Journal of
eISSN: 2373-6437


Research Article Volume 1 Issue 3
1Department of Anesthesia, University of Pittsburgh Medical Center, USA
2Acute Interventional Perioperative Pediatric Postoperative Pain Management, University of Pittsburgh Medical Center, USA
3Department of Surgery, University of Pittsburgh Medical Center, USA
4Department of Anesthesiology, University of Pittsburgh Medical Center Presbyterian-Shadyside Hospitals Aiken Pittsburgh, USA
Correspondence: Mihaela Visoiu, Department of Anesthesiology, Acute Interventional Perioperative Pediatric Postoperative Pain Management, Childrens Hospital of Pittsburgh of Childrens Hospital Drive, 4401 Penn Avenue, Pittsburgh, PA 15224, USA, Tel 412-692-5260
Received: June 06, 2014 | Published: July 25, 2014
Citation: Visoiu M, Joy LN, Scholz S, et al. Continuous paravertebral nerve blockade for postoperative analgesia after video-assisted thoracoscopic surgery and chemical pleurodesis in children-a case series. J Anesth Crit Care Open Access. 2014;1(3):77‒81. DOI: 10.15406/jaccoa.2014.01.00016
Study objective: It is to compare continuous thoracic paravertebral blockade and thoracic epidural catheters for postoperative pain after VATS and chemical pleurodesis in children.
Design: Case series, retrospective chart review.
Setting: Children’s Hospital of University of Pittsburgh Medical Center.
Patients: We studied seventeen (17) pediatric patients who underwent VATS with chemical pleurodesis.
Interventions: Fourteen children (14) had continuous thoracic paravertebral blockade and three children (3) had thoracic epidural catheters.
Measurements and main results: Postoperative pain scores and consumption of analgesics were compared during the first 48 hours after surgery. Total length of hospital stay and complications secondary to analgesics and regional analgesia were analyzed and compared. Median pain scores were similar with P-values ranging from P = 0.13-0.76. Opioid consumption was not significantly different, with P-values for opioid morphine equivalency ranging from P= 0.13-0.96. Length of stay was significantly shorter for thoracic paravertebral group (3.86, SD±0.77) than for thoracic epidural group (5.00, SD±1.00) (P= 0.04). The rate of complications was low; frequency of nausea/emesis (P= 0.16) and itching (P= 0.60) was similar between groups.
Conclusion: Thoracic paravertebral analgesia and the thoracic epidural catheter were effective for our patients. The hospital stay was significantly shortened in paravertebral group, with only a few minor complications.
Keywords: Child, Acute postoperative pain, Pain-PACU, Regional, Local anesthetic, Thoracic paravertebral catheter
VATS, Video-Assisted Thoracoscopic Surgery; TE, Thoracic Epidural Catheter; TPVB, Thoracic Paravertebral Blockade; ASA, American Society of Anesthesiologists; ME, Morphine Equivalency of Opioids, POD, Post-Operative Day; PACU, Post Anesthesia Care Unit; LOS, Length of Stay; NRS, Numeric Rating Scale; PCA, Patient Controlled Analgesia; PSP, Primary Spontaneous Pneumothorax
Video-assisted thoracoscopic surgery (VATS), apical blebectomy and chemical pleurodesis are often combined to prevent recurrence of spontaneous pneumothorax.1,2 Postoperative pain arising from above procedures can be severe, leading to increased length of stay.2,3 Effective analgesia in the immediate post-operative period is necessary for optimal recovery, and satisfactory postoperative pain control for pediatric patients is even more important than in the adult population. To our knowledge, no study to date has assessed the efficacy of thoracic paravertebral blocks for postoperative pain control following pediatric VATS with chemical pleurodesis. In the current study, we sought to compare the effectiveness of continuous thoracic paravertebral blockade (TPVB) with our standard of care, thoracic epidural catheter (TE). We hypothesized that the pain scores and morphine equivalency of opioids (ME) consumption in the first 2 days after surgery are similar, with reduced rate of complications for TPVB, and similar hospital length of stay.
The University of Pittsburgh Institutional Board Review approved and deemed this study exempt from full committee review. Twenty-three (23) charts of pediatric patients that underwent VATS and pleurodesis at Children’s Hospital of University of Pittsburgh Medical Center, after June 1, 2009 and before January 6, 2013 were reviewed.
Inclusion and exclusion criteria
Cases were included if the patients were less than 18 years of age and underwent VATS and chemical pleurodesis, alone or combined with mechanical pleurodesis. The patients were not excluded if they underwent more than one VATS with chemical pleurodesis on two different admissions. The patients were excluded if they were ≥18 years, underwent bilateral VATS or VATS and mechanical pleurodesis only, remained intubated at the end of the procedure, and had more than one paravertebral catheter placed. Details about surgical procedure, multimodal and regional perioperative analgesia, and postoperative pain scores (up to 48 hrs after end of surgery), and demographics were collected from the patient chart. The patients were assigned to one of two groups: TPVB group, who had unilateral continuous thoracic paravertebral blockade and multimodal analgesia or TE group, who had continuous thoracic epidural blockade and multimodal analgesia. We analyzed and compared Numeric Rating Scale (NRS) pain scores and analgesics consumption from intraoperative period, PACU stay, and floor stay on postoperative (POD) 0, POD 1, and on POD 2 (until midnight). Additionally, side effects from opioids administration (nausea, emesis, itching, and respiratory depression) and complications from regional anesthesia, duration of intravenous patient controlled analgesia (PCA) and continuous regional analgesia, anesthesia and surgery duration, time required for catheter placement, length of PACU and overall hospital stay (LOS) were compared between the two groups.
The primary end-point was median NRS floor pain scores as documented in patient’s record, until POD 2 (midnight). The secondary end points were the total amount of morphine (mg/kg), hydromorphone (mcg/kg), oxycodone (mg/kg), hydrocodone (mg/kg), fentanyl (mcg/kg), morphine equivalency (ME) of opioids (mg/kg), Ketamine (mcg/kg), acetaminophen equivalency (mg/kg), ketorolac (mg/kg), gabapentin (mg/kg) used intraoperative, 24, and 48 hours postoperatively and the hospital LOS. Hospital discharge criteria for patients undergoing VATS were based on three different factors. After pleurodesis, especially with talcum, there is a large amount of pleural inflammation, which leads to drainage. Prior to discharge, the drainage has to come down for the chest tube to come out. Usual drainage amounts are 40 ml per 12 hours, but can vary by surgeon and age of the child. Additionally, adequate pain control must be achieved prior to discharge as well as the general wellbeing of the patient.
Statistical analysis
Descriptive statistics were computed for the cohort. T-tests were performed to determine significant differences between the two groups. Chi-square was used to compare patient gender, ASA class, and procedure type (chemical pleurodesis only, and chemical and mechanical pleurodesis). All statistical analyses were two-sided, and the p significance level was set at 0.05. Data was analyzed using PASW statistics 21.0 (released August 14, 2012; SPSS Inc., Chicago, IL).
Descriptive statistics
Twenty-three (23) patients underwent VATS with chemical pleurodesis. Four subjects were excluded because they did not have regional anesthesia, and one had VATS on the contra lateral side on POD 2. Data from 17 patients (13 male, 4 female, 15.65±1.11 years of age) who underwent VATS with chemical pleurodesis were included in final analysis. Two patients had VATS with chemical pleurodesis on the contra lateral side on two different admissions; one patient had TE and TPVB and one patient had TPVB twice, as per current practice of the pain attending. Fourteen (14) patients from TPVB group and 3 patients from TE group were compared in terms of gender, age, weight, height, body mass index (BMI), and ASA, anesthesia, and surgery characteristics. There was no clinically meaningful difference between the groups in their baseline characteristics. There was no statistically significant difference in the duration of chest tube or duration of regional anesthesia catheter (Table 1).
|
TPVB Group (n=14) |
TE Group (n=3) |
P Value |
Age (Years) |
15.57 ( 1.16) |
16.00 ( 1.00) |
0.56 |
Weight (Kg) |
54.45 ( 7.67) |
57.03 ( 9.57) |
0.62 |
Height (cm) |
168.17 ( 14.07) |
179.81 (11.62) |
0.21 |
BMI |
18.31 ( 1.68) |
17.53 ( 0.75) |
0.46 |
Gender, n (%) |
|
|
1.00 |
Female |
3 ( 21.4 ) |
1 (33.3 ) |
|
Male |
11 ( 78.6 ) |
2 (66.7 ) |
|
ASA Class, n (%) |
|
|
0.18 |
I |
|
|
|
II |
14 (100 ) |
2 (66.7 ) |
|
III |
|
1 (33.3 ) |
|
Chemical Pleurodesis, n (%) |
7 ( 50 ) |
1 (33.3 ) |
|
Chemical and Mechanical Pleurodesis, n (%) |
7 ( 50 ) |
2 (66.7 ) |
|
Surgical Time (min) |
47.50 ( 12.09) |
69.00 (30.41) |
0.34 |
Anesthesia Time (min) |
133.86 ( 22.92) |
145.33 (33.71) |
0.48 |
Block Time (min) |
14.07 ( 3. 1 ) |
14.67 (10.02) |
0.93 |
Chest Tube (days) |
4.00 ( 0.88) |
4.33 ( 1.53) |
0.60 |
TPVB (days) |
3.86 ( 0.86) |
|
0.46 |
TE (days) |
|
4.33 ( 1.53) |
|
PACU Stay (min) |
128.36 ( 46.12) |
75.33 (21.60) |
0.08 |
Length of Stay (days) |
3.86 ( 0.77) |
5.00 ( 1.00) |
0.04* |
Table 1 Demographics, surgical and anesthetic characteristics
Data is presented as mean and SD for continuous variables and n (%) for categorical variables
TPVB, Thoracic Paravertebral Blockade; TE, Thoracic Epidural Catheter; ASA, American Society of Anesthesiologists Physical Status Classification; PACU, Postoperative Anesthesia Care Unit; *p <0.05
Regional anesthesia
In the TE group, using the classical technique, the catheters were placed at T7 vertebral level under general anesthesia for 2 patients and under sedation for one patient. In the TPVB group, 4 patients had the blocks performed under sedation and three TPVB catheters were inserted under general anesthesia. The level for TPVB varied from case to case; 2 catheters were inserted at T4 vertebral level, 5 at T5 level, and one at T6, T7, T8 and T9 level. The level was not documented in 3 cases. Six (6) paravertebral catheters were placed using the classical technique. After August 2011, 8 patients in the TPVB group had the catheter placed under ultrasound guidance as described by Boretsky et al.4
Pain scores
There was no statistically significant difference in the mean of NRS median pain scores recorded until the end of POD 2 (TPVB group, 3.46, SD±1.45; TE group, 4.33, SD±2.08; P= 0.39). There was no statistically significant difference in the mean of median pain scores during PACU stay (P= 0.24), or floor stay on POD 0 (P= 0.76), POD 1 (P= 0.13), POD 2 (P= 0.69) (Figure 1).
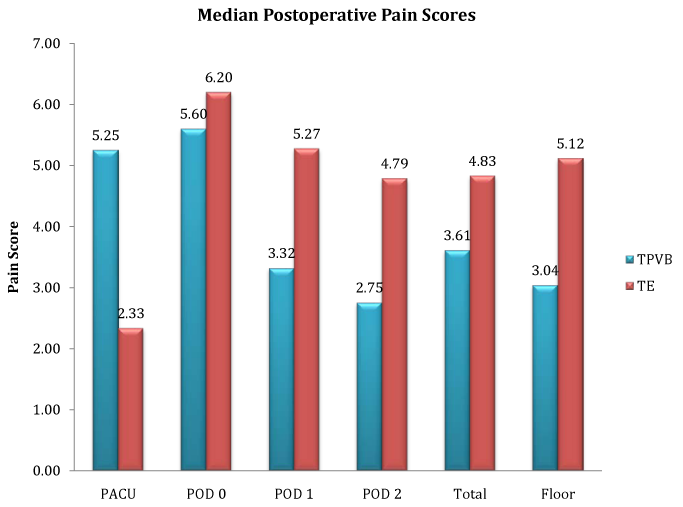
Figure 1 Postoperative pain scores.
Pain scores represent means of Numeric Rating Scale (NRS) pain scores; TPVB, Thoracic Paravertebral Group; TE, Thoracic Epidural Group; PACU, Postoperative Anesthesia Care Unit
POD 0 is day of surgery, POD 1 is postoperative day 1, POD 2 is postoperative day 2, and Total represents pain scores documented after surgery until midnight of POD 2.
Analgesics administration
During intraoperative period, the patients received fentanyl, morphine, and hydromorphone. There was no statistically significant difference in the ME administered intraoperative (P= 0.26) (Figure 2). The same medications were administered during PACU stay, with no difference between the 2 groups (P= 0.13) (Figure 3). For the first 2 postoperative days, multimodal analgesia consisted of hydromorphone via patient controlled analgesia (PCA) or as rescue intravenous (iv) doses, morphine via PCA or as rescue iv doses, Ketamine via PCA, ketorolac iv, oxycodone by mouth (po) (alone or in combination with acetaminophen), hydrocodone-acetaminophen po, gabapentin po and acetaminophen po. There was no statistically significant difference in ME on POD 0 (P= 0.78), on POD 1 (P= 0.96), on POD 2 (P= 0.44) and overall ME (P= 0.55) (Figure 2). In the TE group, no patients received oxycodone on POD 0 or POD 1, or Ketamine and gabapentin during hospital stay. In the TPVB group, total Ketamine consumption was 1 mg/kg and 5 patients received gabapentin (8.02 mg/kg, SD±12.06). There was no statistically significant difference in acetaminophen equivalency (TPVB=53.22, SD±48.9 vs. TE = 30.58, SD±52.97) (P= 0.48), or ketorolac (TPVB = 0.04, SD±0.14 vs. TE = 0.08, SD ± 0.15) (P= 0.59) (Figure 3).
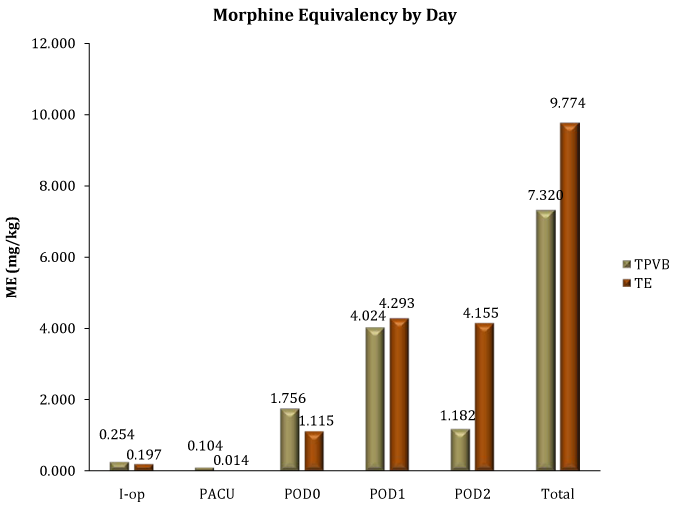
Figure 2 Morphine equivalency by day.
TPVB, Thoracic Paravertebral Group; TE, Thoracic Epidural Group; ME, Morphine Equivalency of opioids; IOP, Intraoperative Period; PACU, Postoperative Anesthesia Care Unit; POD, Postoperative Day
POD 0 is day of surgery, POD 1 is postoperative day 1, POD 2 is postoperative day 2, and total represents ME documented after surgery until midnight of POD 2.
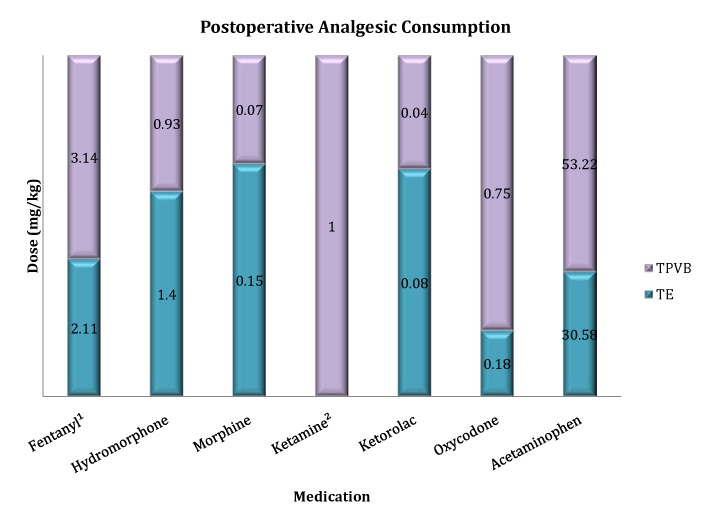
Figure 3 Postoperative analgesic consumption.
TPVB, Thoracic Paravertebral Group; TE, Thoracic Epidural Group
1Dose (mcg/kg)
2Ketamine only administered in the TPVB group
Local anesthetic administration
The total amount of ropivacaine (0.5% or 0.2%) administered intraoperative was 1.48 mg/kg (SD±0.54) in the TPVB group and 0.72 mg/kg (SD±0.13) in the TE group (P= 0.03). Each patient in the TE group received 3 ml of lidocaine 1.5 % with epinephrine 1/ 200000. The total amount of ropivacaine (0.2%) administered was 18.14 mg/kg (SD±6.07) in the TPVB group and 20.8 mg/kg (SD±1.6), in the TE group (P= 0.48).
Complications
There was no difference in incidence of nausea/emesis (P= 0.16), or itching (P= 0.60). No episodes of respiratory depression were documented in either group. Complications included a small leak of local anesthetic at the catheter insertion site (2) and disconnection of the paravertebral catheter (1), all in the TPVB group. Two patients had a Foley catheter in each group; however, the catheters were removed after 3 days in the TPVB group and 5 days in the TE group. There was no statistically significant difference in the duration of chest tube or duration of catheter for regional anesthesia (Table 1).
Length of hospital stay
The TPVB group had a significantly shorter LOS (days) than the TE group (TPVB=3.86, SD±0.77 vs. TE=5.00, SD±1.00) (P= 0.04). Moreover, there was a trend toward spending more time in the PACU for the TPVB group (P= 0.08) (Table 1).
A primary spontaneous pneumothorax (PSP) occurs without a precipitating event. Most individuals have unrecognized lung disease, with the pneumothorax resulting from rupture of a sub pleural bleb.5 Recurrences occur in more than 50% of cases, most commonly within the first year.6 Initial treatment options for PSP include observation, supplemental oxygen, needle aspiration of intra pleural air or tube thoracostomy depending on clinical preferences and circumstances. Video-assisted thoracoscopy (VATS) is preferred for children with persistent air leak or recurrence of spontaneous pneumothorax.7 VATS is highly effective in the treatment of pneumothorax reducing recurrence rates to below 5%. During VATS, an endoscopic stapler is used to resect pulmonary blebs or bullae, which can be readily identified on the lung surface. Pleural symphysis is created by mechanical pleurodesis or chemical pleurodesis using talc or tetracycline derivative. Chemical pleurodesis, in particular, is associated with intense chest pain requiring multimodal perioperative pain control and a longer postoperative course of chest tube drainage, both leading to increased hospital stays.2,3
Satisfactory post-operative analgesia is necessary for optimal recovery. In a study done by Ozcan et al.1 22 children who underwent VATS and chemical or mechanical pleurodesis used PCA for postoperative analgesia. Multiple intercostal nerve blocks, two levels above and below chest tube were performed only for the patients with severe respiratory insufficiency.1 Moreover, the etiology of the pain is thought to be multi factorial, including tissue injury at the thoracoscopic instrument and chest tube sites (incisional pain), chemical irritation of the pleura (visceral pain), and diaphragmatic irritation (shoulder pain). The perioperative use of non-steroidal anti-inflammatory drugs negatively affects the quality of pleural adhesion obtained after mechanical pleurodesis in a pig model,8 and their use is controversial. Although multimodal analgesic regimens can be used to treat postoperative pain, the severity of pain prompts the pain specialists to use continuous thoracic epidural analgesia as technique of choice.
Over the last years, many anesthetic practices have changed and we noticed a trend away from neuraxial anesthetic techniques in favor of using peripheral nerve block techniques with an improved safety record.9,10 Many studies agreed that thoracic paravertebral blockade is at least as effective as TE analgesia for pain control post-thoracotomy,11‒14 but none compared TPVB with TE for postoperative pain control after VATS chemical pleurodesis in adult or pediatric patients. The chest wall is innervated by intercostal nerves, however, the visceral pleura are not, and the parietal pleura are innervated by the intercostal and phrenic nerves. Thoracic paravertebral nerve blocks result in somatic and sensory blockade of multiple contiguous dermatomes above and below the site of injection.15 Postoperative analgesia from one paravertebral catheter or TE is not sufficient and multiple adjuvant pain modalities are required. At our institution, TE was considered standard of care for pediatric postoperative pain control after VATS and chemical pleurodesis. However, awareness of complications after epidural analgesia10,16‒20 changed our practice and continuous paravertebral nerve blocks,11‒15,21‒24 replaced epidural analgesia for postoperative pain management for many surgical procedures. At our institution, only 9% of our regional catheters were TE in 2013, compared with 24% in 2010. For VATS with chemical pleurodesis TPVB replaced almost entirely TE; for these 23 cases, the last TE being done in November 2011.
Unsatisfactory analgesia, the duration of chest tubes and regional anesthesia with continuous catheters can affect the patients hospital stay. Duration of chest tube was 4.6 days (range 2-12 days) in Ozcan et al.1 study and this is consistent with our findings. The TPVB and TE catheters did not increase patients LOS; they were removed earlier or at the same time with chest tubes. In our study, the hospital length of stay was shorter in the TPVB group despite previously enumerated confounding factors. Majority of patients in this group did not have Foley catheters in the postoperative period and it is our subjective observation that this increased patients’ and surgeons’ satisfaction. As we predicted, pain scores and analgesics consumption were similar for our two groups. There are several limitations to our study. The pain scores were extracted from patients’ charts as documented by nursing staff. Pain was regularly assessed, minimum every 4 hours, but we do not know if pain scores were documented during rest or upon mobilization. Due to the retrospective nature of this report, we could not control for the type of medication used, dose, or criteria for administration. We compared daily medication consumption and in order to account for different pain medications, the totals of all opioids were converted to ME and the total of acetaminophen to acetaminophen equivalence. Ketamine and Gabapentin were administered only in the TPVB group, but the dose was small and with minimal contribution to the total amount of analgesics administered. We hoped for an equal amount of patients in both groups, but we ended with a reduced number of cases in the TE group because our practice had changed. However, in both groups, the amount of medication is similar and the pain scores were mild to moderate.
This case series support continuous thoracic paravertebral catheter in combination with multimodal analgesia as a feasible intervention to reduce perioperative pain associated with VATS with chemical pleurodesis in pediatric patients. Length of stay was significantly shorter for the TPVB group than for the TE group, with few minor complications in the TPVB. Additional prospective data is needed to compare these two postoperative analgesic techniques and validate TPVB.
None.
None.
Authors declare that there is no conflict of interest.

©2014 Visoiu, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.