2, where the film terminal ends. It is the widest in the cervical area and is narrow in the lumbar region and is expanded over dorsal root ganglion (DRG). The dorsum and lateral subdural space have a higher potential capacity. Both dura and arachnoids are connected together in the ventral root and thus the potential subdural space is much smaller ventrally. Subdural injection located in the posterior part and spare the anterior nerve roots which carries sympathetic and motor .The incidence of subdural injectionduring epidural injection of the lumbar spine is 0.8 %. The subdural space in the cervical region is larger than the lumbar region, so the risk of unintended subdural injection may also be higher in the cervical area.13,14 The onset of the block is intermediate betweensubarachnoid and epidural block and distinguish by a fastunexpectedly high sensory block . Clinical diagnosisof subdural injection is a moderate decrease in blood pressure, slow onset of symptoms, progressive respiratory problem, and complete recovery in two hours’ time followed by a full recovery.15–17 Accidental injection into the subduralspaces ought to be suspected if there's less pronounced resistance once the needle is placed within the epidural space or if the patient complains of a frontal headache.The tiny volume of sunduralspace might permit local anesthethic to succeed in intracranial structures (e.g. brainstem) resulting in important neurologic and hemodynamic complications with a period of unconscious state and apnea lasting many hours. Patients with previous back surgery were a lot of probably to possess the subdural injection, because of secondary anatomy that was liable to scarring and potential loss of epidural space. A recent spinal block may also be a predisposingfactor to subdural injection. Patients with a subdural block should closely monitor for vital supportand assurethat this is often a reversible and temporary event.18–22
Flouroscopicview of contrast injection in meningeal spacs
Fluoroscopy helps you to differentiated epidural block from the subduralor subarachnoid injection. The AP fluoroscopy of subdural injection shows a dense contrast in the center of the vertebral canal with a small amount of contrast extend laterally, delineating the nerve roots that are not affected by a change in posture and can be unilateral. The AP fluoroscopy of the epidural injection demonstrates afoamy pattern which is due to the fatty content of epidural space with a flow outward through the IVFand along nerve roots.The AP fluoroscopy view of subdural injection is similar to the subarachnoid injection, but the contrast agent rapidly descends in the CSF with gravity and dilute, so appear less opaque although outlines the exiting nerve roots in AP view. The lateral fluoroscopy view of subdural injection represents a dense collection confined to the posterior aspect of the spinal canal, spreading mainly in a cephalic direction. Due to the small volume of the subdural space relative to the epidural space, the cephalocaudal spreading of the contrast agent is far more compared to the epidural space even with low volume contrast injection. While the posterior line of the subdural injection is soft due to the dura, the anterior boundary appears irregular due to the arachnoids andthere are a regular posterior border and an irregular anterior border of condensed contrast. Comparingto the typical lateral lumbar epidurogram demonstrates the “double-line” or “railroad track” appearance of radiographic contrast in the anterior and posterior epidural space in epidural block, the subdural block looks like a "railroad track", however, contrast did not fill along the exiting nerve root in AP view unlike an epidural "railroad track"23–25 (Figures 2-4) (Table 5).
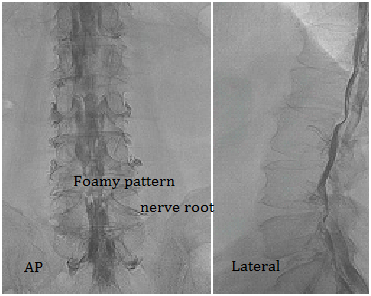
Figure 2 AP fluoroscopy of epidural block and distribution of contrast with foamy pattern that flow outward through the intervertebral foramina along nerve roots, lateral view of epidural block and double-line” or “railroad track”.
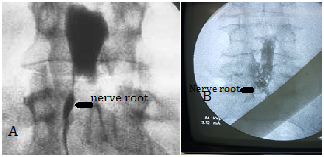
Figure 3 The AP fluoroscopy view of subdural injection(A) shows a dense contrast in the center of the vertebral canal compare to the foamy pattern of fatty content of epidural space(B) and a wide distribution which tends to flow outward through the intervertebral foramina along nerve roots however in subdural injection a small amount of contrast may extend laterally, delineating the nerve roots, spread can be unilateral.
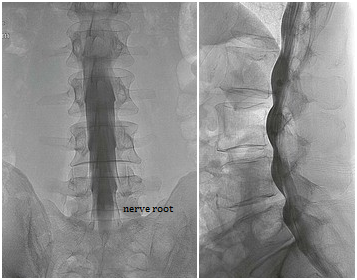
Figure 4 AP & lateral fluoroscopy of subarachnoid block .The spinal cord and exiting nerve roots are visible within the contrast collection, the contrast extends all the way from the posterior to the anterior limits of the thecal space in lateral view.
Anatomic space |
Lateral view |
AP view |
Epidural |
“Doubleline” or “railroad track” appearance of radiographic contrast in the anterior and posterior epidural space |
Foamy pattern of fatty content of epidural space and a wide distribution which tends to flow outward through the intervertebral foramina along nerve roots |
Subdural |
The regular posterior border and irregular anterior border of loculated contrast |
A dense contrast in the center of the vertebral canal |
Subarachnoid |
The contrast extends all the way from the posterior to the anterior limits of the thecal space |
CSF dilutes contrast and it appears less opaque, the spinal cord and exiting nerve roots are visible within the contrast collection |
Table 5 Comparing AP & Lateral fluoroscopic view of epidural & subdural and subarachnoid space after contrast injection
Complete or total spinal block
Total spinal block is a high block involving the cervical spine and above (such as brain stem and cranial nerves). It is more frequent with epidural block to spinal block and depend on anatomic variation.26 Symptoms and signs (hypotension, bradycardia, nausea and anxiety, arm/hand dysaesthesia or paralysis respiratory compromise, apnea, reduced oxygen saturation, difficulty speaking/coughing, loss of consciousness, cardiac arrest ) usually occur within minutes, however, delay up to 30minutes has been reported. Nausea and high sensory level block (>T1) may be early indicators. Management is supportive and dependent on degree and height of the block. Early recognition is vital to prevent serious cardio respiratory compromise.21
Local anesthetic systemic toxicity (LAST)
Local anesthetic reaches the circulation via systemic absorption or accidental intravascular injection. The incidence of LAST for epidural anesthesia is 1.2–11 per 10 000 anesthetics. It is more frequent with the epidural block to spinal block. After LA administration, any abnormal cardiovascular or neurological symptoms and signs, including isolated cardiac arrest (cardiovascular collapse may occur without preceding neurological changes) should raise suspicion of LAST. Central nervous system toxicity is classically described as a two-stage process. An initial excitatory state is followed by a depressive phase. Early neurological features include perioral tingling, tinnitus, and slurred speech. Lightheadedness and tremor may also occur, as may a change in mental status with confusion or agitation. However, LAST can occur without characteristic premonitory signs. The excitatory neurological phase culminates in generalized convulsions. This may lead to the depressive phase of coma and respiratory depression. Cardiovascular system toxicity is classically in three phases. The initial phase includes hypertension and tachycardia. The intermediate phase is associated with myocardial depression and hypotension. The terminal phase includes peripheral vasodilatation, severe hypotension, and a variety of arrhythmias such as sinus bradycardia, conduction blocks, ventricular tachyarrhythmia, and asystole.27
While prevention is clearly the most important element in avoiding morbidity and mortality associated with LAST, such cases still occur despite best practice. The block should take place in a setting with standards monitoring, resuscitation equipment, and capable help nearby knowing how to manage this uncommon event. The key is to recognize it immediately and institute appropriate management and follow up.28 Keep in mind ultrasound guidance injection reduces the risk of local anesthetic systemic toxicity.29
Spinal cord & nerve root injury
Intraneural injection, a direct trauma to the nerve root or dorsal root ganglion can occur by inadvertent needle placement, especially during transforaminal ESI. Transoraminal injection performs in three ways. In classic or sub-pedicle technique needle enter below the pedicle and above the superior articular process (SAP). Concentration of the contrast medium is located along the nerve and the posterior and anterior epidural space. The other method is retroneural injection more posterior than the subpedicular technique and lateral to nerve root, so the contrast agent spreads along the nerve and posterior epidural space. In the last technique or retrodiscal method, needle enter from the outside of the SAP of the lower vertebra to the medial aspect of nerve and anterior epidural space. Retroneural approach may help to avoid such nerve trauma.30–32 (Figure 5) In cases of intraepineural injection, the patients may have severe radiating pain during the procedure, and it may cause mechanical neuritis or nerve injury inside the nerve root. When a patient presents severe pain during the procedure or distinct type of contrast spread pattern is identified, the needle should be slightly withdrawn and reassessment of the needle position is recommended. Do not over sedate patient before the procedure for not masking patient reaction. Sign and symptoms of spinal cord injury are more severe: neurogenic shock with severe pain, bradycardia, and hypotension with delay onset (hours) of complete sensory and motor loss, paraplegia, complete loss of bowel and bladder sensation.
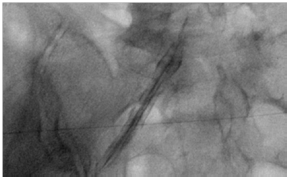
Figure 5 Intraepineural contrast spread, the nerve root has several thin linear contrast fillings inside the nerve root as a feathery appearance.
Inadvertent intravascular injection or injury
The posterior and anterior radicular arteries majorly supply spinal cord below the neck. These arteries run into the spinal cord alongside the dorsal and ventral nerve roots. The Adamkiewicz artery is the largest anterior radicular arteries, which usually arises between L1 and L2 or anywhere from T9 to L5. Although doppler ultrasound is useful for scanning of a blood vessel, because of the risk of intra-arterial injection, insoluble corticosteroids must not be used when real-time contrast dye injection with fluoroscopy and/ or digital subtraction angiography is not used. The mechanism of injury may be related to vascular injury, not steroid embolism. Vascular injury may be to direct trauma with or without injection. Since the Adamkiewicz artery is the only artery that gives a lot of blood flow to the spinal cord of the lumbosacral region, it is clinically important. Unfortunately and rarely the radiculomedulary blood flow during the pain injections is cut off. Any disruption of the spinal cord blood flow is clinically important due to the cell necrosis, ischemia and serious functional deficit which clinically presented as ASA syndrome.
ASA syndrome characterizes by a sudden bilateral loss of pain and temperature below the spinal lesion level, with the preservation of vibration and position sensation, loss of motor function (usually paraplegia) and absence of urine and stool control. Even though the radicular artery is visible by ultrasound, it is advisable to inject contrast agent at the end of the procedure and take a contrast injection fluoroscopy view to rollout intravascular injection. Intravenous contrast injection is typically not seen on still images because the contrast material is rapidly diluted in the bloodstream. During real-time or live fluoroscopy, intravenous contrast can be seen flowing away and lateral from the spinal canal toward the venous circulation. Intra-arterial contrast injection is typically not seen on still images because the contrast material is rapidly diluted in the bloodstream. During real-time or live fluoroscopy, intra-arterial contrast injection can be seen flowing toward the midline (e.g. lumbar spinal cord)33,34 (Figure 6) (Figure 7).
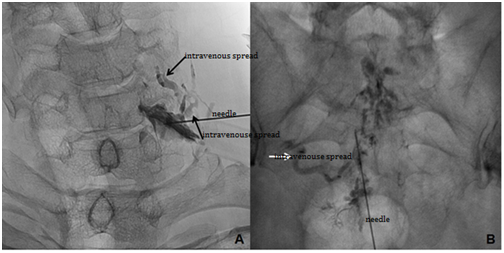
Figure 6 Inadvertent intravenous contrast can be seen flowing away and lateral from the spinal canal toward the venous circulation during cervical transforaminal block(A)& caudal block(B).
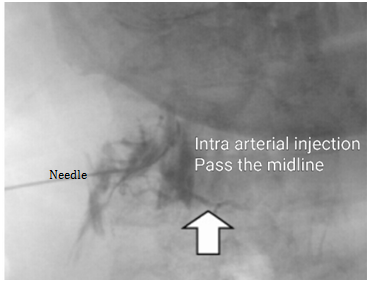
Figure 7 intra-arterial injection disappear soon and contrast injection can be seen flowing toward the midline during cervical transforaminal block.
Transforaminal ESI injection has more chance of intravascular injection. As mention before transforaminal epidural injection perform with different techniques: classic sub-pedicular approaches through the safe triangle zone, retroneural technique (periradicular or selective nerve root block) to the posterior neural foramen and retrodiscal technique (kambin triangle) into the neural foramen and medial aspect of the spinal nerve (retrodiscal area).32 The safe triangle zone is not really safe. Retroneural approach may help to avoid intravascular injection. It is safer to place needle lateral the exiting nerve root and farther from IVF and epidural space to obviate the risk of placing the needle in the area of foramen that contains the blood supply to the spinal cord. There is no significant correlation between pain relief and needle tip position retroneural or subpedicular approach in relation to the neural foramen and success rate is not dependent on the distance between the needle tip and the nerve root.33–39 The predisposing factor for intravascular injection are the size, sharpness, positioning of the needle within the foramen, rate of injection, and vascular engorgement.40 The ability of the ultrasound to show vessels and increase first pass needle success rate reduces this complication.
The question is that how to perform a safe injection nevertheless such side effect and complications. Although ultrasound guidance regional anesthesia is a gold standard technique41 but ultrasound guide spine injection is a little different .It is not easy and has limitations as a result of depth, bony acoustic shadowing, and complicated three- dimensional anatomy. Preliminary studies suggest that having acquired the basic knowledge on ultrasound of the lumbar spine, the experience of 40 or more cases may be required to attain competency in just spine scanning.42 Safety tips should be considered before every ultrasound guide spine injection. These include: patient selection, sterilization, monitoring of the vital signs, preparation of the emergency rescue equipment, and limitation of drug dosage to the comprehensive familiarity with the ultrasound device, settings, and secondary confirmation technique (Table 6).43,44Real-time fluoroscopy at the end of every spine procedures can show the intravascular pattern of injection or inadvertent space clearly. Interventional pain physicians must have an adequate knowledge of normal and abnormal patterns of epidural and perinural fluoroscopy guided contrast dispersion and flow in order to avoid harm to the patients. This complication probably occurs more often than is recognized and may lead not only to a lack of efficacy but also to a potential hazard. Further technical and equipment advancements are needed to improve and reduce the existing limitations associated with the ultrasound-guided spine injection technique until that time the multimodality imaging guidance is safer.
Safety recommendation for spinal injections |
Choice of the patient carefully for the specific processor |
Obtain and view MRI scans prior to performing the procedure. Disc herniation may shift the |
Know the contraindication of spine injection, such as patient dissatisfaction and uncontrolled coagulation disorder |
Be aware of patient medical history(e.g. diabetes, hypertension and cardiovascular disease) |
Consider the possibility of increasing blood glucose after steroid injection in diabetics |
Discontinue medications that increase the likelihood of bleeding, according to the protocol before and after |
Use sedation as needed, minimize it in the cervical injections |
Completely adhere to the sterilization |
Monitor the vital signs |
Prepare emergency rescue equipment for emergency situations |
The correct counting of the vertebrae that you can use for signs of the occipital promontory, |
Comprehensive familiarity with ultrasound device and settings. Consider the types of probes |
Avoid deep sedation. The deeply sedated patient may become agitated and may move unexpectedly. |
Use local anesthetic before needling |
Speak with your patient during procedure to aware of the patient vigilance and show the |
Perform a systematic scan |
Visualize key landmark structures |
Identify target on shortaxis imaging(preferred) or long axis |
Plan for safe needle approach as far as possible from vital organs and vascular |
Follow the tip of the needle in real time |
Inject small amount of a test dose before drug injection |
Monitor spreading of injection under real time |
Remember there is increase chance of neurologic injury with transforaminal epidural |
Consider the use of nonparticulate steroids. |
There is an increased chance of neurologic injury when particulate steroids are used for |
Limit the total local anesthetic to an amount that is safe if delivered intrathecally. Provide |
Rule out intrathecal needle placement with a local anesthetic test dose. Abandon the procedure |
Avoid the addition of epidural opioids, especially morphine |
Because of the risk of intra arterial injection, insoluble corticosteroids must not be used |
Avoid epidural needle placement above C67. There is typically a small amount of epidural fat |
Ultrasound allows direct visualization of soft tissue structures and may play an important role in |
Consider a secondary confirmation technique (e.g. fluoroscopy after contrast injection) |
Maintain appropriate document |
Table 6 Safety recommendation for spinal injections
None.
The author declares no conflict of interest.

©2018 Gharries. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.