Journal of
eISSN: 2373-6437


Review Article Volume 16 Issue 6
1Anesthesiology and Resuscitation, Ramón y Cajal University Hospital, Spain
2Anesthesiology and Resuscitation, Medical Lieutenant Colonel, “Gómez Ulla” Central Defense Hospital, Spain
Correspondence: Ildefonso Ingelmo Ingelmo, Anesthesiology and Resuscitation, Ramón y Cajal University Hospital, Spain
Received: November 07, 2024 | Published: November 19, 2024
Citation: Ildefonso II, Ricardo NS. Biophysics and physiopathogenesis of blast wave traumatic injury. Narrative review Part II.. J Anesth Crit Care Open Access. 2024;16(6):159-166. DOI: 10.15406/jaccoa.2024.16.00608
The harmful effect of chemical explosions on living beings and the destructive effect on nature are encompassed by the generic term of traumatic injury caused by blast waves. Nowadays, blast injuries are not exclusive to the military field, since in the civilian environment both accidental explosions (domestic and industrial) and intentional explosions (urban terrorism and asymmetric and/or hybrid warfare) have increased considerably. Blast injuries include both physical and psychological trauma. The pathophysiology of tissue damage caused by the blast wave is different from that of conventional civilian trauma (precipitation, traffic accidents, and others).
The blast wave produces a multimodal injury (different etiological factors) and multidimensional (several organs affected at the same time); in addition to causing a multitude of injuries in a short period of time, which saturate the health care services; hence it is considered a mass casualty incident. The pathophysiology of blast injuries is the subject of this narrative review.
Keywords: Explosive agents, Blast wave, Blast injuries, Taxonomy of blast injuries, Mass casualties.
... The blast wave is a shot without a bullet, a slash without a sword. Theodor Benzinger 1950.1 The shock wave is a shot without a bullet, a slash without a sword. It is present everywhere within its radius of action or range. It is its invisibility and ubiquity that contributes to the mystery of blast injuries and their perceived uniqueness.2 The zenith of which is post-explosion post-traumatic stress disorder (shell shock).3 Gunpowder originated in the 9th century by Chinese alchemists. Gunpowder was invented in China in the 9th century. The earliest literary reference to explosions is the description of the effects of black powder in the 14th century.4 The first medical description of the blast wave per dates back to 1915, during the Balkan war. The Swiss physician Franchino Rusca observed many dead without apparent injuries. These were casualties exposed to heavy explosions but without serious external injuries, and the deaths were attributed to massive lung damage from the blast wave.5
Explosive devices produce a "blast" wave; it is wrong to speak of a "blast" wave. This manuscript uses the Anglo-Saxon term "blast wave", which is comparable to "shock wave" in both military and civilian jargon. Only the explosion by chemical explosives is addressed; not the nuclear explosion, which requires specific considerations. It should be mentioned that blast wave (BW) injuries are not limited to the war context; as the civilian population is also exposed to BW injuries from terrorist attacks or from accidents related to: industry, home, aviation, nature and others.6-8 BW trauma should not be considered an entity of exclusive management by the military physician, on the contrary, every civilian physician should know the patterns and mechanisms of injury associated with the BW and even more, blast wave trauma should be a problem for all humans.2 The worldwide prevalence of blast injuries has increased over the last decade. Currently, blast injury is of great relevance, as explosives cause 66 to 84% of combat injuries according to figures from the conflicts in Iraq and Afghanistan and others in the civilian arena9-11 and many others in the civilian sphere. Other notable events include: New York 2001, Madrid 2004,12 Boston 2013, Brussels 2016 and Beirut 2020.13 Terrorist attacks worldwide over the past decade have tripled from approximately 5,000 in 2007 to more than 16,000 in 201714 and injuries related to these acts have increased eightfold.15,16
The BW produced after the detonation of an explosive agent causes serious damage to both people and material structures. In humans, BW injuries include both physical trauma and moral, psychosocial and psychological damage.17 as well as moral, psychosocial and psychological damage.18 The generic term BW injury applies to a set of injuries that are often severe, multiple and complex, both in anatomical location, type of injury (closed/open) and etiopathogenesis (pressure, thermal, chemical, biological); hence the concept of multimodal (barotrauma, ballistic, thermal, toxindromes, neuropsychological and others) and multidimensional (multiorgan injury) injury pattern, thus requiring interdisciplinary management to ensure proper management of BW injuries.19 to ensure appropriate management of the injured.8,9,17,20 The multiple and different injuries of the victims challenge triage, diagnosis, decision making and treatment.21
Initially, any victim exposed to a detonation, even if apparently uninjured (concealed injury concept), will be treated as a casualty with multiple potential injuries. The presence of sentinel symptoms/injury at triage should consider overlapping injuries towards speculative sentinel diagnoses. Even when bodily injuries are mild, the systemic effects of the shock wave amplify the original organ damage and influence its severity and outcome. The acronym "BBBB" stands for "blessée, blasted, burned and brained", i.e. an wounded, burst, scorched and concussion human, which easily illustrates the potential risks to which humans are exposed following a detonation.22
Pathophysiology of blast wave injuries
Following the open-air explosion, a BW is formed as a result of rapid chemical conversion of a solid or liquid to highly pressurized, hot gases, which rapidly expand and compress the surrounding air. The BW propagates quasi-circularly to the epicentre in all directions, causing multiple injuries to people and destructive effects on the environment. The components of the BW are the shock wave and the wind wave, not to mention other effects caused by the explosive: thermal, sonic and seismic, as well as toxindromes and inflammatory response. BW lesions were described by Schardin H23 and by Benzinger T1 in 1950 as the anatomical and physiological changes produced by shock wave-human body interaction. Upon impact of the shock wave (SW) on the body surface, a fraction is reflected / diffracted, another is absorbed, and the remainder propagates through the body as a pressure wave transmitted by the tissues, which are injured by pressure oscillations.24 The SW, i.e. barotrauma, is the cause of most closed injuries. The pathophysiology of tissue damage caused by SW, both by its positive phase of hyperpressure and its negative phase of hypopressure, is somewhat uncertain. The most frequent mechanisms described by several authors13,22,24-28 are: a) spallation, b) implosion, and c) shearing. A fourth mechanism, irreversible work, is suggested in the respiratory system. However, the exact degree to which these factors actually cause (closed) tissue damage is not fully known.15
The four mechanisms in their physical phase have the following considerations: The oldest described is scaling or defragmentation or splintering or spallation. The SW on impact with the body and passing through tissues of different densities causes tissue disruption, as the magnitude of the total wave (direct and reflected) exceeds the tensile strength of the tissue, so the interface separating them breaks towards the less dense medium, resulting in crack formation, microfragmentation and spalling (splintering, flaking, slabbing) on the tissue surface. The damage is microscopic rather than visible lacerations.28 In addition, the hyperpressure component of the SW passing through the different layers of the body tissue generates pressure differences, resulting in "molecular" disruption. On the other hand the negative pressure component of the SW, i.e. a drop below the local (vapour) pressure, causes the formation of "microbubbles" from the dissolved gas, which travel to areas of higher pressure where they coalesce and explode (cavitation effect), further increasing tissue spalling. Cavitation and tissue spalling are common at the tissue/gas and fluid/gas interface respectively, causing severe microvascular damage and tissue defragmentation.29 On the other hand, they are different and sometimes non-concurrent phenomena.30 Typical examples are: water splash in underwater detonation or when throwing a stone into the water, joint cracking or cavitation, anti-tank combat weapons and deterioration of reinforced concrete ("crocodile skin" cracks, spalling and falling out). Spalling occurs when the pressure SW passes from a denser medium to a less dense medium. Typical effect of spalling on the intestine2 and lung13 are: from the intestinal wall into the gas-filled intestinal lumen causing wall hematoma and/or haemorrhage; from the pulmonary capillary into the air-filled alveolus causing alveolar haemorrhage, respectively.
On the other hand, the phenomena of cavitation and boiling should not be confused, as they are different. Boiling bubbles arise from higher pressure (liquid phase) to lower pressure (air phase); cavitation bubbles arise in internal zones of low pressure (suction effect: "vacuum aspirations") to gather in external zones of higher pressure and break up. Spallation at the water-gas interface is defined as the displacement and fragmentation of the denser medium into the less dense one.31 In the mechanism of implosion, Boyle's Law stands out: at constant temperature, the volume of the gas is inversely proportional to its pressure. Therefore, when the gaseous content inside the tissues is compressed, the volume of the SW decreases, and if the pressure is very high, the cavity bursts "inwards". However, to explain visceral rupture, the action-reaction effect is added, i.e., as the hyperpressure phase of the SW passes, the gas re-expands and the cavity bursts "outward" with the release of high kinetic energy. Implosion is a "compression-expansion" mechanism (Figure 1) that affects the gases confined in the body (middle ear, sinuses, lung and intestine).32 Implosion in gas-containing structures is the result of the displacement of the less dense medium into the denser one. Air emboli traveling into the pulmonary circulation are an example of the implosion effect in the lung and the main factor in acute arterial air embolism.31 Implosion also causes compression of other tissues that would not otherwise be compressible (e.g. solid organs), resulting in both internal and external tissue tearing.2
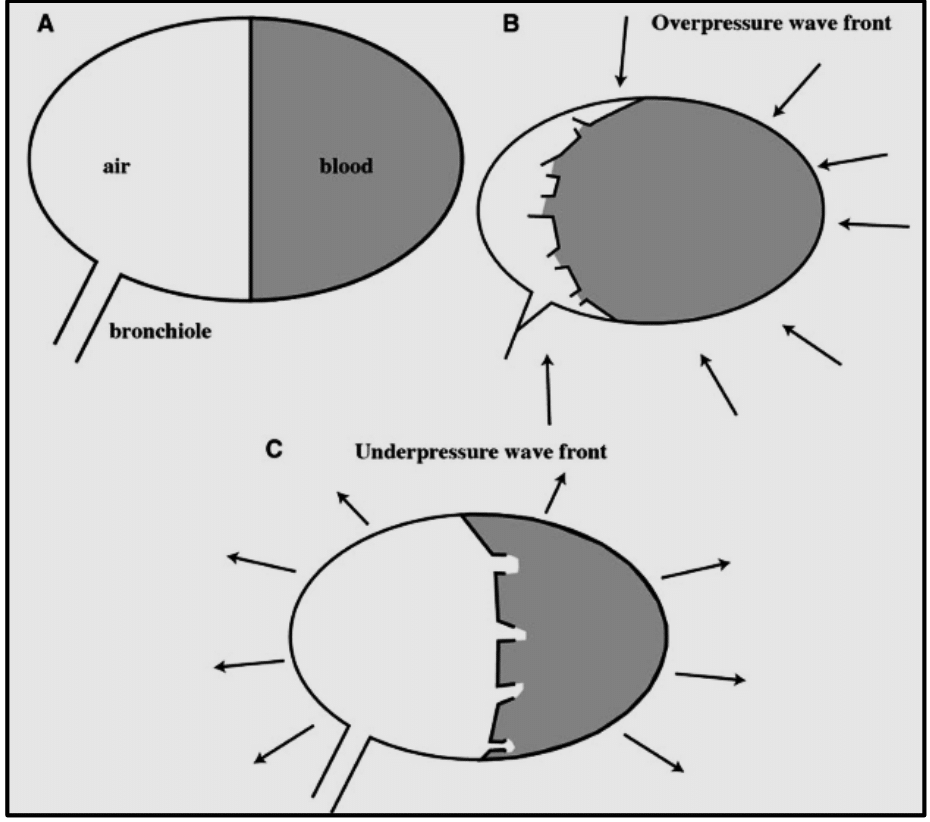
Figure 1 A simple conceptual model of primary pulmonary blast injury. Source, modified from: Ho AM. Med Hypotheses. 2002 59:611–613.
Injuries attributed to shear stress or shear forces are due to the fact that SW, when penetrating body organs: a) travels through tissues of different densities, causing microscopic disruptive effects rather than visible lacerations, at tissue interfaces, and b) at different velocities (acceleration/deceleration effect).2 In the abdomen, for example, it causes tearing of delicate junctions, such as the junctions of the intestinal mesentery and those of solid organs at the junctions of their capsules, as well as visceral tears secondary to the uneven movement of the abdominal wall and viscera.13,33,34
More controversial is the suggested mechanism for lung blast, known as irreversible work, which expresses the energy expended by the SW in deforming the thoraco-pulmonary unit to overcome the tensile strength forces of the tissue and injure it. The illustration often used is that of an aluminium can that is slightly dented and pushed back to shape. When the can is dented beyond its tensile strength, it can no longer be restored to its original shape and eventually cracks.35 For some authors36,37 the most likely mechanism of primary thoraco-pulmonary blast injury (barotrauma), which fits current modelling techniques, is the irreversible work effect related to differences in tissue tensile strength and shock wave velocity across different tissue phases.38 At the thoraco-pulmonary level, the onset of damage occurs when the hyperpressure SW compresses the tissues and they attempt to re-expand, so that the resulting forces exceed the tissue tensile strength and cause thoracic ecchymosis (parallel to the intercostal spaces), peribronchial / perivascular disruption, microhemorrhages, and pulmonary contusive foci.39
Regarding the frequency (Hz) component of the SW, it is suggested that the high amplitude and low frequency (<0,5 kHz), affects tissues with different speed of motion (spallation/shear effect), e.g. muscle-bone, grey-white matter; whereas low amplitude and high frequency (0,5-1,5 kHz) mainly target organs containing abrupt density changes from one medium to another (spallation/implosion effect), e.g. air-blood interface in the alveolar-capillary unit of the lungs or air-intestinal wall.24 In addition to the physical effect, the SW has a chemical effect, causing the breakdown of some protein molecules (l-arginine) and producing toxic elements (hydrogen peroxide and other free radicals), which would explain the systemic inflammatory response syndrome (SIRS), i.e. the inflammatory response to the primary blast observed in survivors after an explosion (e.g. pentrite).40
Aetiopathogenesis of blast injury syndrome
The physical theories of acoustic waves apply to the propagation of BW in body tissues. When a pressure wave encounters a surface with a different interface, some of the energy is reflected by the first interface and some passes through the first interface and propagates through the second interface. The ratio between reflected and transmitted energy depends on the acoustic impedance of the material (solid, liquid or gas). The pathophysiology of blunt blast trauma is controversial. Like any elastic wave, the shock wave is composed of: a) stress wave, or compression wave or P-wave, and b) shear wave or S-wave.29 Stress waves are longitudinal pressure forces and the motion of the particles is in the direction of propagation. Shear waves are transverse and particle motion is perpendicular to the direction of propagation (Figure 2). The stress wave propagates in the tissues at supersonic speed (80 - 90 m/s), has a high brisance power and causes weak tissue displacement. Its propagation is perpendicular to the interface, i.e. from the wall to the depth, and is reflected back when encountering stiffer structures, which determines the amplification of its injurious effect at the angles of reflection (e.g.: rib cage). The stress wave is the cause of tissue damage by spallation and implosion.31
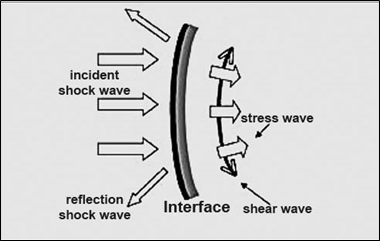
Figure 2 Body propagation of the shock wave. Source (modification): Debien B, Leclerc T, Clapson P, Perez JP, Lenoir B, Pats B. Explosion injuries. MAPAR (Mise Au Point Anesthésie Réanimation). 2006: 537-55.
Shear waves are shear or tear waves due to hyper- and hypo-pressure phenomena, equivalent to acceleration-deceleration forces. Their speed is weaker (20 to 25 m/s), but the tissue displacement they cause is more important, perpendicular to the stress waves, i.e. parallel to the interface. These waves cause distortions with asynchronisms of movement in adjacent structures, interruption of their junctions, stretching of mesos and vascular pedicles, and collisions between viscera. The distortions depend on the maximum amplitude of organ displacement and the time for that displacement (which is a function of weight). These effects are the cause of tissue defragmentation and haemorrhagic vascular tearing.29,41,42 The human body, which is deformable, resists SW better than surrounding structures. The unprotected human being can survive an explosion with a maximum hyperpressure of 30 Psi (206 kPa), but buildings and other structures collapse with an overpressure of only a few Psi. This means that people can survive the effects of the explosion and only be injured by the collapse of the buildings.22 Not only the destructive (physical / chemical) effect of the SW has to be considered, but also its therapeutic (biological) effect. Perhaps the most relevant is the fragmentation of calculi (urological, pancreatic, salivary) by extracorporeal lithotripsy. The mechanism of stone fragmentation by the lithotripter is by means of the hyperpressive stress wave that acts on the: a) anterior surface of the stone (fissures: spallation and cavitation), b) middle or inner part (reverberating stress waves), and c) posterior surface of the stone (spallation: flaking).43 At the systemic level, the benefits are multiple (neoangiogenesis, mitogenesis/morphogenesis, analgesic/anti-inflammatory/scavenger effect, in chronic processes, etc.); hence its use in recuperative physiotherapy and dermatology.
Taxonomic classification of blast injury syndrome (blast injury)
Up to five factors have been described15,33,44,45 up to five factors by which BW causes diverse and severe tissue damage in humans. Conventionally, the injuries are attributed to the type of blast causing46,47 and according to the taxonomy of injury described in U.S. Department of Defense (DoD) Directive 6025.21E6 is classified as primary, secondary, tertiary, quaternary, and quinary (Table 1).48
|
Category |
Mechanism |
Typical injuries |
|
Primary |
Impact of the shock wave with its two components (stress wave and shear wave) on the body. Preferentially affects hollow or gas-filled structures (ear, lung, digestive system, bone sinuses) without ruling out solids (brain). |
Barotrauma. Lung (lung burst). Ear (tympanic rupture and damage to the middle ear. Abdomen (abdominal haemorrhage and intestinal perforation). Rupture of the eyeball. Closed neurotrauma (concussion, post-traumatic stress disorder). |
|
Secondary |
Effect of primary fragments (shrapnel- shrapnel injury- pieces of casing, and/or secondary: additional contents (nails, screws, etc.) accelerated and thrown by the shock wave on the body (ballistic trauma). |
Open body injuries. Penetrating / perforating wounds (cavitational effect). Traumatic amputation of limbs. Lacerations. Rifling. |
|
Tertiary |
Effect of the wind wave propelling the body over hard surfaces, injuries due to the impact of fragments of "flying" materials (flying missiles) and/or the crumbly/collapse of material structures. |
Closed > open body injuries. Closed > open neurotrauma. Thoracic contusion. Avulsion of extremities. Tearing of soft tissues. Skin stains with explosive residue. Entrapment (mechanical asphyxia), Crush syndrome. |
|
Quaternary |
Other injuries not attributable to primary, secondary or tertiary mechanism. It also includes exacerbation or complications of pre-existing diseases. |
Flame or flash burns. Inhalation of dust (asbestos), steam, smoke (CO) or toxic or hot gas, Toxidromes from fuel, metals, etc. |
|
Quinaria |
Controversial blast mechanism. Body absorption of contaminants Abnormal tissue reaction to metals or fuel oils |
Immediate hyperinflammatory state |
Table 1 Taxonomy of blast injury
Source Bryden DW, Tilghman JI, Hinds SR, (2019) Blast-Related Traumatic Brain Injury: Current Concepts and Research Considerations. J Exp Neurosci 13:1179069519872213 https://doi.org/10.1177/1179069519872213
Source MSD Manual. 2021 Merch & Co. Kenilworth, NJ., USA https://www.msdmanuals.com/es-es/professional/lesiones-y-envenenamientos/armas-que-provocan-v%C3%ADctimas-en-masa/lesiones-por-explosivos-y-onda-expansiva
Source Hazell GA, Pearce AP, Hepper AE, Bull AMJ (2022) Injury scoring systems for blast injuries: a narrative review. Br J Anaesth 128:e127-e34 https://doi.org/10.1016/j.bja.2021.10.007
Source Franke A, Bieler D, Friemert B, Schwab R, Kollig E, Gusgen C. The First Aid and Hospital Treatment of Gunshot and Blast Injuries. Dtsch Arztebl Int. 2017;114(14):237-43. https://doi.org/10.3238/arztebl.2017.0237
I.- Primary blast: Primary blast injuries are attributed to the direct effect of the stress wave (P-wave), i.e. the hyperpressure component of the SW, on the subject's body. Therefore, in any Friedlander wave propagation medium the mechanism of injury is barotrauma. However, in the closed environment, in water and in solids there is no negative phase, only a P-wave of higher amplitude (peak) and duration (ms) due to reverberation (reflection/refraction/diffraction) of the wave, which causes more severe injuries than the blast in open air. The primary blast injury (blast injury itself) is predominant in the epicentre of the explosion, which causes lethal closed injuries and defines the generalized blast49,50 characterized by quasi-existence of external body injuries but with involvement of multiple internal organs (generalized capillary haemorrhages, especially thoracic-abdominal, avulsion of viscera, laceration of large vessels, air and fat embolisms, presence of carboxyhaemoglobin and foreign bodies). Tattooing is also frequent in the areas of the body exposed to the focus of the explosion. In areas close to the epicentre, the most striking are the frequent lethal open injuries, with quasi-total disruption / disintegration of the body (impalement, dismemberment, decapitation, scattering of visceral remains and panniers), i.e. anatomical damage that is not usually survivable, since even traumatic amputation is considered a marker of critical primary blast injury, since 50% of patients will die despite aggressive therapy.29
II.- Secondary blast: In addition to barotrauma, the energy of the SW causes a "ballistic effect", i.e., injuries by primary projectiles [pieces of the casing: shrapnel] and/or secondary projectiles [additional contents of the explosive device: nails, pellets, pellets, nuts, scrap metal, bolts, etc.)], accelerated and propelled at a distance by said wave; therefore, it is considered a "ballistic trauma" injury.
Secondary blast is the most frequent cause of lethal open (penetrating/piercing) injuries in victims. These types of injuries are contaminated; therefore, they generate a high risk of infection and septicaemia. In survivors, it is typical to mention the triad of hematomas, abrasions and punctate dermal lacerations (riddling, souffle criblages), due to the violent impact of multiple small fragments (shrapnel and others) on the victim's skin. The fragments may leave areas of pigmentation on the skin and tattooing due to residues of the explosive product. The recording of these injuries facilitates the determination of the location and relative position of the victims.
Eventually there may be bone fragments from surrounding victims, leading to the transmission of infectious diseases (hepatitis, HIV, etc.).
III.- Tertiary blast: The injuries it causes are attributed to the effect of the BW due to: a) body propulsion against the ground or rigid surfaces (impact trauma), b) collapse of built structures (burial) and c) fragments of structures (splinters, pebbles, and others) flying and accelerated by both the BW and the gravity effect (flying missiles). In addition, in this phase, air displacement (positive pressure) occurs to form a vacuum, which is followed by negative pressure (subsonic) to normalize the pressures and fill the vacuum.15
There is controversy about including injuries caused by "flying" fragments in tertiary blast; so that for some authors50 all injuries caused by the "fragmentation effect", i.e. "shrapnel" injuries, are attributed to secondary blast in high potency explosives (HPE) and to tertiary blast in low potency explosives (LPE) due to the minimal presence of SW.
Tertiary blast, also known as "wind blast", is the cause of both open and closed injuries to victims. Open (penetrating/piercing) injuries due to the effect of flying fragments can cause lacerating, puncture or cutting wounds; tearing of soft tissues (degloving injuries), impalement and deep wounds with severe haemorrhage. They are very contaminated wounds and even by facultative anaerobes. Closed injuries are due to: i) body propulsion, which by the action-reaction effect causes closed trauma (cranial, thoracic, abdominal); contusions, fractures and lacerations of solid viscera or the aorta, and ii) collapse of the structures [entrapment injuries, entrapment without extrication and traumatic asphyxia, as well as crush syndrome and compartment syndrome].
IV.- Quaternary blast: They are a group of miscellaneous injuries induced by heat (radiant and convective) and/or by toxics, since the explosion can be a vector of chemical and biological warfare agents. They are produced: a) thermal burns, of the flash or flame type: by combustion (incendiary bomb: napalm), or by incandescent particles (flakes) (e.g. white phosphorus bomb); b) mucosal lesions of the oropharynx and upper airway by inhalation of toxic and superheated gases/vapours and c) skin lesions by contact with chemical irritants (residues of the explosive, elements of its decomposition or additives).
Flash burns, depending on their location, allow us to determine the position of the victim. With regard to toxic asphyxia, there are frequent injuries due to inhalation of: CO, cyanide, and fumigants, as well as inhalation of dust containing asbestos or coal, and of toxic vapours/gases such as Hg, Cl, nitrous, P, and other vapour toxin syndromes.51 which aggravate a concomitant lung blast. Another route of entry is dermal absorption, e.g. P intoxication ("white death") when penetrating the organism after burns by the incandescent flakes of the white phosphorus bomb. Other authors6,22,27,51 also include exacerbation or complications of pre-existing medical conditions and psychological-psychiatric dysfunctions: shell shock, post-traumatic stress disorder (PTSD), and other neuropathologies, e.g. sideration, dissociation, neurosis or suicide.
V.- Quinary/quintenary blast: This category is controversial since it is not usually due to BW per se. Currently, hyperinflammatory reaction without associated lesions that explain it is considered in this category. These patients manifest hyperpyrexia, diaphoresis, tachycardia, low central venous pressure, and excessive fluid demand to maintain adequate tissue perfusion.22 The clinical picture is considered to occur only with a certain type of explosive: PENT (Pentrite), which possesses the vasodilator properties of alcohols (pentaerythritol). In fact, it is used like nitroglycerin, for myocardial ischemia. The drug Lentonitrate is manufactured from pure Pent. The toxicity of pentrite is suggested to be due to skin absorption of the explosive after detonation.21 Likewise, the additives of the "dirty bombs" (radiation, metals and even bacteria or viruses) after dermal and/or mucosal (oral, respiratory, ocular) adsorption / absorption could provoke such a response by affecting the immune system and perhaps the autonomic nervous system, leading to an immediate hyperinflammatory state.15,33,52
Other considerations of blast wave syndrome
The pattern of BW injuries can vary significantly in both military and civilian settings. Military explosions predominate in open spaces. Casualties are young, healthy soldiers, and dressed in personal protective equipment (helmet, vest, coveralls, etc.) resulting in lower rates of thoracic and abdominal injuries compared to previous conflicts. In contrast, civilian explosions are usually in confined or semi-confined sites, which increase the damage and number of injuries. Casualties range from children to the elderly. The co-morbidity of the injured complicates the clinical evolution. The absence of personal protective equipment increases the number of open chest and abdomen injuries.31 From the epidemiological point of view, immediate mortality is high due to lethal injuries in the epicentre and critical injuries in the secondary perimeter (Figure 3). In the surviving victims, morbimortality is high, both because of the multilesive pattern of the injured and because of the multiple simultaneous victims (mass casualty incident) that collapse health care (overcrowding). In health centres, the order of arrival of victims is "backwards": the most seriously injured arrive after the less seriously injured, who bypass the triage of the emergency medical services and go directly to the nearest hospitals.
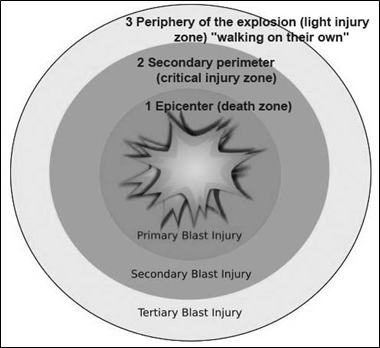
Figure 3 Blast wave zones and types of blast injury.
Source, modified from: https://www.wikimedia.org/ (Anatomy of a blast.sgv)
On the other hand, mortality does not follow the typical three-phase pattern of conventional civilian polytrauma (immediate, early and late), on the contrary, a biphasic pattern is observed, with a more or less high number of immediate mortality, and a relatively low number of early or late mortality.53,54 The anatomical injuries caused by BW have a different pathophysiological pattern than those caused by civilian trauma (fall from height, traffic accident, sports and others) (Figure 4). The cause is multimodal and the pattern multidimensional. Primary injuries result from direct passage of SW through the body ("blast injuries per se") in which "some is transmitted, some is absorbed and some is reflected/diffracted/refracted". The impedance of each tissue determines the amount absorbed from each part and the injury threshold (an overpressure of 414–552 kPa or 60–80 psi is considered potentially lethal).
According to the category of blast injury, it is suggested that closed (blunt) injuries are mainly from primary blast (barotrauma from SW), not forgetting body propulsion and collapse of structures (crushing, entrapment) from tertiary blast.33,55 It has been considered that the primary blast only affected heterogeneous (hollow) organs, i.e. air-filled structures (ear, larynx, lung, digestive tract, sinuses) or with liquid-gas interface (intestinal wall, blood vessels); however, there is now no doubt that SW barotrauma also injures homogeneous (solid) organs. The greatest energy transfer occurs at points where tissue density changes, hence energy transfer at a bone/tissue-soft tissue interface can partially amputate limbs. The effects are more manifest with HPEs than with LPEs, because the latter do not generate SW. Regarding the open injuries (penetrating/piercing) of the HPEs, secondary blast is predominant due to the "shrapnel" effect, followed by tertiary blast due to "ballistic" (flying missiles), while those of the LPEs, since they do not present SW, are due to wind wave (WV), i.e., body propulsion and ballistics.22,54 In aerial blast, the injury profile is related to the distance. When it is very short, less than 3 meters, most injuries are critical, even with very small explosive charges. At distances greater than 15 meters, injuries are usually minor, even with charges of more than 40 kg of conventional explosive (TNT). The epicentre is considered a lethal zone; in contrast, in the critical zone the immediate threat to life is usually injury by multiple fragments (Figure 5) affecting multiple anatomical sites.28,56 However, in reality, the effects of SW and WW are synergistic (combined or additive), i.e. the injuries are caused by the conjunction of different types of blast (e.g. traumatic amputation); hence, the BW syndrome is a multidimensional/multifaceted (blast-plus injury) injury, 24 both in terms of topography (multiorgan and polycompartimental) and mechanism (barotrauma, ballistic, thermal, toxin syndromes, and others), single or combined (Figure 6). Hence, it is a challenge to classify the lesion in the category of the blast cause.42,57,58 Therefore, some authors define the concept of "effective pressure" as the primary factor of injury, as they consider that it is the overpressure phase of both SW and WW that is responsible for BW damage. Thus, if an individual stands next to a wall they will receive both incident and reflected/diffracted overpressure, and in this case they will all form the effective pressure.34 Due to the complexity of categorizing BW injuries, other authors propose a bipolar classification: primary injuries attributed to barotrauma (primary blast per se) and secondary injuries due to other factors (shrapnel, fragments, thermo-chemicals and others, i.e. secondary, tertiary and quaternary blast, respectively).44,50
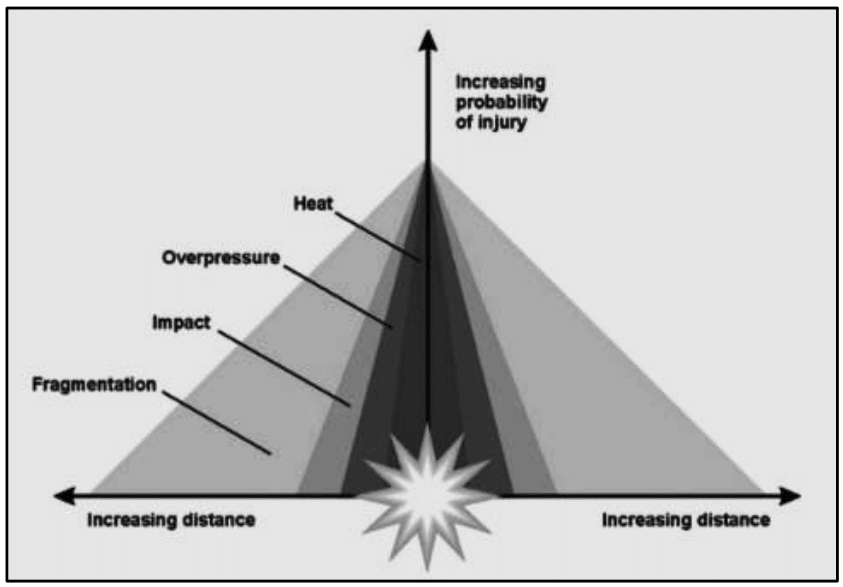
Figure 5 Probability of injury according to distance from the blast epicenter. Source, modified from: Emergency War Surgery: 5th edition United States Revision.
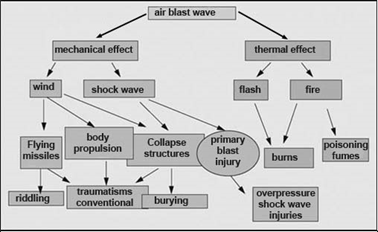
Figure 6 Effect of the shock wave in the airborne propagation medium.
Source modified from: Pats B, et als. 2000. EMC-Anest Reanim
In blast injury syndrome, the disproportion between the apparent scarcity of external injuries and the enormous internal destruction (viscera) is striking (Figure 7). It is important to bear in mind that survivors may suffer shock or hypoxemia in the absence of external signs of injury. In them, what attracts attention is the open trauma (penetrating / perforating) due to the "fragmentation and projectile" effect, but the closed one is trivialized with "hidden injury", which usually goes unnoticed initially, due to its mediated presentation; hence it requires diagnostic suspicion.46 Sentinel injuries (tympanic rupture, laryngotracheal petechiae, intercostal thoracic ecchymosis, hyphema, pale tongue, livedo reticularis) are subtle injuries that may increase the risk of having or developing severe BW injury. These patients with closed blast injury should be closely observed, no matter how well they are clinically. A valuable aid is the full-body computed tomography (CT) scan, which facilitates the diagnosis of closed trauma caused by BW, although in the blast belly it has certain limitations.58 It is known that the injuries produced by the BW show their severity in relation to: a) the characteristics of the explosive (HPE / LPE /, IEDs, quantity, brisance), c) the medium (air, water or solid), d) the place (open, closed) and the velocity of propagation; as well as the distance of the victim to the epicentre and individual factors. Personal factors include: a) the position of the individual with respect to the BW (standing/decubitus position, parallel/perpendicular to the BW), b) corpulence, c) the occurrence of SW reverberation, d) the presence of personal protective equipment (goggles, helmet, military vest/overalls, etc.), and e) individual resistance. It should be noted that personal protective equipment (bulletproof vest/overalls and helmets), although they prevent shrapnel and/or projectile injuries, do not protect against primary blast, and even aggravate the effects of SW. This "behind the armor" blunt trauma can be responsible for serious and disabling injuries.58

Figure 7 Wounded by blast wave in the Afghanistan War treated in the Spanish Military Hospital (photograph by the author -RNS-).
The effect of BW on the body (blast-body interaction) is general as well as local (regional).59 The response of the organism after a blast involves interlocking mechanisms of local, systemic and encephalic responses. Even when the regional tissue response is mild, systemic changes substantially modify the original organ damage and influence its severity and outcome. Air embolism/fat/thrombus, vascular mechanisms (hemodynamic, endothelial and smooth muscle cell), systemic inflammatory response syndrome and encephalic response [autonomic activation: (juxtacapillary J receptors, Bezold-Jarisch reflex, Takotsubo stress), neuroendocrinopathy, stunned neuron) are among the most important systemic alterations that modify the initial (local) blast wave injury.24,60 In addition, although most injuries are caused by explosive or incendiary devices, the possibility of secondary devices such as weapons of mass destruction (WMD: biological, chemical or nuclear) must always be considered, without forgetting victims as terrorists (second impact).
A chemical explosion produces a blast wave, formed by the shock wave and the wind wave, as well as other effects: hyperheated gases, thermal effects, seismic effects, and toxins, among others.
Explosive devices are classified into high power and low power.
Blast injuries are classified into four types according to the type of blast injury: primary, secondary, tertiary, quaternary and quinary.
Closed (blunt) injuries are mostly due to barotrauma (primary blast). The factors of closed injury are: spallation, cavitation, implosion, shearing and irreversible work.
Open injuries (penetrating/piercing) are secondary and/or tertiary blast injuries
The severity of the injuries depends on the distance of the victim from the focus of the blast. Three zones are considered: epicentre (lethal zone) where the primary blast acts, secondary perimeter (critical zone) where the secondary and tertiary blast acts and the periphery of the explosion (minor injuries).
The blast wave not only provokes a local/regional injury but also a general/systemic (inflammatory, endocrine and immune) response.
I. Ingelmo Ingelmo states that there is no conflict of interest.
R. Navarro Suay states that there is no conflict of interest
This narrative review paper does not contain any studies with human or animal participants conducted by any of the authors.
Informed consent for the use of photographs taken by the author R.N.S.

©2024 Ildefonso, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.