Journal of
eISSN: 2373-6437


Case Report Volume 13 Issue 1
University of Foggia, Italy
Correspondence: Marco Paolo Perrini, University of Foggia, via don lino palmisano 27 Locorotondo BA, Italy ,, Tel 00393281671727
Received: February 02, 2021 | Published: February 12, 2021
Citation: Perrini MP. Acute neck pain after manipulations in a healthy adolescent patient: a case report. J Anesth Crit Care Open Access. 2021;13(1):30‒33. DOI: 10.15406/jaccoa.2021.13.00466
It is renowned that cervical spinal manipulation therapy (CSMT) is widely used among the people. It is frequently involved in the multi-disciplinary treatment approach for neck pain and stiffness. These kind of treatments are often offered by many medical institutions such as non-medical institutions. Although spinal manipulation is a simple and safe therapy compared to surgical or pharmacological treatments, the serious complications caused by neck manipulation cannot be ignored. These complications include vertebral artery dissection, spinal cord or root injury, phrenic nerve injury, cervical subluxation, and cerebrovascular accidents.1,2 Cervical epidural hematoma (CEH) is an uncommon entity that can arise spontaneously or due to CSMT, cervical dislocation fractures, coagulopathies, thrombocytopenia, hemophilia, and immune diseases such as ankylosing spondylitis and Paget disease.3,4 Few cases of severe quadriplegia caused by neck manipulation have been reported.5-15 Most of these cases suffered from various under-lying diseases, such as coagulation dysfunction and cervical vascular malformations. We report a case of acute CEH in a healthy adolescent male patient rapidly evolving to tetraplegia due to neck manipulations performed in the previous days. There are actually no reported cases on our knowledges of healthy adolescent patients in literature.
A 19-year-old healthy adolescent male presented to our ED in february 2020 with acute neck pain. He referred to periodically undergo cervical spine manipulations after a car accident occurred at the end of october 2019 with no reported traumatic injuries. On neurological examination he had no dysesthesia at the four extremities. Muscle power was scored as grade 5 over 5 in the upper extremities, grade 4 over 5 in the lower extremities. No deep tendon reflexes abnormalities in the extremities bilaterally. Babinski’s sign and Hoffmann’s signs were absent. Laboratory testing results were negligible.
Magnetic resonance imaging (MRI) with paramagnetic contrast agent of the cervical spine (Figure 1) revealed a C4-C6 extramedullary/epidural over fluid layer occluding the posteriors perimedullary spaces. The collection was characterised by inhomogeneous signal probably linked to the presence of haemoglobin degradation products, related to the subacute evolution phase. There was an evident compressive effect on the spinal cord without signal alterations. No vessels abnormalities were found with the technique. A computed tomographic (CT) scan (Figure 2) of the cervical spine didn’t reveal fractures or other collateral findings except for the hyperdensity expressed by the extramedullary fluid collection. We leant, at the beginning, for a conservative approach keeping the patient under observation in our neurosurgery department. Three days after, the patient suddenly developed dysesthesia at the four extremities and tetraplegia with a residual capacity of slight intra rotation of the upper limbs.
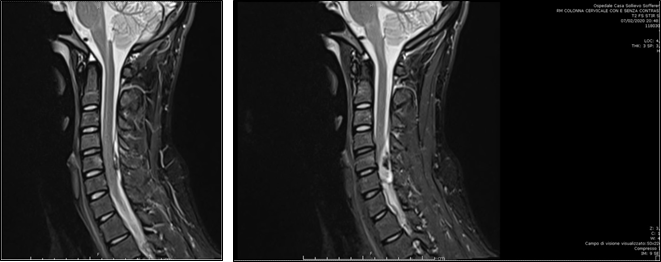
Figure 1 MRI with paramagnetic contrast agent of the sagittal cervical spine revealing a C4- C6 extramedullary/epidural over fluid layer occluding the posteriors perimedullary spaces.

Figure 2 Sagittal CT scan view of the cervical spine underlying the hyperdensity expressed by the extramedullary fluid collection in the absence of fractures.
A new MRI (Figure 3) in the sagittal T2 STIR sequence showed increased dimensions of the collection extending from C7 up to C2 with increased evidence of the previous compressive findings together with a new hyperintensity of the posterior cervical spinal tract linked to the medullary impairment. The patient underwent emergency C4 to C6 laminoplasty to evacuate this space-occupying hematoma. During the operation, an acute-subacute hematoma located in the posterior part of the spinal canal was isolated.
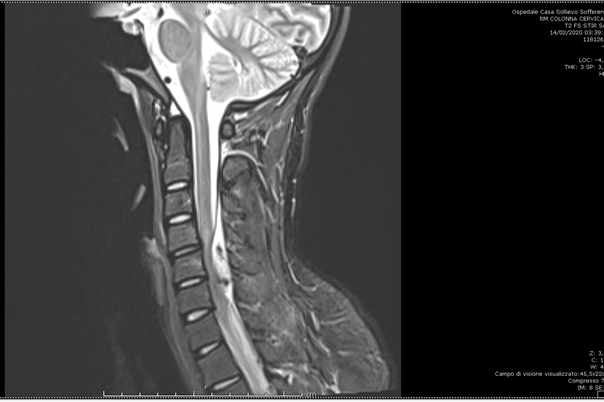
Figure 3 MRI in the sagittal T2 STIR sequence showing increased dimensions of the collection extending from C7 up to C2 with increased evidence of the previous compressive findings.
No vascular abnormalities were found intraoperatively.
The postoperative course was uneventful with a progressive complete recovery from the motor-sensitive deficits showed. We postoperatively performed an angiographic study, laboratory test for coagulopathies or linkable diseases without relevant results. Another MRI was performed one week after the operation emphasizing the resolution of the case (Figure 4).
Spinal epidural hematoma is a rare condition which may lead to serious complications.
CEH can arise spontaneously without an identifiable cause in 40% to 50% of reported cases or it can be caused by CSMT, cervical dislocation fractures, coagulopathies, thrombocytopenia, hemophilia, vascular malformations, neoplasm, pregnancy and immune diseases such as ankylosing spondylitis and Paget disease.3,4,7,11 Most traumatic SEH are associated with vertebral trauma, penetrating injuries, birth trauma, or iatrogenic injuries such as epidural steroid injection, lumbar puncture, and spinal surgery.5 Cervical spinal manipulation is a common practice,used for the treatment of neck pain and stiffness, which is performed by either professional or non-professional personnel.
It is defined as: “A passive, high velocity, low amplitude thrust applied to a joint complex within its anatomical limit with the intent to restore optimal motion, function, and/ or to reduce pain”.13
The incidence of complications has been estimated to be less than one injury for every 1 to 1.5 million adjustments,16 of course, there are the above mentioned factors which could expose the patient to a higher risk of bleeding complications. Other possible complications resulting from cervical spinal manipulation could include cerebral stroke from local pressure on the blood vessels, ligament injury or fractures from excessive pressure or rotation such as spinal cord injury. CEH after spinal manipulation has been reported very rarely and there are only few cases described in literature (Table 1). Before any manipulation an accurate physical examination and patient clinical history collection should always be performed.
|
Reference |
Age (years) |
Gender |
Symptoms |
Level |
Location of hematoma |
Treatment |
Outcome |
|
Segal et al.5 |
33 |
Female |
Paraplegia |
C4-6 |
posterior |
surgery |
|
|
Tseng et al.8 |
67 |
Female |
Hemiparesis |
C3-5 |
posterolateral |
surgery |
recovery |
|
Saxler G et al.6 |
27 |
Female |
Headache |
C1-S1 |
not reported |
conservative |
recovery |
|
Whedon et al.7 |
79 |
Male |
Lower extremity paralysis |
C2-4 |
posterolateral |
surgery |
recovery |
|
Domenicucci et al.10 |
52 |
Female |
Hemiparesis |
C4-T1 |
posterolateral |
surgery |
recovery |
|
Heiner et al.11 |
40 |
Male |
Upper extremity paralysis |
C4 |
posterolateral |
conservative |
recovery |
|
Huang et al.13 |
40 |
Male |
Upper extremity paralysis |
C2-T2 |
posterolateral |
Surgery |
recovery |
|
Fattahi et al.14 |
44 |
Female |
Tetraplegia |
C1-4 |
anterior |
Conservative |
recovery |
|
Ling et al.9 |
33 |
Male |
Tetraplegia |
C4-7 |
posterolateral |
Surgery |
die |
|
Ryu et al.12 |
38 |
Male |
Paraparesis |
C6-T1 |
anterior |
Conservative |
recovery |
|
Chen et al.15 |
55 |
Male |
Tetraplegia |
C3-T3 |
posterolateral |
Surgery |
partial recovery |
|
present case |
19 |
Male |
Tetraplegia |
C4-C6 |
posterior |
Surgery |
recovery |
Table 1 Summary of reported cases of cervical epidural hematoma after spinal manipulation therapy
The presence of any neurological deficit on physical examination could be the signal of a CEH and should be regarded as an indicator of the patient’s risk of getting severe complications during a cervical manipulation. A detailed and focused patient history collection should assess possible vasculogenic contribution, coagulopathies and conditions that might contraindicate the mobilization or manipulation. All reported CEH cases have generally occurred posteriorly or posterolaterally.5-15 The pathological mechanism of spinal epidural hematoma remains still unclear but the bleeding from the epidural vein plexus is the most widely accepted hypothesis for the mechanism of hematoma formation.17
The most probable association could be explained by the anatomical lack of valves in the epidural venous system. Any sudden rise in intrathoracic pressure, as it physiologically happens lifting a weight or coughing, may be transmitted directly to the epidural venous plexus thus causing bleeding and the formation of an epidural hematoma.18 The sudden increase in venous pressure induced by the pressure applied by the maneuvers could have led to bleeding from the epidural veins causing the formation of the hematoma in our patient. The clinical presentation of CEH is severe neck pain associated to the presence or absence of neurological compromission including sensory, motor, or autonomic dysfunction.
These symptoms can vary depending on the size and location of the hematoma, leading sometimes to an underestimation of the pathology in the absence of neurological deficits, anyway, almost all patients develop acute symptoms immediately after the manipulation.5,8 MRI is the gold standard imaging tool for early diagnosis of SEH. It allows to identify the lesion and its impact on the spinal cord collaterally evaluating other conditions such as herniated vertebral discs, acute bony compression, cord edema, cord contusion, and subarachnoid hemorrhage. The treatment for CEH depends on the severity of neurological symptoms.
Although conservative treatment has been proposed and described as a strategy to successfully treat patients with mild or no neurological symptoms, as we considered for our patient at the beginning, early surgical decompression is still the best choice of treatment for CEH. In a series of 30 patients who suffered from a spinal epidural hematoma Lawton et al. examined the relationship between surgical timing and neurological outcome. The average postoperative Frankel grade decreased from 4.7 to 3.7 in patients operated on in less than six hours versus after 24 hours, and there was a corresponding decrease in rate of complete recovery from 67% to 12%. Better outcomes were seen in patients operated on within 12 hours of symptom onset.19
Cervical laminectomy has been the most described surgical procedure for decompression of spinal cord in patients with CEH.5,7,8-10,13 However, standard laminectomy has also been reported to result in late cervical deformities such as kyphosis or segmental instability.20 Full recovery from all neurological deficits was reached by our patient some days after the emergency decompression surgery.
Neck pain is a common and recurrent symptom. In the absence of any neurological sign and symptom, rare pathologies such as CEH could be underestimate because there is no practical, clinically valid screening tests to identify underlying risks in patients with neck pain. SEH following CSMT is one of the possible, although rare, differential diagnosis to take in count in the patient history collection. Before any manipulation an accurate physical examination and patient clinical history collection should always be performed by the professional or non-professional personnel investigating for conditions that could predispose to various complications. Independently to the etiology, SEH causes severe compression of the cord, which can result in irreversible neurological deficits. The complete neurological recovery is strictly related to the time to surgical intervention. A high index of suspicion on history taking, early signs recognition, MRI evaluation and the right treatment option are crucial elements in the pathway for the best outcome.
Authors declare no conflict of interests for this article.

©2021 Perrini. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.