Journal of
eISSN: 2373-6437


Research Article Volume 5 Issue 4
3rd Anesthesiology Department, Hippokratio General Hospital, Thessaloniki, Greece
Correspondence: Dimosthenis Petsas MD, Karavaggeli 49, Pilaia, Thessaloniki, PO BOX 55535, Greece, Tel 00306972008383
Received: August 11, 2016 | Published: August 23, 2016
Citation: Petsas D, Leontidou A (2016) Epidemiology and Characteristics of Emergency Pediatric Neurosurgical Cases in A Tertiary Hospital in Northern Greece. J Anesth Crit Care Open Access 5(4): 00195. DOI: 10.15406/jaccoa.2016.05.00195
Purpose: Description of the emergency pediatric neurosurgical cases in a tertiary hospital in northern Greece. We examined age, sex, initial diagnosis, comorbidities, surgery duration, need for revision surgery and complications. We also investigated possible correlations between age, surgery duration, preexisting medical conditions as well as kind and frequency of complications.
Patients and Methods: This was a retrospective study (from January 2008 to September 2011), by the Anesthesiology department .The study was based on the anesthesia intraoperative and postoperative records. All statistical distributions and analysis was made using SPSS® (Version 20.0. Armonk, NY: IBM Corp.©).
Results: We examined 116 emergency operations (in 55 patients). Patients age varied from 0 to 16 years old (majority aged 0- 6 months old). The 63.79% were males and 36.21 % females. The most frequent diagnosis was hydrocephalus of various haetiology (56 %), traumatic brain injury (12, 9%), craniosynosteosis (12, 1%), tumors (8, 6%). A percentage of 70.7% had one or more preoperative comorbidities. Preoperative comorbidities included prematurity, anemia, infectious disease and respiratory problems.
Conclusion: A medium-high rate of complication (25%) and increased revision surgery rate. Testing for possible correlations explaining that fact showed no significant correlation between surgery duration, number of revision and complications. There seems to be possible correlation between preexisting comorbidity and possibility for revision operation. Female sex and revision surgery seems to predispose to increased risk of complications.
Keywords: pediatric neurosurgery, diagnoses, comorbidities, complications, Greece
It is well known, throughout history of medicine that epidemiologic observations and reports has many times highlighted possible correlations of various medical conditions with several factors. Epidemiology is the study of how often diseases occur in different groups of people and why. Epidemiological information is used to plan and evaluate strategies to prevent illness and as a guide to the management of patients in whom disease has already developed.1,2 This fact highlights the value of reporting cumulative data from epidemiological observational (cohort) studies. By analyzing data collected from this type of studies, the investigators can form an hypothesis which of course may need other type of studies to confirm. Pediatric neurosurgery presents with many peculiarities .The unique anatomy and physiology of children, the evolving nervous system and the need to live and evolve for many years with the medical intervention and its consequences.3,4
One of our special interests in this retrospective study was to investigate the distribution of age, preoperative comorbidities, duration of surgery and the need for revision surgery, as well as reporting some adverse outcomes and complications in this specific subtotal of pediatric patients in northern Greece. Studying emergency cases give us the advantage of observing patients with important comorbidities undergoing neurosurgical intervention. In opposition, elective surgery imposes postponing the surgery and managing (if possible) preexisting comorbidities.
Our study was a retrospective observational (cohort) study of all emergency pediatric neurosurgical cases in a tertiary hospital in northern Greece. We examined a total of 116 operations in 55 patients from January 2008 to September 2011. There was recording of sex, age, initial (preoperative) diagnosis, preexisting comorbidities, type of surgery, surgery duration, number of revisions in each patient and postoperative complications.
All patients received general anesthesia and were intubated. Induction of anesthesia included intravenous (IV) administration of thiopental, induction dose 4-5 mg/kg of body weight (BW), fentanyl 1mcg/kg BW and a muscle relaxant (rocuronium 0.8mg/kg BW). Anesthesia maintenance included combination of a volatile anesthetic (Sevoflurane) with maximum allowed concentration from 0.8 to 1 Minimum Alveolar Concentration-MAC (with goal to minimize alterations in cerebrovascular autoregulation),5 combined with remifentanyl at an infusion rate of 0.5 mcg/kg/min, titrated up to 1 mcg/kg/min depending on hemodynamic response to noxious stimuli. Calculation of intravenously administered fluids was based on the "4:2:1" rule (4 ml/kg/h for the first 10 kg of body weight plus 2 ml kg/h for the next 10 kg of body weight and addition of 1 ml/kg/h for every kilogram of body weight above this).6
Concerning the type of IV fluid solution to be administered, Dextrose 5% with Normal saline (D5NS) was administered to children up to 12 months of age while older children received Ringers Lactate. The decision of administering a solution containing dextrose in neurosurgical patients under 12 months of age (despite reports of possible negative influence on nervous system) was based on estimation of patients being prone to develop hypoglycemia.6,7 All recorded parameter distributions were tested for normality (using Kolmogorov -Smirnov, Shapiro-Wilk and D'Agostino skewness, kurtosis and omnibus).
When normality in distribution was rejected, a non parametric test were used for comparisons (Mann-Whitney test). In the case of non existing normality, all distributions were described reporting median and range instead of mean and standard deviation.8 Nominal data were tested with the use of contingency tables (2x2), Phi "Φ" criterion and Chi Square transformation, as well as significance level.
All data were analyzed using SPSS ® (Version 20.0. Armonk, NY: IBM Corp.©), and StatPlus® Proffesional( Version 5.8.4.3, ©2010 Analystsoft). A review of our study material, operations and complications can be seen in Table 1.
|
Review of study data |
|||
|
Median (range) |
Mean (SD) |
||
|
Age (mo) |
12 (2-192) |
44.4 (53.2) |
|
|
Sex |
|||
|
Male, n (%) |
74 (63.8) |
||
|
Female, n (%) |
42 (36.2) |
||
|
Preexisting comorbidity, n (%) |
82 (70.7) |
||
|
Initial Diagnosis |
|||
|
Hydrocephalus, n (%) |
65 (56) |
||
|
Craniosynostosis, n (%) |
14 (12.1) |
||
|
TBI, n (%) |
15 (12.9) |
||
|
Tumors, n (%) |
10(8.6) |
||
|
Other, n (%) |
12 (10.3) |
||
|
Operation |
|||
|
External drainage, n (%) |
34 (29.3) |
||
|
Ventriculoperitoneal drainage, n (%) |
26 (22.4) |
||
|
Calvarial vault remodeling, n (%) |
14 (12.1) |
||
|
Craniotomy-tu excision, n (%) |
10 (8.6) |
||
|
All Operations, N (%) |
116 (100) |
||
|
Initial operations, n (%) |
55 (47.4) |
||
|
Revision, n (%) |
61 (52.6) |
||
|
No. of revisions, n (%) |
0(0-13) |
1.3(2.4) |
|
|
Complications |
|||
|
All, n (%) |
29(25) |
||
|
Infectious, n (%) |
16 (55.2) |
||
|
Electrolytes imbalance, n (%) |
6(20.7) |
||
|
Cerebral hemorhage, n (%) |
3 (10.3) |
||
|
Fever of unknown origin, n (%) |
2 (6.9) |
||
|
Pneumencephalus, n (%) |
2 (6.9) |
||
Table 1 Review of epidemiologic data and operational characteristics of the study population
SD, standard deviation; Mo, months; TBI, traumatic brain injury; Tu, tumors
Concerning patients sex there was a vast predominance of male gender, including 74 males and 42 females (63.79% vs 36.21 %), in a total of 116 surgery cases. The age - frequency distribution of pediatric neurosurgical patients expressed in months of age can be seen in Figure 1. The primary (preoperative) diagnosis of the emergency pediatric neurosurgical patients included a variety of conditions, with hydrocrephalus being the most frequent preoperative diagnosis. The preoperative diagnoses frequencies can be seen as a pie graphic in Figure 2. The surgery duration (primary and revisions) was 120 minutes (range 50-630 minutes). The duration is expressed as median (range). Twenty one (21) of the 55 pediatric patients finally underwent one or more revision surgery (38%). These patients underwent from 1 to 13 (!) revision operations. The number of patients related to the number of revision operations can be seen in Figure 3.
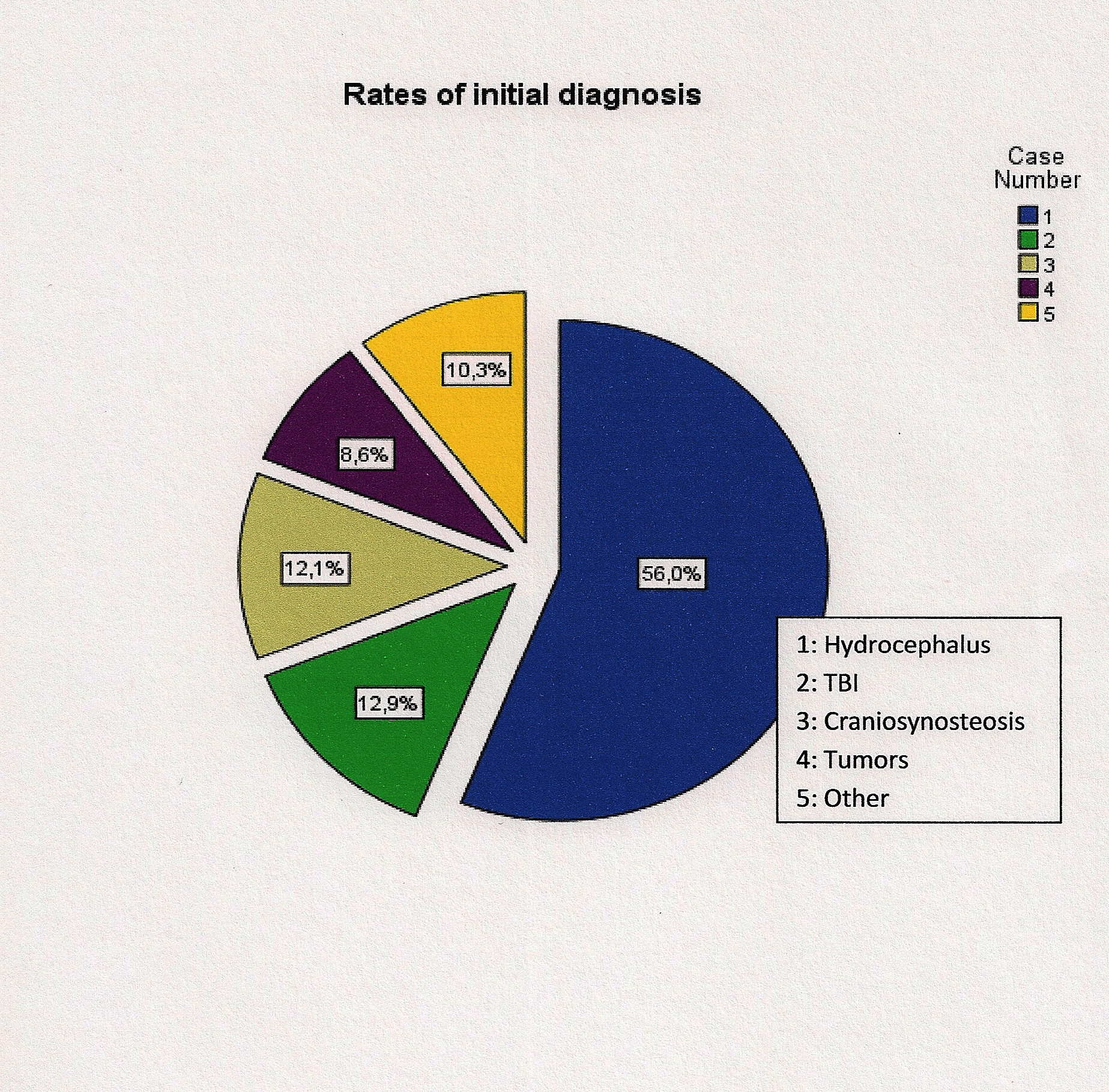
Figure 2 Distribution of primary (preoperative) diagnoses of pediatric emergency neurosurgical patients. (1: Hydrocephalus, 2: Traumatic Brain Injury, 3: Craniosynostosis, 4: Tumors, 5: Other).
As it can be clearly seen in Figure 3, the majority of pediatric patients underwent one or two revision operations. There were a total of 61 revision surgeries. From this total of 61 operations, 17 (27.9%) was external drainage revision, 12 (19.7 %) was ventriculoperitoneal drainage revision, 2 (3.3%) conversion from external drainage to ventriculoperitoneal drainage, 5 (8.2%) conversion from ventriculoperitoneal to external drainage, 2 (3.3%) craniotomies, 4 (6.6%) cases of calvarial vault remodeling and other procedures in 19 cases (31.1%). The characteristics of these revision operations concerning type of operation, age of patients, preexisting comorbidities and complications can be seen in Table 2.
|
Type of revision operations and patients characteristics |
||||
|
Parameters |
||||
|
Revision operation |
No. of patients n (%) |
Age (mo) Median(range) |
Pre existing comorbidity n (%) |
Complication n (%) |
|
External drainage |
17(27.9) |
7 (2-72) |
12(70.6) |
6(3.5) |
|
Venticuloperitoneal |
12(19.7) |
33.5 (3-144) |
12(100) |
3(25) |
|
External to ventriculoperitoneal |
2(3.3) |
75.5(7-144) |
1(50) |
0(0) |
|
Ventriculoperitoneal to external |
5(8.2) |
60(18-72) |
2(40) |
1(20) |
|
Craniotomy |
2(3.3) |
94.5(9-180) |
1(50) |
1(50) |
|
Calvarial vault remodeling |
4(6.6) |
9.5(8-18) |
2(50) |
1(25) |
|
Surgical cleaning |
5(8.2) |
36(8-144) |
3(60) |
1(20) |
|
Central vain placement |
1(1.6) |
3 |
1(100) |
0(0) |
|
Other |
13(21.2) |
- |
- |
- |
Table 2 A review of revision operations concerning type of operation and patients characteristics in each operation. Since parameters distribution did not met normality criteria, they are expressed as median (range)
Mo, months.
Preexisting (preoperative) comorbidities of the study patients was prematurity, respiratory distress syndrome, infectious disease ( tuberculose meningitis, upper and lower respiratory tract infections, HCV), anemia, thalassemia, congenital heart disease, respiratory and renal disease. The frequency of these preexisting comorbidities distributed in relation with patients age is shown in Table 3.
|
Distribution of preexisting (preoperative) comorbidities related to patients age |
|||||||
|
Age |
|||||||
|
0-6 mo n (%) |
7-12 mo n (%) |
1-5 y n (%) |
6-10 y n (%) |
11-15 y n (%) |
>15 y n (%) |
||
|
Prematurity |
15 (12.9) |
9 (7.7) |
4 (3.4) |
3 (2.6) |
- |
- |
|
|
Anemia |
14 (12.1) |
4 (3.4) |
2 (1.7) |
1 (0.9) |
- |
- |
|
|
Respiratory |
RDS |
12 (10.3) |
7 (6.0) |
2 (1.7) |
- |
- |
- |
|
URI/LRI |
- |
2 (1.7) |
1 (0.9) |
1 (0.9) |
5 (4.3) |
- |
|
|
other |
2 (1.7) |
1(0.9) |
- |
1 (0.9) |
3 (2.6) |
- |
|
|
CHD |
4 (3.4) |
- |
1 (0.9) |
- |
- |
- |
|
|
Oncological |
2 (1.7) |
- |
- |
1 (0.9) |
- |
- |
|
|
Other |
4 (3.4) |
1 (0.9) |
- |
2 (1.7) |
1 (0.9) |
- |
|
|
Total |
|
53(45.7) |
24(20.7) |
10(8.6) |
9(7.7) |
9(7.7) |
- |
Table 3 Distribution of preexisting comorbidities in relation with patients age
Mo, months; y, years; RDS, respiratory distress syndrome; URI, upper respiratory tract infection; LRI, lower respiratory tract infection; CHD, congenital heart disease
Clinically important complications during these operations were observed in 29 cases in a total of 116 operations (overall frequency of complications 25%). In this subtotal of complications, the diagnoses and relative frequencies were: cerebral hemorrhage in 3 of 29 cases (10.3%), infective complications in 16 of 29 cases (55.2%), electrolytes abnormalities in 6 of 29 cases (20.7%), fever of uncertain origin in 2 of 29 cases (6.9%), pneumencephalus in 2 of 29 cases (6.9%). If the number of complication mentioned above is attributed to the whole sample of our study (a total of 116 operations) then the percentages transforms as following: infective complications 13.8%, electrolytes abnormalities 5.2%, cerebral hemorrage 2.6%, fever of central origin 1.7% and pneumencephalus 1.7%. These complications, related to patient’s age can be seen in Table 4.
|
Distribution of complications related to patient's age |
||||||
|
Age |
||||||
|
0 - 6 mo n (%) |
7- 12 mo n (%) |
1 - 5 y n (%) |
6 - 10 y n (%) |
11-15 y n (%) |
>15 y n (%) |
|
|
Infection |
4(13.8) |
2(6.9) |
7(24.1) |
2(6.9) |
1(3.4) |
- |
|
Hemorrhage |
2(6.9) |
- |
1(3.4) |
- |
- |
- |
|
Electrolyte abnormalities |
1(3.4) |
4(13.8) |
- |
- |
1(3.4) |
|
|
Fever |
1 (3.4) |
1(3.4) |
- |
- |
- |
- |
|
Pneumencephalus |
- |
- |
1(3.4) |
1(3.4) |
- |
- |
|
All, N=29 (25%) |
8(27.6) |
7(24.1) |
9(31.0) |
3(10.3) |
2(6.9) |
0(0) |
Table 4 Complications frequency distributed in relation with patients age
Mo, months; y, years
As it can be seen in the above table, complications are more frequent in ages from 1-5years old followed by the group 0-6 months. The most frequent and clinically important infective complications included, six (6) cases of meningitis (two cases of tuberculose meningitis, one case of vancomycin resistant enterococcus meningitis), one (1) case of central nervous system (CNS) infection, two cases of possible colonization of the cerebrospinal fluid (one case with Aspergillus and one case with Gram positive cocci), two (2) cases with fever of uncertain origin, two (2) cases of lower respiratory tract infection and one (1) case of upper respiratory tract infection. It might be logical to assume that some of these infective complications were the result of treatment in the pediatric intensive care unit. Although the above mentioned may be supported, it is also difficult detecting the impact of surgical stress response and effect of anesthetics in immune function as well as preexisting comorbidities.9–11
Testing for possible increased complications in pediatric patients with preexisting comorbidities shows an increased rate of complications in pediatric patients with preexisting comorbidities. Of a total 25% rate of overall complications, 69% presented in patients with at least one comorbidity and 31% in patients with no preexisting comorbidity. We applied the "Φ" (Phi) criterion for comparison of nominal data (comorbidity, no comorbidity, complication, no complication) and then transforming to Chi -Square (χ2). Testing for significance can be seen in Table 5.
|
Contingency tables results |
|||||
|
Phi "Φ" criterion and Chi-Square transformation - statistical significance. |
|||||
|
Chi Square (χ2) |
Sig. (p) |
||||
|
Parameters |
Phi (Φ) |
Yates |
Pearson |
Yates |
Pearson |
|
Patient's sex/revision surgery |
-0.12 |
1.1 |
1.59 |
0.294 |
0.207 |
|
Patient's sex/complications |
-0.14 |
1.59 |
2.18 |
0.207 |
0.139 |
|
Surgery duration/complications |
0.12 |
1.16 |
1.67 |
0.281 |
0.196 |
|
Revisions/complications |
0.16 |
2.15 |
2.89 |
0.142 |
0.089 |
|
Preexisting comorbidity/revisions |
0.35 |
12.67 |
14.26 |
0.0003 |
0.0001 |
|
Preexisting comorbidity/complications |
0.05 |
0.11 |
0.31 |
0.74 |
0.577 |
Table 5 Results of 2x2 contingency tables. "Phi" criterion and Chi-square (χ2) transformation
Statistical significance under p=0.05
Important indications is extracted with the calculation of odds ratio between sex (male/female), surgery duration (with remodeling into two groups: one group under 120 minutes and the other over 120 minutes), type of surgery (primary/revision), preexisting comorbidity and complications. The results can be seen in Table 6. From the odds ratio table we can see that sex and type of surgery (primary or revision) may be associated with increased rate of complication. To be more specific, female sex and revision surgery seems to predispose to an increased possibility of occuring complications.
|
Odds ratio and significance of various factors with postoperative complications |
|
||||
|
Groups |
Odds ratio |
95% Confidence Intervals |
z |
Sig.(p) |
|
|
Lower limit |
Upper limit |
||||
|
Sex/complications |
2.231 |
0.969 |
5.132 |
1.88 |
0.059 |
|
Duration/complications |
0.839 |
0.363 |
1.938 |
0.41 |
0.682 |
|
Type of surgery/complications |
4.448 |
1.729 |
11.442 |
3.09 |
0.002 |
|
Comorbidity/complication |
0.928 |
0.376 |
2.228 |
0.16 |
0.871 |
Table 6 For purposes of calculating odds ratio, surgery duration was grouped in two groups, one group with surgery duration < 120 minutes, and one group in which duration was >120 minutes. Grouping of surgery type refers to initial or revision surgery
It is an established knowledge that preexisting comorbidities preoperatively may influence the outcome of surgical procedures concerning the frequency of occuring complications.12 The majority of these comorbidities is usually expressed cumulative in the form of a clinical/functional scale, such as ASA (American Society of Anesthesiologists) classification, or additionally taking into account laboratory values, as in the APACHE (Acute Physiology And Chronic Health Evaluation) score and other scales. These scales have a value that is priceless, but in this type of research deprives us of the capability to detect the role of a specific preexisting comorbidity that may lead to increased complications. This was the reason we recorded specific comorbidities and did not "code" preoperative status and comorbidity applying one of these scales. Many preoperative conditions aggravating the overall morbidity and mortality has been encountered in this study. Conditions as brain cancer, leukemia, head injury, respiratory failure, pyrexia, hydrocephalus and pneumonia which were present in our study population has been shown to be factors aggravating the prognosis (morbidity and mortality), with specific odds ratio for each factor.13,14 We believe that the best way to prove and establish a correlation between preoperative comorbidities and postoperative complications is to study cases of emergency surgery. In elective surgery, postponing the operation and treating (if possible) the comorbidity, is the indicated approach. The opposite is increasing the perioperative risk and may be medically "unethical". Furthermore, for pediatric patients it is a major mistake to generalize knowledge exported from studies including adults. Major differences concerning anatomy, physiology and specific comorbidities may alter their management. Especially in neurosurgery and neuroanesthesia, there are major differences concerning the maturity of central nervous system (CNS), such as blood brain barrier immaturity, craniac vault differences, airway anatomy differences, cardiac autonomic reflexes alterations and differences concerning pharmacodynamics and pharmacokinetics.15
The main purpose and goal of our retrospective study was to describe and highlight possible correlations between basic parameters of factors affecting outcome, such as age, sex, surgery duration preexisting comorbidities and complications. The value of this study lies in describing cases of emergency pediatric neurosurgery, in a holistic way, not interfering with details of management. This study reports the frequency of diagnosis in a tertiary hospital in northern Greece, as well as the characteristics of the pediatric neurosurgical patients (related to patients sex, age and preexisting comorbidities). In many cases we have described increased frequency of revisions or complications in specific subtotals of the study, though they might not seem to reach a point of statistical significance when comparing parameters.
A finding in this study, reaching the point of statistical significance was the possible influence of preexisting comorbidity regarding the need for revision operations (p = 0.0001). Regarding diagnosis our study seems to be in accordance with the literature, describing a high relative prevalence of hydrocephalus, traumatic brain injury (TBI) and Craniosynostosis as the most frequent diagnoses met in pediatric neurosurgical patients. The most frequent revision operations (in our study 31 % of all neurosurgical cases) seem to be surgery for cerebrospinal fluid (CSF) shunting. If this percentage is attributed to the total population undergoing CSF shunt procedures, it becomes 56.3% (36 CSF shunt revisions/64 total CSF shunting procedures). In the literature there are reports of approximately 35% revision operations concerning CSF shunting procedures.16 Reviewing the literature, our complications rate seems to be at a medium level (25%) while the literature reports a complications rate with great variation, from 16.4% to 39.9%.17,18
This fact may be explained by methodological differences concerning the study population (eg criteria of complications, emergency vs elective procedure, one procedure vs various procedures). As in every epidemiological retrospective (cohort) observational study, our investigation has weak points and possible bias.19 First of all the relatively short period of the study (31 months), having in mind the study period for epidemiological studies. This study seems to be a "snapshot" of the emergency pediatric neurosurgery cases. Another negative of this study was the need to determine a "start point" and a "end point" regarding cases that would contribute to the sample. This fact implies that some cases was analyzed as initial case while it really was a revision, and some cases were considered having no revision surgery although there is a possibility underwent revision after the study "end point". Also, the complications reported are all referring to this period of time. Of course that could lead someone to argue that complication rate might be underestimated in our study. On the other hand, we must take into account that complication from cases before the study "start point" (cases studied as initial though revision) was presented in the study period, leading to an increased rate of complication. This study reports a cumulative frequency of complications as result of many etiologies (preexisting comorbidities, anesthetic complications, surgery complications and ICU complications). Although the mentioned above is true, the study maintain its value, reporting a "holistic" rate of complications and maintains an alertness for pediatric neurosurgical patients management.
Emergency pediatric neurosurgical cases in northern Greece seem to present with a significant number of comorbidities. Approximately 70.7% of all surgical cases presented with at least one comorbidity. Males seems to be more susceptible requiring emergency neurosurgical intervention. The most frequent complications is infectious and postoperative hemorrhage. Female sex and revision surgery seems to increase the possibility of complications occurring. Preexisting comorbidity seems to increase the likelihood of revision surgery. This fact may be explained by taking into account that the most frequently performed operation is that of cerebrospinal fluid shunting and the most frequent complication is infection. The most frequent cause of CSF shunts failing is usually attributed to infection.20 The presence of infection increases the likelihood of CSF shunts failing. It also noticed that patients undergoing revision surgery is more prone to complications, although this fact did not reach a point of statistical significance (p=0.089). A significant conclusion-message regarding aseptic techniques and aggressive control of infections since it seems to be the main problem leading to a vicious circle (revisions and increased morbidity).
Evangelia Xanthaki RN, Paraskevi Parastati RN and Eleni Samara RN, nurses of the anesthesiology department for helping with anesthesia records.
The authors declare there is no conflict of interests.
None.

©2016 Petsas, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.