Journal of
eISSN: 2373-6437


Background: Post-Dural Puncture Headache (PDPH) is a common problem after a deliberate puncture of the dura-arachnoid for the purposes of diagnosis, therapy, spinal anesthesia, or unintentionally during epidural procedures. It is a clinically main complication which affects the daily life of patients with marked restriction of their physical activities. Spinal anesthesia is the frequent anesthetic procedure for obstetric patients which identified as cause for PDPH. The aim of the study was to assess the prevalence and associated risk factors of PDPH after Cesarean Section (CS) delivery under spinal anesthesia.
Method:An institution based cross sectional study design was conducted on all eligible obstetric patients who came for operation under spinal anesthesia from September, 2015 to January,2016. The data collection method was including chart review and patient follow up for three days of post operative period.
Results: 107/251 (42.6%) patients developed PDPH. Among those patiens with PDPH big needle sizes (AOR=8.6; 95% CI: 0.06-0.46) and repeated number of attempts (AOR=4.54; 95% CI: 0.52–39.14), were found to be significantly associated with the dependent variable of PDPH on the multi variate logistic regression.
Conclusion and recommendation: In this study, we showed the prevalence of PDPH was higher, 107/251 (42.6%) compared with other literatures. The study also showed that big spinal needles and repeated number of attempts were the independent associated risk factors for PDPH in Felege Hiwot Referral Hospital, Bahir Dar, Ethiopia. The higher magnitude of PDPH has to be reduced by avoiding use of big needles, and the repeated dura puncture.
Keywords: post dural puncture headache, spinal anesthesia, cesarean section, spinal needle
PDPH, post dural puncture headache; SA, spinal anesthesia; CS, cesarean section
Regional anesthesia is the favored methods of cesarean section delivery due to their safety to the mother, simplicity of the technique, lesser maternal risk and satisfactory postoperative analgesic effect.1-3 However, Post-dural puncture headache (PDPH) has been a problem for patients next to dural puncture which is the iatrogenic cause of patient’s morbidity in modern anesthesia, as well as pain management therapy after attempted epidural and spinal blocks.2 It is believed to be caused through penetration of dura matter by spinal needle with continuous cerebrospinal fluid (CSF) outflow. The concern of the new born and bond of family member may be affected by the post-operative headache.4
PDPH is explained as a bilateral headache which is associated with position. It is better during recumbence and worsened during upright position of the patient. The factors that can affect the incidence of PDPH includes age, gender, pregnancy, history of PDPH, shape of needle tip, size of needle, number of lumbar puncture and needle orientation to dural matter.4,5 The association between needle size and type with incidence of PDPH was described as 75% for 16-18G needles, 30% for 22G Quinke needles and reduced to 0.37% for 27G pencil point needles.6 The most favourable needle sizes for spinal anesthesia are probably the 25G, 26G, and 27G needles.7,8 When we used smaller size of spinal needle, there will be decreased risk of PDPH, due to low CSF leakage through narrowed puncture of the dura.8 Based on the diagnostic criteria of the International Headache Society (IHS) in 2004, the Post dural puncture headache can appear up to the fifth day after the procedure and it is self limiting in a week which is defined by at least one of the following symptoms: neck stiffness, tinnitus, hypoacusia (partial loss of hearing), photophobia, and nausea are manifested.9
In Ethiopia Bahir Dar, Felege Hiwot Referral Hospital anaesthetists are doing spinal anesthesia by spinal needles with different sizes, but the same design for Obstetric patients. We did this cross sectional study for the purpose of knowing the magnitude of PDPH based on this difference of needle sizes. Therefore, we assessed the prevalence and associated risk factors of PDPH after cesarean section delivery under spinal anesthesia and finally, to disseminate the results of the practice to other anesthesia professionals and it will be base line information for other researchers.
Study design and patients
A Cross Sectional study design was conducted at Felege Hiwot Referral Hospital, North West Ethiopia from the time of duration September, 2015 to January, 2016. All consecutive cesarean section patients at postoperative period were included by fulfilling the inclusion criteria of ASA status I - II patients after Cesarean Section was done upon spinal anesthesia. There were cases rejected as exclusion criteria of Uncooperative patients, Patients with impaired cognitive ability and Patients with eclamsia.
Study variables
Dependent variable is post dural puncture headache.
Independent variables are age, body mass index (BMI), and American society of Anesthesiologist (ASA), needle size, neddle design, position, and number of attempts and previous history of PDPH.
The sample size was taken as total 251 patients in the time duration of September, 2015 to January, 2016.
Data collection
The entire procedures were performed at sitting position with different Anaesthetists who have greater than two years of experience. The backside of the patients was cleaned with Iodine and alcohol. Spinal anaesthesia was done using a midline approach at the L2-3 or L3-4 interspaces by using different size of spinal needles and 0.5 % isobaric bupivacaine 2.5-3.0ml was injected. The intra operative information could be collected by one of the data collector from each patient chart. Patients were interviewed by another data collector on day 1, 2, 3 and were questioned as regard to headache, location, character, and duration, associated symptoms like neck stiffness, tinnitus, hypoacusia (partial loss of hearing), photophobia, and nausea. PDPH was diagnosed as fulfilling the following criteria. These are headache develops within 3 days after dural puncture, headache that worsens within 15 minutes after sitting or standing and improves within 15 minutes after lying down, and with at least one of the following symptoms : neck stiffness, tinnitus, hypoacusia, photophobia and nausea were included.
Data analysis
Data were analyzed in SPSS version 20 by using bi-variant and multi-variant logistic regression. Odds ratio with 95% confidence interval and p-value were computed to determine the strength of the association. A p-value <0.05 was considered as statistical significant.
Ethical approval
Ethical clearance was obtained from Amhara Regional Health Bureau Research Ethics Review Committee (RERC), Bahir Dar. Written informed consent was obtained from the patient after clear explanation what they had to do throughout the study. Anyone who was not willing to participate in the study could resign at any time. Confidentiality was guaranteed with anonymous questionnaires and keeping them locked.
Socio-demographic & physical characteristics of the study participants
The 251 Patients were included in this study with fulfilling the criteria. However, three patients were excluded due to refusal to take the sample. The mean age of patients participated in study was 27.24 years old with a standard deviation of 5.23 years old and 18 years old is the minimum age of patients participated in this study, where as 40 years old is the maximum age. All patients were either ASA I or ASA II (Figure 1) (Table 1).
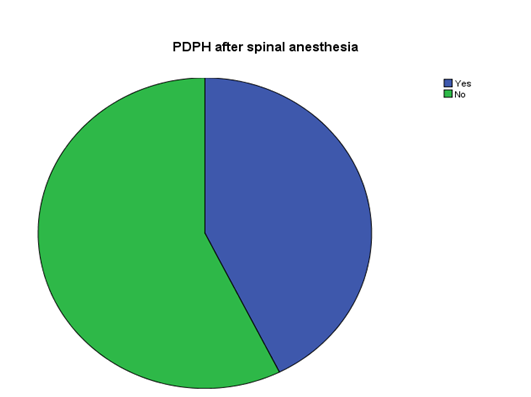
Figure 1 Proportion of patients who developed PDPH participants underwent spinal anesthesia cesarean section delivery, in the period of September 25, 2015–January 10, 2016.
Variable |
Frequency: n (%) |
Age in years |
|
18 – 30 |
196 (78.1%) |
31 - 45 |
55(21.9%) |
BMI |
|
< 18.5 (underweight) |
8(3.2%) |
18.5 – 24.9 (normal) |
222 (88.4%) |
>24.9 ( over weight) |
21 (8.4%) |
ASA status |
|
ASA I |
223(88.8%) |
ASAII |
28(11.2%) |
Table 1 Socio-demographic and physical characteristics of the study participants who underwent spinal anesthesia cesarean section, in the period of September 25, 2015 – January 10, 2016
Spinal anesthesia related parameters of the study subjects
Sixteen patients had a previous history of spinal anesthesia exposure and two of them complained a PDPH like headache after the procedure. All patients had given spinal anesthesia on sitting position. 21 G needle is the most frequently used spinal needle which is 45.4% of total patients whereas 20 G is used as 2.4%. There were 3 cases (1.2%) diagnosed as failed block which were converted to general anesthesia. None of patients developed PDPH (Table 2).
Variables |
Frequency: n (%) |
Previous spinal anesthesia |
|
Yes |
16(6.4%) |
No |
235(93.6%) |
Previous history of PDPH |
|
Yes |
6(2.4%) |
No |
245(97.6) |
Position of spinal anesthesia done |
|
Sitting |
251(100%) |
Lateral |
0(0%) |
Number of attempts |
|
Single attempts |
199(79.3%) |
Twice attempts |
42(16.7%) |
>2 attempts |
10(4%) |
Size of spinal needle |
|
20 Gauge |
6(2.4%) |
21 Gauge |
114(45.4%) |
22 Gauge |
77(30.7%) |
23 Gauge |
15(6%) |
24 Gauge |
21(8.4%) |
25 Gauge |
18(7.2%) |
A successful block |
|
Yes |
248(98.8%) |
No |
3(1.2%) |
Associated symptoms |
|
Neck stiffness |
92(36.7%) |
Tinnitus |
6(2.4%) |
Hyper accusia |
1(0.4%) |
Photophobia |
5(2%) |
Nausea |
46(18.3%) |
None |
101(40.2%) |
Table 2 Spinal anesthesia related parameters of the study participants who underwent cesarean section delivery in the period of September 25, 2015–January 10, 2016
Factors associated with PDPH
Hosmer-Lemeshow test of goodness of fit was performed to check the appropriateness of the model for analysis. Variables found to be significant at a binary logistic regression were: needle size and number of attempts. After analysis with multivariate logistic regression needle size and number of attempts were found to be significant at p-value<0.05 (Table 3). Size of the needle used to administer spinal anesthesia is significantly associated with the development of PDPH. Patients received spinal anesthesia using bigger spinal needles were more than eight times more likely to develop PDPH than patients who received spinal anesthesia using smaller needles. Another significant association was found between number of attempts and PDPH. Patients who received spinal anesthesia (SA) with multiple attempts were four times likely to develop PDPH than their counter part patients who had a single attempt.
Variables |
|
PDPH |
AOR( 95% CI) |
P –value |
|
Yes |
No |
||||
Spinal needles |
Big needles (20 G ,21 G & 22 G) |
102 |
101 |
8.6 (0.06-0.46) |
|
Small needles(23 G,24 G,25 G) |
5 |
43 |
1 |
0 |
|
Attempt |
multiple |
37 |
70 |
4.54 (0.52–39.14) |
|
Single |
15 |
129 |
1 |
0.015 |
|
Table 3 Factors associated with PDPH of patients who underwent spinal anesthesia cesarean section delivery in the period of September 25, 2015 – January 10, 2016
Prevalence of PDPH
In this study PDPH was present in 107 patients (42.6%).
Post dural puncture headache (PDPH) has been believed to be a major problem of patients after spinal anesthesia. The overall postdural puncture headache in this study was 42.6% which is comparable to Egypt study,10 but excessively higher than other studies report.9,11,12 The high percentage of prevalence of PDPH in this study might be related with the most 77.8 % of participants were received spinal anesthesias using big spinal needle. Specifically, the contribution of big needle was strongly significant association for the over all of PDPH as compared with small needles. This higher PDPH percentage after spinal anesthesia by using big needles were 8.6 times more likely to develop PDPH than small needles (AOR= 8.6; 95% CI: 0.06, 0.46; p = 0.000). This might be linked with larger needles put down wider opening on the dura which allowed more CSF pour out than smaller hole caused by smaller needles. Our finding is in line with different studies.13-16 However, we couldn’t see the associations to the outcome variable on type of design of needle, because of all were Quincke type.
The other significant association was found linking the number of attempts and the development of PDPH. The spinal anesthesia was successful at first attempts with 79.3% which is less likely to develop PDPH than those patients who have repeated attempts. In addition, patients who had an attempt of more than once are about 4.5 times at risk to develop PDPH than those patients who had a single attempt (AOR=4.54; 95% CI: 0.52, 39.14; p=0.015). This could be correlated with the number of attempt to increase the probability of piercing the dura matter repeatedly will increase the volume of CSF leak, thus increasing the probability of development of intracranial hypotension & PDPH. This finding is aligned with other studies.5,15 The proportion of repeated attempts of spinal needles related PDPH reports from a population based study in University of Basel, Switzerland (4.2 %)17 was somehow lower than our report (14.7%). However, some other studies couldn’t come across significant association between the number of attempts and PDPH.16,18,19
Even though different studies showed on variables of the lower BMI, younger age, and previous history of PDPH are listed as risk factors for PDPH development,5,14,20 our observation study did not bring into being significant association between these variables and PDPH. This might be due to the lack of sample size to compare lower to higher BMI, young to old age, and patients with versus without previous history of PDPH. There are some limitations in our study. The sample size was not sufficient for different size of needles (23G, 24 G, 25 G, and 26 G). For this reason, it was not possible to determine the proportion of PDPH in each of small needles. Our study participants were followed for three days only. However, they may develop PDPH until the seventh days of dural puncture which may underrate the overall prevalence of PDPH. We didn’t also observe the severity of post dural puncture headache.
In conclusion, the prevalence of PDPH was higher, 107/251 (42.6 %) compared with most other studies. The study also showed that big spinal needles and repeated number of attempts were the independent associated risk factors for PDPH in Felege Hiwot Referral Hospital, Bahir Dar, Ethiopia. We recommend the higher magnitude of PDPH has to be reduced by avoiding use of big needles and the repeated dura puncture.
No additional data are required; all information is clearly presented in the main manuscript.
No funding source.
Not applicable.
It was obtained from Amhara Regional Health Bureau Research Ethics Review Committee (RERC) with official permission letter to conduct the research and written informed consent was taken.
Fentahun Tarekegn conceived the study and developed the proposal, collected the data, analyzed the data and manuscript preparation. Setegn Eshetie, revised the proposal and involved in data collection, data analysis and manuscript preparation. Adugna Aregawi, revised the proposal and involved in data collection, data analysis and manuscript preparation. Kassaw Moges also revised the proposal and involved in data collection and manuscript preparation. All authors approved the final manuscript and agreed to publication in Journal of Anesthesia and Critical Care.
We would like to thank Felege Hiwot Referral Hospital anesthetists for the achievable of this study.
We declare that have no competing interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.