Journal of
eISSN: 2373-6437


Case Report Volume 6 Issue 3
1Resident Physician, Department of Anesthesiology, Loma Linda University School of Medicine, Loma Linda, USA
2Assistant Professor of Anesthesiology, Department of Anesthesiology, Loma Linda University School of Medicine, USA
3Assistant Professor of Radiology, Department of Radiology, Loma Linda University School of Medicine, USA
4Professor and Chair, Department of Anesthesiology and Pain Medicine, University of California Davis School of Medicine, USA
Correspondence: Michelle Y Woodfin, Department Anesthesiology, Institution Loma Linda University School of Medicine, Mailing address Room 2532 LLUMC, 11234 Anderson Street, Loma Linda, CA, USA 92354, Tel 1-909-558-4475, Fax 1-909-558-4143
Received: November 15, 2016 | Published: December 9, 2016
Citation: Cluff M, Woodfin MY, McCluskey EA, Harder SL, Applegate RL (2016) Accidental Dural Puncture and Subsequent Intrathecal Catheter Placement for Labor Analgesia leads to Cranial Nerve VI Palsy. J Anesth Crit Care Open Access 6(3): 00232. DOI: DOI: 10.15406/jaccoa.2016.06.00232
Accidental dural puncture during epidural placement for labor analgesia is a relatively common complication occurring in roughly 1.5% of all epidurals. There are many possible sequelae of accidental dural puncture, ranging from benign to serious. We present a case in which an accidental dural puncture during labor epidural placement led to headache and prolonged unilateral abducens nerve palsy. We discuss our management of these complications and encourage close follow up from anesthesia providers of patients who experience accidental dural puncture to ensure no significant complications remain untreated.
Keywords: accidental dural puncture; post dural puncture headache; cranial nerve VI Palsy; epidural blood patch
Epidural catheter placement is commonly used to provide analgesia for labor and anesthesia for cesarean delivery. Accidental dural puncture is a known complication of epidural catheter placement. The incidence of accidental dural puncture varies based on practitioner experience, volume performed at an institution, and other factors. Meta-analyses show the incidence of accidental dural puncture to be approximately 1.5%, but some studies report rates as high as 7%.1,2 The most common complication following accidental dural puncture is post dural puncture headache, although other complications are known. In this case report we discuss an accidental dural puncture that resulted in a rare but extremely severe complication, unilateral cranial nerve VI palsy. The patient reviewed the case report and gave written permission for the authors to publish the report.
A 32-year-old G2P0010 female was admitted to our facility for induction of labor at 40 weeks and 2 days with fetal macrosomia. The patient had an otherwise unremarkable medical history. Induction of labor using an appropriately timed sequence of misoprostol and dinoprostone, followed by augmentation with oxytocin was done. Labor failed to progress initially but eventually membranes were ruptured. With continued labor, she requested an epidural catheter for pain management. Epidural catheter placement was moderately difficult requiring two attempts. The epidural space was identified using the loss of resistance technique with air. The epidural catheter was then threaded easily through the Touhy needle. On removal of the needle, slow backflow of clear fluid was noted. One mL of 2% lidocaine with 1:200000 epinephrine was injected without cardiovascular symptoms. The catheter was managed as an intrathecal catheter using continuous infusion of ropivacaine and fentanyl throughout labor. The patient required multiple additional bolus administrations of ropivacaine and fentanyl through the catheter because of patchy pain relief. Labor did not progress adequately and she was eventually taken to the operating room for cesarean section. Attempts were made to achieve surgical anesthesia by bolus local anesthetic administration through the intrathecal catheter, but these resulted in a primarily right-sided block with mostly intact left sided sensation. The decision was made to proceed with general endotracheal anesthesia. Anesthesia was uneventful and her trachea was extubated at the end of the surgery. The intrathecal catheter was left in place for 24 hours after cesarean section with the thought this may decrease the likelihood of postdural puncture headache.3 The catheter was removed intact. At the time of catheter removal the patient complained of mild postural occipital headache, which was treated with fluids and caffeine. Her headache was mild so an epidural blood patch was not offered at that time. She was discharged on post-operative day 3 with continued mild headache.
The patient’s headache continued to worsen and six days after catheter placement, she developed double vision. She was seen by her primary physician 8 days after catheter placement and referred back to the hospital for management of headache and diplopia. On examination she was noted to have left cranial nerve VI palsy. Neurology and ophthalmology were consulted and a CT head and MRI brain scans were obtained (Figure 1 & 2). The MRI showed low lying cerebellar tonsils, partial effacement of the basal cisterns, small bilateral extra-axial fluid collections overlying the cerebral hemispheres, prominent pituitary gland and enlarged dural venous sinuses. These findings were consistent with intracranial hypotension. The obstetric anesthesia service performed an epidural blood patch with 20 ml autologous blood. The headache improved and she was discharged later that day with scheduled follow up with neurology and ophthalmology. Repeat MRI done 13 days after the initial MRI showed resolution of the features of intracranial hypotension (Figure 3), however the patient still had a disabling cranial nerve VI palsy that was managed conservatively with an eye patch. Approximately 1.5 months after epidural placement she continued with unchanged diplopia. She was prescribed a Fresnel prism to help her tolerate the diplopia and was referred to the strabismus clinic. At her follow up appointment 2.5 months after epidural placement she reported almost complete resolution of her cranial nerve VI palsy.
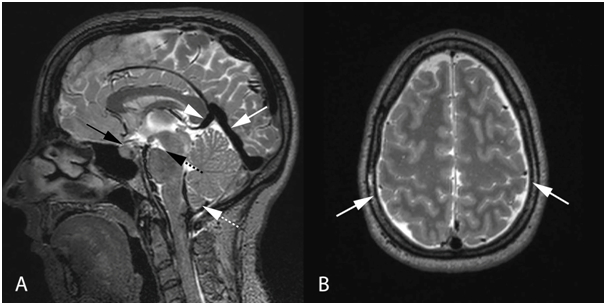
Figure 2 Sagittal T2 weighted MRI (A) demonstrates distended dural sinuses (white solid arrow), prominent pituitary (black solid arrow) and mild downward displacement of the cerebellar tonsils (white dashed arrow). Central brain descent causes a "closed" pons-midbrain angle (black dashed arrow) and there is mild depression of the internal cerebral veins/vein of Galen junction by the splenium (white solid arrow head). Axial T2 weighted MRI (B) demonstrates small bilateral extra-axial fluid collections (white arrows).
This case illustrates the potential for serious complications related to placement of an epidural catheter. Although cranial nerve VI palsy is uncommon after accidental dural puncture, it is important to inquire about diplopia as early recognition may be critical for recovery in these patients.
Diplopia due to cranial nerve palsy typically presents four to ten days after dural puncture, but has been documented one day to three weeks following dural puncture.4 The rate of cranial nerve palsy after dural puncture is estimated at between 1 in 400 and 1 in 8,000 dural punctures (varying based on the needle type, needle size and number of dural punctures). One observational report of 9,277 spinal anesthestics found six cases of diplopia, all of which occurred with the use of 16-gauge spinal needles (a rate of 1 in 140).5 No cases of diplopia were observed for 8439 patients who received spinal anesthetic through 19 or higher gauge needles. The prognosis is generally favorable with 89% of patients experiencing full recovery. The time course for full recovery varies widely, from 2 weeks to 8 months, with the majority recovering within 2-3 months. Cranial nerve palsy can also occur after resolution of post-dural puncture headache6 or without clinically apparent dural puncture or development of headache after epidural placement,7 which may lead physicians to question a relationship to epidural catheter placement. Patients that develop cranial nerve palsies may be referred to neurology or ophthalmology without consulting the anesthesiology service, which may result in this being a less known complication of accidental dural puncture among anesthesiologists.4
Cranial nerve palsy following accidental dural puncture is thought to result from intracranial hypotension, resulting in traction on cranial nerves with subsequent damage to the nerve. This hypothesis is supported by the finding of cranial nerve palsies resulting from cases of diagnostic lumbar punctures without injection of medications8 as well as spontaneous cases of intracranial hypotension.9 MRI findings consistent with intracranial hypotension seen in this case included sagging of the brain, downward displacement of the tonsils, pachymeningeal enhancement, engorgement of venous structures, enlargement of the pituitary gland and subdural fluid collections.10
Epidural blood patch has been shown to be an effective treatment for post dural-puncture headache. Although most studies have shown epidural blood patch to be less effective in the management of cranial nerve palsies following accidental dural puncture, a few have shown some benefit. One case report documented a blood patch done within 24 hours of the patient developing bilateral cranial nerve VI palsies with both subjective and objective improvement in severity of the palsies. The cranial nerve palsies occurred 10 days after dural puncture and the blood patch was performed on the day she developed the palsies.11 The patient continued with mild diplopia for an additional 26 days, despite complete resolution of the headache 2 hours after blood patch was performed. Another case report described the use of an epidural blood patch in the treatment of a patient with spontaneous intracranial hypotension.9 After presentation to the hospital, the patient became obtunded and developed intermittent bilateral cranial nerve III palsies. A bolt was placed for intracranial pressure (ICP) monitoring and the patient’s ICP ranged -7 to 5 mmHg. CT myelography was performed and he was found to have CSF leaks at the C1-3 and T6-10 levels. The patient received a blood patch with 8 ml autologous blood at the C2 level and 21ml in the T6-7 level which provided immediate relief of headache and increased ICP to 15-19 mmHg. By the next day the bilateral cranial nerve palsies had resolved. Other case reports, however, show no immediate improvement in cranial nerve palsy following blood patch12,13 and most palsies resolved with or without blood patch.
Cranial nerve palsy is a relatively rare but severe complication of accidental dural puncture. Given the rarity of this complication and the inherent risks of epidural blood patch performance, it is unlikely that the benefits outweigh the risks of prophylactic blood patching for prevention of cranial nerve palsies, although we could not find studies that evaluated such a treatment approach. This case report also demonstrates the importance of follow-up. The question then arises; how should patients be managed if they still have a post dural puncture headache after a known dural puncture? It is not evident that we should place an epidural blood patch in all patients who still have a headache for several days following accidental dural puncture to prevent this complication. At a minimum we believe all patients who have an accidental dural puncture should have telephone follow up with anesthesia providers to ensure they have not developed any severe complications associated with dural puncture, and any complications they may have developed are managed appropriately.
Eric Gray, MSIV Loma Linda University School of Medicine, Loma Linda, CA, USA.
The authors declare there are no conflicts of interest.
None.

©2016 Cluff, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.