Journal of
eISSN: 2373-6437


Research Article Volume 2 Issue 5
Department of Anesthesiology and Pain Medicine, University of Washington, USA
Correspondence: Lollo L, Department of Anesthesiology and Pain Medicine, University of Washington,1959 NE Pacific St, BB-146, Seattle, WA 98195-6540, USA, Tel 206-744-2881, Fax 206-7446240
Received: May 22, 2015 | Published: August 6, 2015
Citation: Lollo L, Stogicza A (2015) Comparison of Analgesic Outcomes Following Sciatic Nerve Blockade Performed by Resident Trainees and Nurse Anesthetists. J Anesth Crit Care Open Access 2(5): 00070. DOI: 10.15406/jaccoa.2015.02.00070
Background and objectives: Peripheral nerve blockade requires regional anesthesia skills that are taught in several formats and assessing technical proficiency has shifted from fulfillment of quotas to comprehensive procedural evaluation. Complete analgesia is the clinical endpoint validating successful nerve blockade but patient, technical and procedural factors influence this result. The purpose of this study was to determine if physician trainee or nurse anesthetist administered sciatic nerve blockade influence postoperative pain scores and opioid analgesic requirements and if patient factors, technique and repetition influence this outcome.
Method: Sciatic nerve blockade by nerve stimulation and ultrasound based techniques were performed by senior anesthesiology resident trainees and nurse anesthetists under the supervision of regional anesthesia faculty. Preoperative patient characteristics including obesity, trauma, chronic pain, opioid use and preoperative pain scores were recorded and compared to the post-procedure pain scores and opioid analgesic requirements upon discharge from the post-anesthesia care unit and 24 hours following sciatic nerve blockade.
Results: 93 patients received sciatic nerve blockade from 22 nurse anesthetists and 21 residents during 36 months. A significant relation between training background and improved pain scores was not demonstrated but transition from nerve stimulation to ultrasound guided techniques lowered immediate opioid usage in all groups. Patients with pre-existing chronic opioid use had higher postoperative pain scores and opioid dosages following nerve block.
Conclusion: Patient analgesia should be an integral measure of proficiency in regional anesthesia techniques and evaluating this procedure outcome for all practitioners throughout their training and beyond graduation will longitudinally assess technical expertise.
RA: Regional Anesthesia; US: Ultrasound; CUSUM: Cumulative Summation Statistical Methods; SNB: Sciatic Popliteal Nerve Blockade; BMI: Calculated Body Mass Index; MS: Morphine Sulfate; NS: Nerve Stimulator; ASA: American Society of Anesthesiologists; PACU: Post-Operative Care Unit; VAS: Visual Analog Scale
Regional anesthesia (RA) techniques are a core component of the practice of anesthesiology and it has been shown that trainees completing a minimal quota of procedures did not acquire all of the skill sets necessary to perform an appropriately selected, timely, safe and successful nerve block.1 Training programs have adopted regional anesthesia rotations with expert faculty in order to teach senior resident trainees these skills by incorporating adjunctive teaching methods including simulation, cadaver dissection, robotics and web-enhanced didactics.2 These instruction modalities have improved the learning experience and the overall competency for residents performing these techniques and in particular the visuospatial coordination required for ultrasound (US) guided procedures.2-4 Global procedural scores and performance times for axillary and inter-scalene brachial plexus nerve blockade for both trainees and practitioners demonstrated improvement in these parameters that was related to the number of procedures completed and weeks in training.5,6 Clinical outcomes monitored by cumulative summation (CUSUM) statistical methods demonstrate resident variability in the number of repetitions necessary to acquire the minimal standard of technical proficiency for any given procedure.7 Sciatic popliteal nerve blockade (SNB) placed by podiatry residents had an overall success rate of 72.4% with no difference in this proportion with respect to months of training.8 The consensus for a successful nerve block is one that requires no further analgesia or intervention for pain relief.9 The objective quantification of a subjective pain score is influenced by many patient variables but this critical parameter assesses successful nerve blockade and is an important marker of clinical proficiency. The purpose of this study was to determine if the success rate of postoperative SNB for analgesia measured by postoperative pain scores and opioid requirements is influenced by the performance of the procedure by the training background of senior residents and nurse anesthetists (CRNAs). Further objectives of this study were to determine if specific preoperative patient factors, procedural technique and repetition of SNB by trainees and nurse anesthetists influenced this outcome.
After receiving institutional review board approval from the University of Washington Human Subjects Division, patients provided written informed consent prior to undergoing elective foot and ankle surgery and were enrolled for participation in this prospective study of the perioperative analgesic effects of popliteal sciatic nerve blockade. All procedures were performed at Harborview Medical Center, Seattle between October 2009 and November 2012. The preoperative data collected were age, gender, ASA physical status, height, weight, calculated body mass index (BMI), recent traumatic lower extremity injury, pre-existing lower extremity neuropathy or chronic pain, worst pain score in the preceding 24 hour interval and maintenance preoperative 24 hour opioid dosage converted to mg of intravenous morphine sulfate (MS). All patients received general inhalational endotracheal anesthesia with sevoflurane and Intraoperative analgesia in the form of intravenous fentanyl, morphine and/or hydromorphone for their surgery. The dosages of Intraoperative opioid administered were recorded for each patient. Postoperative analgesia in those patients with inadequate pain relief following sciatic nerve blockade was administered as intravenous fentanyl, morphine and/or hydromorphone and oral oxycodone in bolus doses in the immediate postoperative period and as patient controlled analgesic infusions in the 24 hour period following surgery. In order to quantify the opioids administered to patients in equivalent dosing units and to compare the opioid usage between patients as a result of the variety of analgesic narcotic medications administered peri-operatively due to both patient and prescribing practitioner preferences, all dosages were converted to equipotent values in mg of intravenous morphine sulphate using standardized opioid conversion formulae. Postoperative popliteal sciatic nerve blockade by the lateral approach at a point 10 cm proximal to the popliteal crease was performed in the post anesthesia care unit by either senior anesthesiology residents or nurse anesthetists supervised by regional anesthesia physician faculty with added expertise in ultrasound guided imaging. All patients were administered 25 ml 0.375% (93.7 mg) bupivacaine for the SNB using a Life-Tech ProBloc II 20 Gauge 100mm 30 degree bevel needle. The procedure was performed in the first 18 months of the study with the use a Life-Tech Tracer III nerve stimulator (NS) and the dose of local anesthetic was injected when toe plantar flexion was observed at a current of less than 0.6 mA. In the second 18 month interval the procedure was performed under ultrasound (US) guidance using a Sonosite M Turbo with a linear 38mm probe to locate the sciatic nerve in the short axis view proximal to its branch point and the local anesthetic was injected when the needle tip was observed to be within close proximity to the nerve using the in plane visualization technique. The patient self-reported pain scores, observation of toe plantar flexion and the total postoperative opioid dosages converted to mg of intravenous MS were recorded both at the time of PACU discharge and at 24 hours following SNB.
93 patients were enrolled during the 36 month study interval. 48 patients received SNB from 22 different CRNAs and 45 were administered SNB from 21 senior anesthesiology resident trainees. The preoperative demographics for the enrolled patients for gender, age, American Society of Anesthesiologists (ASA) physical status, body mass index (BMI), preoperative and Intraoperative opioid doses in mg of intravenous MS are summarized in Table 1. The patients are categorized according to the training background of the practitioner and the guidance technique used for administering the SNB and their respective pain scores and opioid dosages in the immediate post-operative care unit (PACU) and at 24 hours following SNB are also presented in Table 1 and these same data are graphically presented in Figures 1a&1b & 2a&2b. Some practitioners had opportunities to repeat SNB on enrolled patients during the study period and the immediate PACU pain scores were recorded according to training background, SNB guidance technique and the numbered sequence of repetition and these are presented in Figure 3.
|
Opioid naive |
Nerve stimulator |
Nerve stimulator |
Ultrasound guided |
Ultrasound guided |
|
Female Patients (n = 38) |
||||
|
Level of Training (#Trainees) |
Residents (5) |
CRNAs (10) |
Residents (6) |
CRNAs (9) |
|
Patients (n) |
5 |
11 |
10 |
12 |
|
Age |
54.4 (5.2) |
54.45 (14.47) |
58 (11.14) |
48.83 (15.3) |
|
ASA Status |
2 (1) |
2 |
2 |
2 (1) |
|
BMI |
30.7 (6.2) |
27.12 (4.47) |
31.58 (5.66) |
26.42 (4.56) |
|
Preoperative Pain Score |
7 (1) |
5 (4) |
6 (4) |
6 (4) |
|
Preoperative Opioids |
18.5 (32.2) |
7.73 (16.03) |
8.63 (15.03) |
10.5 (13.43) |
|
Intraoperative Opioids |
35.2 (16.4) |
30.97 (14.9) |
41.13 (29.22) |
31.43 (16.47) |
|
1 Hour Discharge Pain Score |
4 (3) |
3 (3) |
3 (3) |
2 (3) |
|
1 Hour Discharge Opioids |
21.6 (16.2) |
20.27 (24.91) |
16.67 (19.16) |
8.05 (8.4) |
|
24 Hour Pain Score |
4 (4) |
4 (2) |
4 (3) |
5 (3) |
|
24 Hour Opioids |
83.9 (68.7) |
59.44 (44.84) |
171.3 (339.5) |
107.24 (92.6) |
|
Male Patients (n = 55) |
||||
|
Level of Training (#Trainees) |
Residents (6) |
CRNAs (7) |
Residents (12) |
CRNAs (9) |
|
Patients (n) |
8 |
13 |
20 |
12 |
|
Age |
49.88 (17.17) |
53.23 (15.6) |
53.16 (14.53) |
48 (16.35) |
|
ASA Status |
2 |
2 (1) |
2 (1) |
2 (1) |
|
BMI |
28.37 (4.64) |
27.57 (3.33) |
26.85 (4.68) |
33.18 (18.36) |
|
Preoperative Pain Score |
5 (3) |
4 (3) |
5 (4) |
5 (3) |
|
Preoperative Opioids |
6.88 (11) |
9.62 (22.59) |
18.2 (25.39) |
6.84 (11.57) |
|
Intraoperative Opioids |
41.96 (6.72) |
45.9 (23.6) |
32.17 (17.04) |
37.09 (17.11) |
|
1 Hour Discharge Pain Score |
3 (2) |
1 (2) |
2 (3) |
2 (3) |
|
1 Hour Discharge Opioids |
15.58 (20.22) |
13.32 (22.14) |
3.92* (6.82) |
3.83 (7.49) |
|
24 Hour Pain Score |
2 (2) |
3 (2) |
5 (2) |
4 (3) |
|
24 Hour Opioids |
94.45 (58.19) |
58.64 (43.91) |
107.1 (147) |
62.78 (62.73) |
Table 1 Patient demographics and perioperative pain scores and opioid doses following sciatic nerve blockade categorized by guidance technique and practitioner category
Data reported are mean (SD). SNB: Sciatic Nerve Blockade; BMI: Body Mass Index, Opioid doses converted to mg of intravenous Morphine Sulfate.
* p< 0.05 by paired t-test.
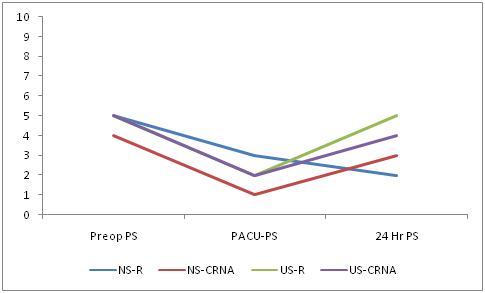
Figure 1B Male Patients.
Figure 1 Perioperative mean pain scores (PS) in the preoperative (Preop), PACU discharge and at 24 hours post sciatic nerve blockade characterized by nerve stimulator (NS) and ultrasound (US) guidance technique and level of practitioner training as either resident trainee (R) or nurse anesthetist (CRNA).

Figure 2B Male patients.
Figure 2 Perioperative mean total opioid dosages expressed as mg intravenous morphine sulphate in the preoperative (Preop), intraoperative (Intraop), PACU discharge and at 24 hours post sciatic nerve blockade characterized by nerve stimulator (NS) and ultrasound (US) guidance technique and level of practitioner training as either resident trainee (R) or nurse anesthetist (CRNA).
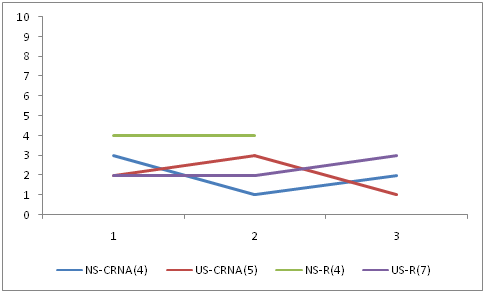
Figure 3 Mean pain scores plotted for repetition of sciatic nerve blockade with either nerve stimulator (NS) or ultrasound (US) guidance for nurse anesthetists (CRNA) and resident trainees (R). Numbers in parentheses indicate number of practitioners observed in each group. Vertical axis represents pain score and horizontal axis is the sequence of repetition of the procedure.
The patient characteristics were comparable for gender, age, ASA physical status, BMI and Intraoperative opioid doses and no significant demographic differences were observed between the patient groups. The technique for performing SNB varied because the group practice changed from using NS to US guidance for SNB at the beginning of month 19. All patients had intact motor function of the foot after SNB. Postoperative pain scores on discharge from PACU following SNB trended lower for the US patients compared to the NS groups for all training levels but this did not reach statistical significance. Improvement in pain control with US guided SNB has been reported by others and the observed lower postoperative opioid requirement for analgesia in the US groups compared to the NS groups supports this finding and in males administered SNB by the resident group this reached statistical significance. A relation between level of RA expertise according to academic background and improved pain scores was not demonstrated but there was slight improvement in this parameter with the transition from NS to US guided SNB in all groups.
Repetition of SNB by practitioners during the course of the study demonstrated a downward trend in both NS and US guided techniques but the group sizes and number of repeat observations were both small. The regional anesthesia curriculum for all practitioners was maintained constant through the course of this study and is summarized in Table 3. Decreasing pain scores with repetition and consistently successful SNB outcomes would support the notion that the practitioner is advancing in clinical proficiency for this technique. Patients receiving preoperative chronic maintenance opioid therapy have been reported elsewhere to be challenging for the success of peripheral nerve blockade for postoperative analgesia.10 Subgroup analysis for the influence of preoperative opioid analgesics on the postoperative pain scores and opioid analgesic supplementation was performed and this is summarized in Table 2. All chronic opioid using patient groups were observed to have higher postoperative pain scores and opioid analgesic usage in both PACU and at 24 hours compared to the opioid naive groups, for every practitioner group and guidance technique. These data are graphically presented in Figures 4a&4b & 5a&5b. Statistical analysis could not be performed due to the small sample sizes of some of these subcategories of patients. The differences in the dosages of opioid analgesia required at 24 hours for opioid tolerant patients indicate that SNB provides some initial pain relief but that this effect is short-lived and a “hyper-algesicrebound” effect occurs once the local anesthetic dissipates.
|
Opioid naive |
Nerve stimulator |
Nerve stimulator |
Ultrasound guided |
Ultrasound guided |
|
Female (n = 22) |
||||
|
Level of training (#Trainees) |
CRNAs (5) |
Residents (2) |
CRNAs (5) |
Residents (4) |
|
Number (n) |
8 |
2 |
7 |
5 |
|
Age (yrs) |
55 (16.2) |
58.5 |
53.6 (18) |
62.8 (4) |
|
BMI |
26 (3.94 |
33.7 |
27 (5.8) |
30.1 (5.1) |
|
ASA |
2 |
2 |
3 |
2 |
|
Preoperative Pain Score |
4 (3) |
7 |
6 (3) |
3 (3) |
|
Preoperative Opioid Dose |
0 |
0 |
0 |
0 |
|
Intraoperative Opioid Dose |
32.9 (13.8) |
25.2 |
25.4 (13.8) |
26.4 (11.7) |
|
1 Hour Pain Score |
3 (3) |
5 |
1 (2) |
2 (3) |
|
1 Hour Opioid Dose |
21.3 (29) |
8.3 |
5.3 (7.6) |
12.6 (20.1) |
|
24 Hour Pain Score |
5 (2) |
2 |
3 (3) |
2 (1) |
|
24 Hour Opioid Dose |
56.2 (35.2) |
49.7 |
56.7 (79.4) |
33.1 (24.9) |
|
Male (n = 34) |
||||
|
Level of training (#Trainees) |
CRNAs (6) |
Residents (5) |
CRNAs (7) |
Residents (10) |
|
Number (n) |
10 |
5 |
7 |
12 |
|
Age (yrs) |
54.1 (17.3) |
46.4 (17.4) |
49.8 (14.2) |
57.3 (14.3) |
|
BMI |
27.7 (3.6) |
26.8 (4.5) |
39.8 (24.4) |
27 (4.8) |
|
ASA |
2 |
2 |
2 (1) |
2 (1) |
|
Preoperative Pain Score |
3 (3) |
5 (3) |
5 (3) |
4 (4) |
|
Preoperative Opioid Dose |
0 |
0 |
0 |
0 |
|
Intraoperative Opioid Dose |
43.3 (20.7) |
41.9 (7.7) |
30.9 (10.6) |
26 (14.6) |
|
1 Hour Pain Score |
1 (1) |
4 (2) |
2 (3) |
1 (1) |
|
1 Hour Opioid Dose |
9.8 (15) |
14.3 (15.6) |
5.2 (9.1) |
2.8 (3) |
|
24 Hour Pain Score |
2 (2) |
2 (2) |
3 (3) |
4 (2) |
|
24 Hour Opioid Dose |
50 (38.9) |
100.2 (69.7) |
45.6 (38.5) |
36.7 (24.3) |
|
Opioid tolerant |
Nerve stimulator |
Nerve stimulator |
Ultrasound guided |
Ultrasound guided |
|
Female (n = 16) |
||||
|
Level of training (#Trainees) |
CRNAs (3) |
Residents (3) |
CRNAs (5) |
Residents (5) |
|
Number (n) |
3 |
3 |
5 |
5 |
|
Age (yrs) |
56 |
51.7 |
42.2 (7.9) |
53.2 (14.3) |
|
BMI |
27.3 |
28.7 |
25.6 (2.3) |
33.1 (6.4) |
|
ASA |
2 |
1 |
2 |
2 (1) |
|
Preoperative Pain Score |
5 |
7 |
6 (5) |
9 (2) |
|
Preoperative Opioid Dose |
28.3 |
30.8 |
25.2 (5.7) |
17.3 (17.9) |
|
Intraoperative Opioid Dose |
26 |
41.9 |
39.9 (17.5) |
55.9 (35.3) |
|
1 Hour Pain Score |
3 |
4 |
4 (2) |
4 (4) |
|
1 Hour Opioid Dose |
14 |
30.5 |
12 (8.6) |
20.7 (19.6) |
|
24 Hour Pain Score |
3 |
6 |
7 (2) |
5 (4) |
|
24 Hour Opioid Dose |
69.1 |
106.7 |
178 (58.1) |
281.9 (442.4) |
|
Male (n = 20) |
||||
|
Level of training (#Trainees) |
CRNAs (2) |
Residents (3) |
CRNAs (5) |
Residents(6) |
|
Number (n) |
3 |
3 |
6 |
8 |
|
Age (yrs) |
50.3 |
55.7 |
48.2 (19.5) |
46.1 (13) |
|
BMI |
27 |
31.4 |
25.6 (6.3) |
26.6 (4.5) |
|
ASA |
2 |
2 |
2 (1) |
2 (1) |
|
Preoperative Pain Score |
8 |
5 |
6 (3) |
6 (3) |
|
Preoperative Opioid Dose |
41.7 |
18.3 |
13.7 (13.5) |
45.5 (27.3) |
|
Intraoperative Opioid Dose |
54.4 |
42 |
43.3 (20.9) |
41.1 (16.4) |
|
1 Hour Pain Score |
4 |
2 |
2 (2) |
3 (4) |
|
1 Hour Opioid Dose |
25.1 |
17.7 |
2.4 (6) |
5.7 (10.1) |
|
24 Hour Pain Score |
6 |
2 |
6 |
6 (2) |
|
24 Hour Opioid Dose |
87.4 |
84.9 |
80 (80.2) |
187.4 (179.4) |
Table 2 Demographics and perioperative pain scores and opioid dosages of opioid naïve and opioid tolerant patients receiving sciatic nerve blockade categorized by guidance technique and practitioner category
|
Academic year of training |
Curricular intervention |
|
|
Internship (R-1) |
4 week acute pain service (APS) rotation |
|
|
Pain related didactic lectures |
|
|
|
First (R-2 / CA-1) |
4 week regional anesthesia didactic block including problem based learning (PBLD) |
|
|
Second (R-3 / CA-2) |
4 week acute pain service (APS) rotation |
|
|
One day cadaver based regional anesthesia workshop |
|
|
|
Third (R-4 / CA-3) |
One day cadaver based regional anesthesia workshop |
|
|
One day ultrasound phantom based training workshop |
|
|
|
One day intensive regional anesthesia board review didactic workshop |
|
Table 3 University of Washington Anesthesiology Residency Regional Anesthesia Training Curriculum
Data expressed as mean (SD) where appropriate.
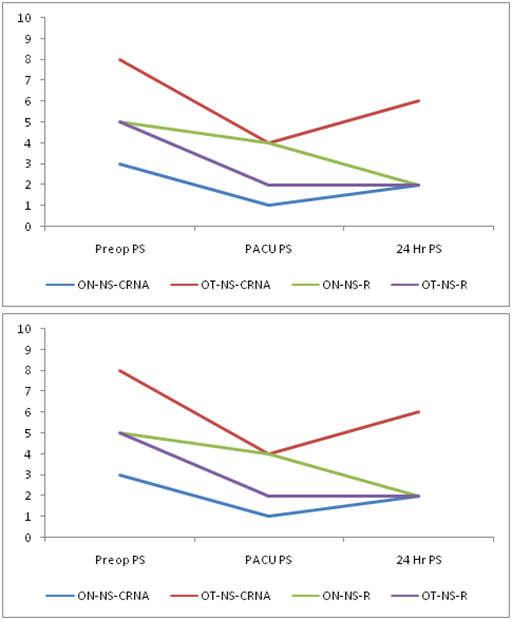
Figure 4B Male Patients.
Figure 4 Perioperative mean pain scores (PS) for opioid naïve (ON) and tolerant (OT) patients in the preoperative (Preop), PACU discharge and at 24 hours post sciatic nerve blockade characterized by nerve stimulator (NS) and ultrasound (US) guidance technique and level of practitioner training as either resident trainee (R) or nurse anesthetist (CRNA).
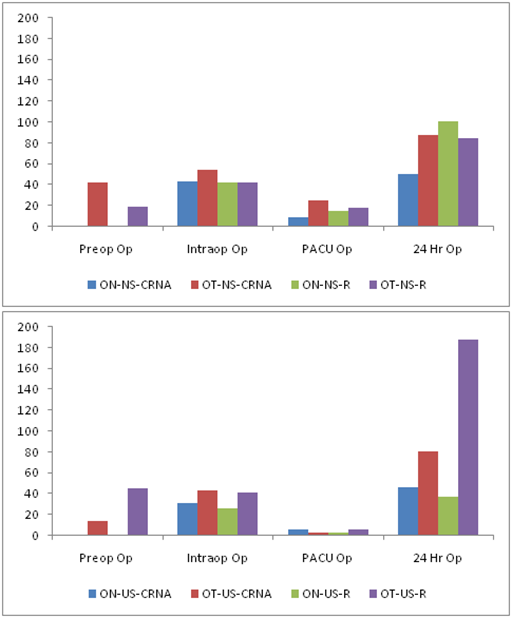
Figure 5B Male Patients.
Figure 5 Perioperative opioid dosages expressed as mg equivalents of intravenous morphine sulpahte for opioid naïve (ON) and tolerant (OT) patients in the preoperative (Preop), intraoperative, PACU discharge and at 24 hours post sciatic nerve blockade characterized by nerve stimulator (NS) and ultrasound (US) guidance technique and level of practitioner training as either resident trainee (R) or nurse anesthetist (CRNA).
This study was limited in that not every SNB performed by the practitioner was assessed and therefore patient selection bias prevents generalizations concerning clinical proficiency and regional anesthesia expertise with respect to successful nerve blockade. The small numbers of patients within the chronic opioid usage subgroups for each practitioner group lead to inferences that this criterion might impact clinical outcomes. Use of the continuous visual analog scale (VAS) rather than selection of the pain score would have allowed more precise assessment of analgesia as compared to the discrete 10 point system. Using pain as a subjective clinical variable to objectively quantify a procedure outcome is challenging due to the many patient factors that contribute to its perception. This study demonstrates this phenomenon with cohorts with lower average pain scores having greater opioid requirements than groups with higher scores both in the preoperative and postoperative phases of their surgery.
There is no overall direct relation between level of academic background in anesthesiology and improved pain scores but there was observed improvement with the transition from NS to US guided SNB in all groups. Chronic preoperative opioid use by patients remains a challenge and influences the desired clinical outcome of successful SNB. Adequate analgesia is an important parameter for assessment of proficiency in RA techniques and should be included in practitioner procedure logs. Future studies need to address the limitations of this study which include using the VAS continuum instead of the discrete pain score and continuous recording of analgesic outcomes for all RA procedures instead of sporadic periodic observations of performance which can lead to inaccuracies for assessment of RA technical expertise. The authors report no external funding source for this study and also report no declarations of interest.
None.
None.

©2015 Lollo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.