Journal of
eISSN: 2373-6437


Case Report Volume 16 Issue 5
1Department of Internal Medicine, Broward Health North, Pompano Beach, USA
2University of Missouri, Department of Anesthesiology, Columbia, USA
Correspondence: Ayman Oweisi, Department of Internal Medicine, Broward Health North, Pompano Beach, 3611 Turtle Run Blvd Apt 625, Coral Springs, FL, USA
Received: August 09, 2024 | Published: September 27, 2024
Citation: Oweisi A, Olson J, Cheney C. Anesthetic management of acute embolic stroke following Non-ST-Elevation Myocardial Infarction: a case report. J Anesth Crit Care Open Access. 2024;16(4):119‒120. DOI: 10.15406/jaccoa.2024.16.00602
The management of patients with severe coronary artery disease (CAD) and acute heart failure following myocardial infarction presents significant challenges. We report the case of a 66-year-old male who developed an acute embolic stroke, possibly due to a cardiogenic embolism, following coronary angiography and cardiac catheterization for a non-ST-elevation myocardial infarction (NSTEMI). The NSTEMI resulted in ischemic cardiomyopathy and left ventricular dysfunction. During an urgent thrombectomy under general anesthesia, the patient required careful propofol dosing to avoid exacerbating his new-onset heart failure. Vasoactive medications, including norepinephrine, epinephrine, phenylephrine, and dobutamine, were used to maintain hemodynamic stability and support myocardial contractility. A thorough understanding of cardiac perfusion dynamics was crucial for the successful anesthetic management of this complex case. This report highlights the importance of individualized anesthetic approaches and the judicious use of vasoactive agents in patients with severe CAD and acute heart failure.
Keywords: Coronary artery disease, heart failure, myocardial infarction, stroke, anesthesia, vasoactive medications, propofol, hemodynamic management
Management of patients with severe coronary artery disease (CAD) and acute heart failure presents significant clinical challenges. CAD is a leading cause of morbidity and mortality, often necessitating interventions such as cardiac catheterization. However, risks from these procedures include the potential for cardiogenic embolisms leading to a stroke.1 Complications from myocardial infarctions could include heart failure and ventricular dysfunction, further complicating patient care,2 as observed in our case of a 66 year old male. The use of medications such as norepinephrine, epinephrine, phenylephrine, and dobutamine are critical for reducing mortality by maintaining hemodynamic stability and supporting myocardial contractility.3 Additionally, the administration of anesthesia in patients with new-onset myocardial depression requires careful dosing of propofol in order to avoid exacerbating heart failure. Our case discusses the rationale behind the selection of vasoactive medications and the importance of safe anesthetic practices in managing patients with severe CAD and acute heart failure.
A 66-year-old male underwent coronary angiography and cardiac catheterization for an NSTEMI due to significant coronary insufficiency secondary to 70% LMCA stenosis, 99% LAD stenosis, and 90% distal RCA stenosis. The NSTEMI led to ischemic cardiomyopathy and left ventricular dysfunction with an ejection fraction of 0.25. While in his nursing unit, he developed right-sided weakness, difficulty speaking, and left gaze paresis, which was indicative of an acute embolic stroke to the left MCA possibly caused by a cardiogenic embolism following the cardiac catheterization.
We proceeded with an urgent thrombectomy in the operating room at 18:45. Given the patient's new onset heart failure, we were careful with the dosing of propofol, which is known for its myocardial depressant properties. The patient weighed 95kg and received a reduced induction dose of propofol at 1.1 mg/kg, totaling 100 mg administered in two 50 mg boluses. The first dose was given at 18:47 and the patient was monitored for any adverse reactions. After tolerating the first dose well, the second bolus of propofol was given at 18:48. We were cautious with our approach in order to minimize the risk of worsening his heart failure while ensuring proper sedation.4
Throughout the case, the patient was managed with total doses of 0.7mg norepinephrine, 9.0mcg epinephrine, 0.4mg phenylephrine, and 23mg dobutamine while using 1L of lactated ringer to maintain adequate blood pressure. Norepinephrine has mixed alpha-1 and beta activity and was used to increase systemic vascular resistance and support myocardial contractility, leading to an increase in blood pressure and cardiac output. Epinephrine has comparable activity on alpha-1 and beta receptors and was used to increase systemic vascular resistance, heart rate, cardiac output, and blood pressure which ultimately provided additional inotropic support. Phenylephrine is an alpha-1 agonist and was given to induce peripheral arterial vasoconstriction, providing improvement in vascular tone and enhancing perfusion pressure.5 During the case, the patient continued to be hypotensive with blood pressures dropping down to 100/40mmHg and dobutamine, a beta-1 agonist with positive inotropic effects, was introduced at 19:38 to enhance cardiac output by increasing myocardial contractility.5 The thrombectomy was completed uneventfully and tolerated well by the patient (Figure 1-3).
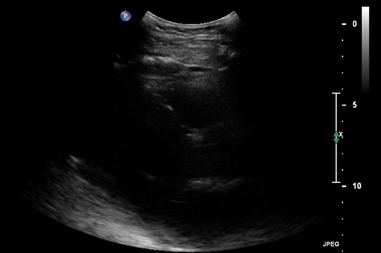
Figure 1 Transthoracic echocardiogram (TTE) in the parasternal long-axis view at end-systole. The image demonstrates a dilated left ventricle with reduced contractility and decreased ejection fraction, indicative of acute heart failure. The left atrium appears enlarged, suggesting elevated filling pressures.
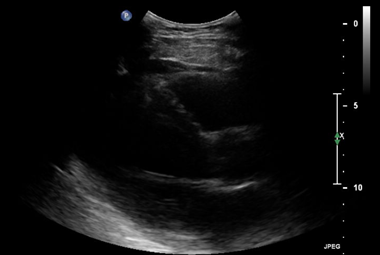
Figure 2 Transthoracic echocardiogram (TTE) in the parasternal long-axis view at end-diastole. The left ventricle is shown to be dilated with thinned walls during diastole. The reduced difference in ventricular size between end-systole (Figure 1) and end-diastole further illustrates the decreased ejection fraction and systolic dysfunction associated with acute heart failure.
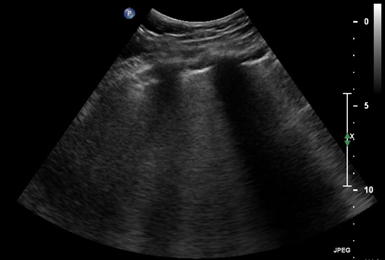
Figure 3 Lung ultrasound demonstrating the presence of multiple B-lines (vertical hyperechoic artifacts extending from the pleural line to the bottom of the screen). B-lines are a sign of increased extravascular lung water and pulmonary edema, which are common findings in patients with acute heart failure. The increased number and diffuse distribution of B-lines throughout the lung fields suggest a significant degree of pulmonary congestion secondary to the patient's cardiac dysfunction.
Administering anesthesia in patients with myocardial depression requires careful planning. Propofol can depress myocardial function further and worsen heart failure, requiring decreased dosing and close monitoring. The anesthetic management strategy in our case included the use of vasopressors to maintain hemodynamic stability and optimize cardiac perfusion. Right ventricular perfusion, as opposed to left ventricular perfusion, is performed throughout the entire cardiac cycle. Additionally, the right ventricle can maintain contractile function and energy stores during coronary hypoperfusion by downregulating its metabolic demand. These characteristics help maintain the oxygen supply-demand balance and provide resistance to ischemia. However, acute or chronic increases in right ventricular afterload can compromise these mechanisms, emphasizing the importance of carefully selecting vasoactive medications to avoid exacerbating right ventricular ischemia and ensuring adequate perfusion during anesthesia administration.6
Our case identifies the complexities of managing a patient with severe CAD, stroke, and heart failure following a NSTEMI. The use of several vasopressors, careful propofol dosing, and a thorough understanding of cardiac perfusion dynamics were crucial in the successful management of this patient. The choice of pressor medications was guided by their specific receptor affinities and physiological effects, ensuring optimal support for both vascular tone and myocardial contractility. Safely inducing anesthesia requires a careful approach, balancing the need for sedation and analgesia to maintain cardiovascular stability.
The authors report no relevant financial conflicts of interest for this manuscript.
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.

©2024 Oweisi, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.