Journal of
eISSN: 2572-8466


Review Article Volume 10 Issue 4
Department of Biomedical Engineering, University of California Los Angeles, USA
Correspondence: Bill Tawil, Department of Bioengineering, UCLA School of Engineering, 420 Westwood Plaza, Room 5121, Engineering V. P.O. Box: 951600, Los Angeles, CA 90095-1600, USA
Received: September 04, 2023 | Published: September 21, 2023
Citation: Kelsey F, Bill T. Wound healing induced scarring: physiology, complications, treatments, and market analysis. J Appl Biotechnol Bioeng. 2023;10(4):132-137 DOI: 10.15406/jabb.2023.10.00339
Wound injuries that penetrate the deeper layers of the skin can result in scars of varying colors, textures, and sizes depending on the severity of the wound and other factors like infection and genetics.1 Although there are many types of scars, the two main scar concerns post wound healing are pigmentation and skin irritation.2 In this review, we will cover skin physiology, how scarring occurs in the wound healing process, different types of scars, common products and treatments, and an analysis of the scar treatment market including market size, distribution, and trends. Finally, we will conclude with an overview of emerging products and tissue engineering approaches for scar treatment.
Keywords: tissue engineering, scarring, wound healing, scar treatment, scar treatment market, melanin, skin, hypertrophic scar, keloid scar, flat scar, atrophic scar, scaffold
The production and deposition of melanin, a complex polymer in the skin, determines skin color.3 When wounds heal, more or less melanin can be produced in the area depending on the type of injury, resulting in a hypopigmented or hyperpigmented scar.4 On top of pigmentation, some scars can become thickened, raised bumps due to an excessive amount of collagen and connective tissue produced in the wound area.1 If left untreated, some scars can worsen - spreading and further developing bigger, elevated buildups of connective tissue on the skin that can cause complications like joint movement immobility if the scar is located on a joint.5 There are many products and medical treatments used to treat scars, but existing products are not completely effective even with long term application.5 However, advances in the development of scar treatment have helped reduce the chances of scar formation and pigmentation.4,6–8 The advantages and disadvantages of existing products will be analyzed.
Physiology of healthy skin
The skin is the largest organ of the body and serves to protect the body against harmful particles in the external environment, prevent water loss, and perform thermoregulation.2 The skin is composed of two main layers – the epidermis and the dermis.9
The epidermis is the outer most and thinnest layer of skin that consists of dead keratinized cells and acts as a barrier to protect the inner parts of skin. It also contains melanocytes, cells that produce melanin and determine skin color.10 Specifically, the epidermis is composed of 5 layers– stratum corneum, stratum lucidum, stratum granulosum, stratum spinosum, stratum basale. Stratum corneum is the outermost layer of dead keratinized cells that flake off over time as new cells are produced.9 Stratum spinosum is the layer with the most keratinocytes, cells that produce keratin, a protein that forms the skin. Stratum basale, the deepest epidermis layer, contains stem cells that differentiate into keratinocytes. The stratum basale also contains melanosomes, which are specialized organelles where the melanocytes reside.9
The dermis is below the epidermis, and consists of blood vessels, nerves, and glands.10 Specifically, the dermis has 2 regions – the papillary region and the reticular region. The papillary region is below the papillary region and has connective tissue and blood vessels that provide nutrients to the epidermis.
Melanin and skin color
Melanin is a negatively charged, hydrophobic polymer. As previously mentioned, melanin is produced by melanocytes in the stratum basale and it is responsible for skin pigmentation.9 Humans have approximately the same number of melanocytes in their skin, but the amount of melanin produced and the deposition of melanin varies, which give rise to different skin colors. There are two types of melanin – eumelanin and pheomelanin.11 Eumelanin produces brown and black pigments while pheomelanin results in red and yellow undertones. Different combinations of eumelanin and pheomelanin results in a wide range of skin colors. For example, Asian skins usually have a yellow undertone due to very few eumelanin and more pheomelanin while dark-skinned people have a lot of eumelanin. Eumelanin is prominent in the development of skin hyperpigmentation, where an area of the skin grows darker than the rest.11
Not only does melanin production affect skin appearances, melanin deposition also plays a role. After melanin is produced, it gets transferred and distributed throughout the nearby keratinocytes by melanosomes. An even distribution of pigment leads to a more uniform skin tone, while uneven distributions can cause pigmented spots like freckles.12 Moreover, melanin granules that are less clustered, more spread out through keratinocytes and travels beyond the stratum basale results in darker skin while clustered melanin distribution that stay within the stratum basale results in paler skin.13
It's important to note that eumelanin can be produced by the skin when exposed to UV radiation from the sun as a protective mechanism to absorb and dissipate the UV radiation since UV radiation can damage DNA in skin cells, leading to sunburns and cancer.14 Thus, exposure to sun can make a person’s skin appear darker as there is more eumelanin produced.14 Overall, eumelanin is harder to degrade compared to pheomelanin since it’s composed of polymers of indole-derivative units, which form more stable and compact structures, so it takes longer for dark skin to become paler naturally.13
Wound healing process and types of scars
The process of wound healing is the same for any type of wound, and it consists of three general steps: stop bleeding, cleaning, and reconstruction of the injured area. Growth factors are secreted in between each stage to trigger the initiation of the next stage.15
Scar formation begins in the last reconstruction stage. In terms of scar pigmentation, hyperpigmentation occurs due to an increase of eumelanin production during the reconstruction stage of wound healing.16,17 Inflammation can trigger the release of growth factors, which can activate melanocytes, leading to more melanin produced in the scar tissue.15 More melanin is also produced by the body to provide additional UV protection for the vulnerable newly formed tissue.8 Conversely, hypopigmentation can occur due to low levels of melanin production.4 Hypopigmentation is usually caused by deep chronic wounds, where the melanocytes are damaged (Figure 1).6
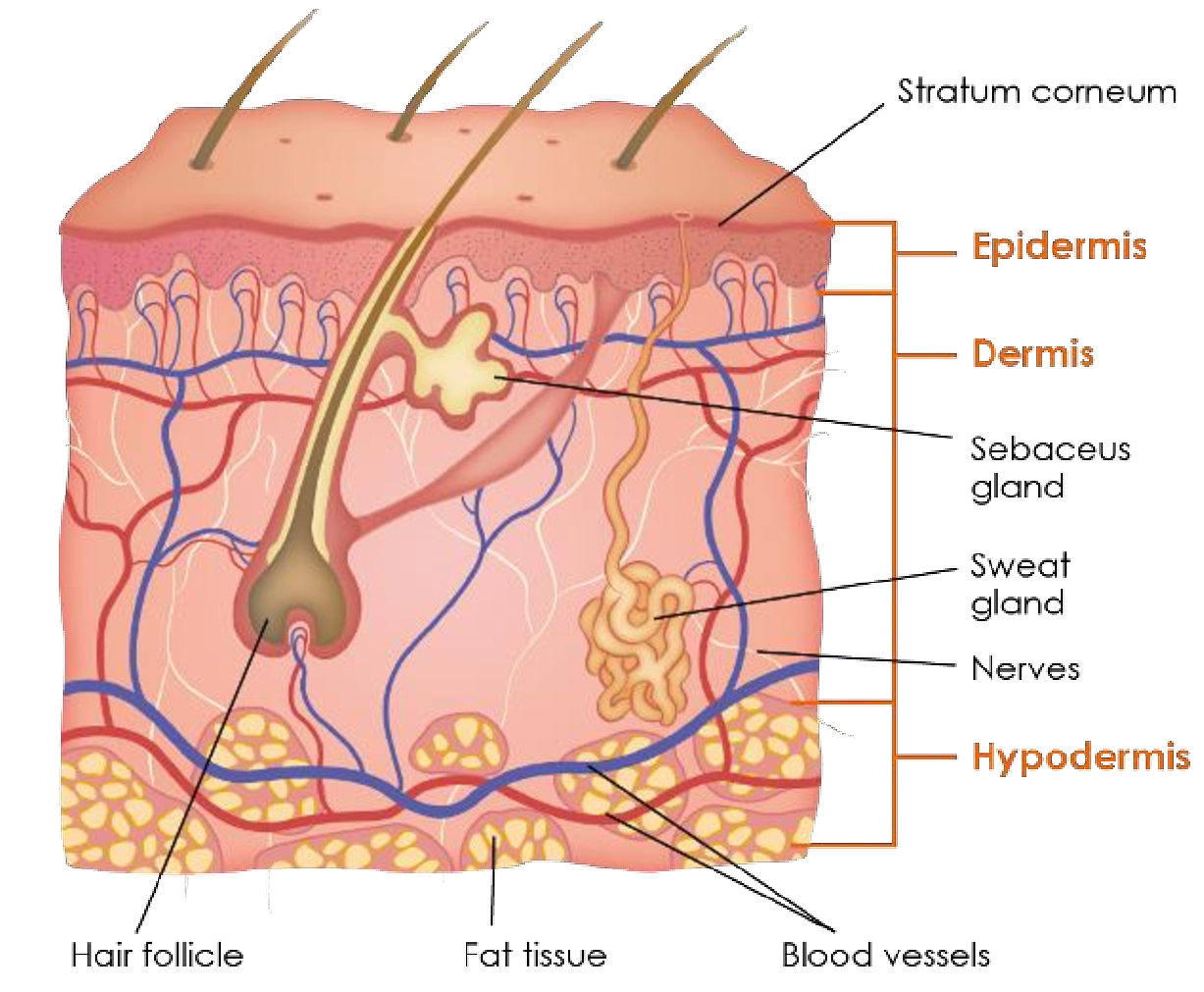
Figure 1 Cross section of skin.2
For deeper wounds in the reconstruction stage, the initial collagen matrix is reorganized and strengthened.16 Excess collagen is broken down and replaced with stronger collagen fibers, resulting in the regenerated skin exhibiting different structure and characteristics than the original, undamaged skin.18,19 The formation of a scar is influenced by several factors, including depth and size of the wound, the individual’s age, skin type, etc.5 Large, deep wounds and abnormally prolonged wound healing increases the severity of a scar.20 In general, different types of wounds caused by different injuries can form different scars.21 There are 5 general types of scars: flat, hypertrophic, keloid, atrophic, and contracture scars (Figure 2).22
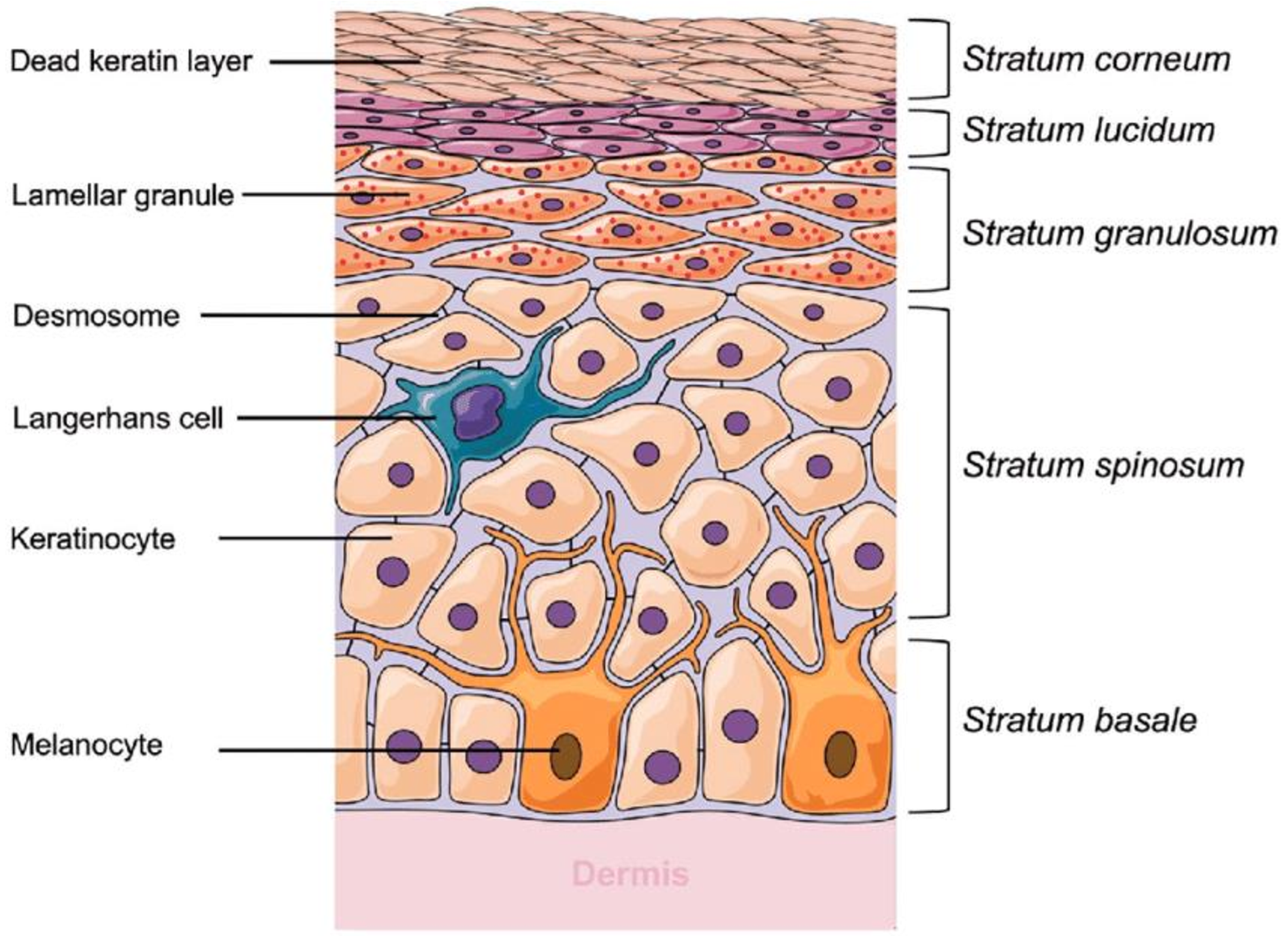
Figure 2 Five layers of the epidermis.3
A flat scar is a minor scar that’s often red or pink.23 Flat scars are the most common type of harmless scars.20 Over time, the scar can become slightly hypopigmented or hyperpigmented.2 A flat scar can be caused by minor cuts, burns, and sudden weight gain induced stretch marks.23
A hypertrophic scar forms when the collagen and connective tissue on the healed area is thicker and less flexible than the rest of the skin.1 This results in a raised, thickened scar.1 Hypertrophic scars are usually caused by more severe injury such as a knee scrape, where the deeper layers of the skin are damaged.1 Delayed healing and tension on the wound can also result in a hypertrophic scar (Figure 3).12
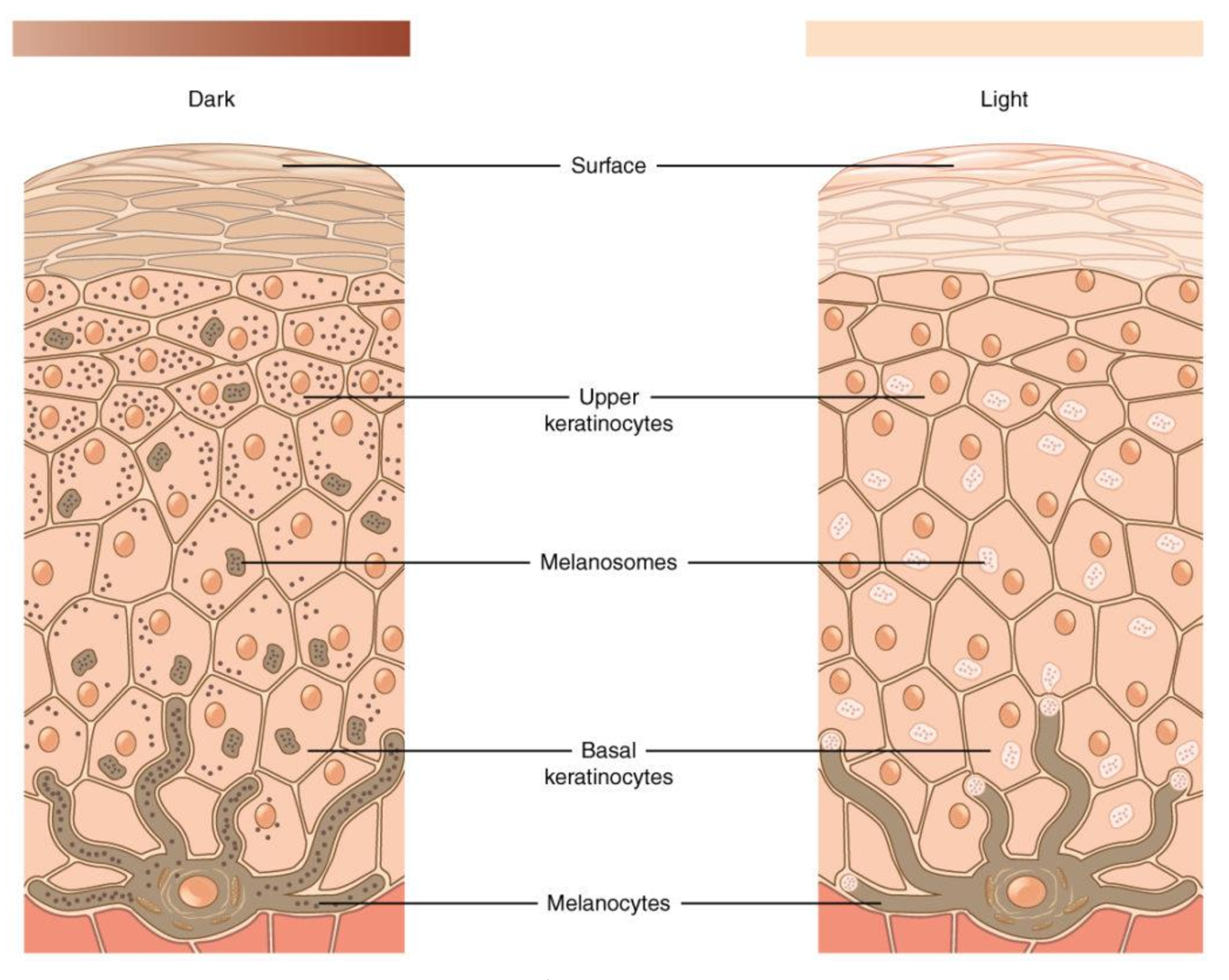
Figure 3 Differences in melanin production and deposition results in different skin colors.5
It's ideal to treat a hypertrophic scar when it first appears as it can extend beyond the original wound area and develop into a more severe keloid scar, an even thicker and raised scar.24,25 Keloid scars often lead to more complications like difficulty stretching the scarred area of skin and increased risk to skin cancer.18
Atrophic scars are sunken scars that are usually caused by chicken pox and acne.18 Atrophic scars are often hyperpigmented.19 Although atrophic scars are not harmful, they can significantly impact the physical aesthetics of a person’s face and body.
Contracture scars usually develop after a burn over a joint and cause the skin to tighten, reducing skin mobility.20 Over time, contracture scars can produce joint pain and mobility issues.12 Evidently, all scars share the trait of becoming pigmented and potentially causing skin irritations and mobility issues. Figure 4 summarizes the 5 types of scars and their characteristics.
Market size
There is no accurate data for how many people have experienced scarring globally as there is a lack of centralized reporting system for scar data and lack of awareness so many individuals with scars do not seek medical attention or report their condition. It’s also difficult to get accurate data on scar prevalence because it would require large-scale population studies.13
However, a study done in the United Kingdom revealed nearly a quarter of people living with scars have experienced short term emotional or physical problems and 14% are experiencing long term problems. Additionally, there are approximately 20 million new cancer cases each year worldwide, and 90% of these cancer patients have surgery that can lead to scarring.19 4 million people in the Western World are affected by burn injuries each year.18 There are also 50 million Americans affected by acne and acne induced atrophic scars yearly.19 These are just a few statistical examples of scar incidences. Evidently, scars are extremely prevalent worldwise.
In the United States, the scar treatment market size was at 6.3 billion dollars in 2021 and has an expected compound annual growth rate of 13.8% from 2022 to 2032.14,15
The global scar treatment market size was estimated at 25.1 billion dollars in 2022 and is expected to reach 56.76 billion dollars by 2030, indicating a compound annual growth rate of 10.7% from 2022 to 2030.24 As can be seen in Figure 4, Asian countries and the Americas have the highest demand and market size for scar treatment.16,24 Figure 5 suggests that retail pharmacies and E-commerce products hold the biggest share in the global scar treatment market, followed by clinical treatment and hospital treatments.16 Currently, the key companies at the forefront of scar treatment products are Lumenis, Merz Inc., Nutramarks Inc., Enaltus LLC, Pacific World Corporations, etc.19
Market segment and trends
There has been an overall increase in demand for scar treatments over the past years.15,19 According to Figure 6, demand in topical product increased and will continue to grow the most.15 Previously, Figure 5 also indicated that E-commerce and retail pharmacy products make up the biggest portion of the global scar treatment market, and this might be due to the Covid-19 pandemic and an increased awareness of skincare and desire for physical aesthetics.13 During Covid-19, online shopping also became more popular as people couldn’t go out to shop. 13

Figure 6 Global scar treatment market by hospital, clinical, and retail treatments.16
Additionally, as can be seen in Figure 7, atrophic, hypertrophic, and keloid scars are the biggest targeted scars of the scar treatment market.19 This makes sense because atrophic, hypertrophic, and atrophic scars are the most common scar types.24 Usually, these scars don’t need hospitalized treatment, so topical over-the-count products like creams, gels, and silicone sheets became popular as scar awareness improved.24
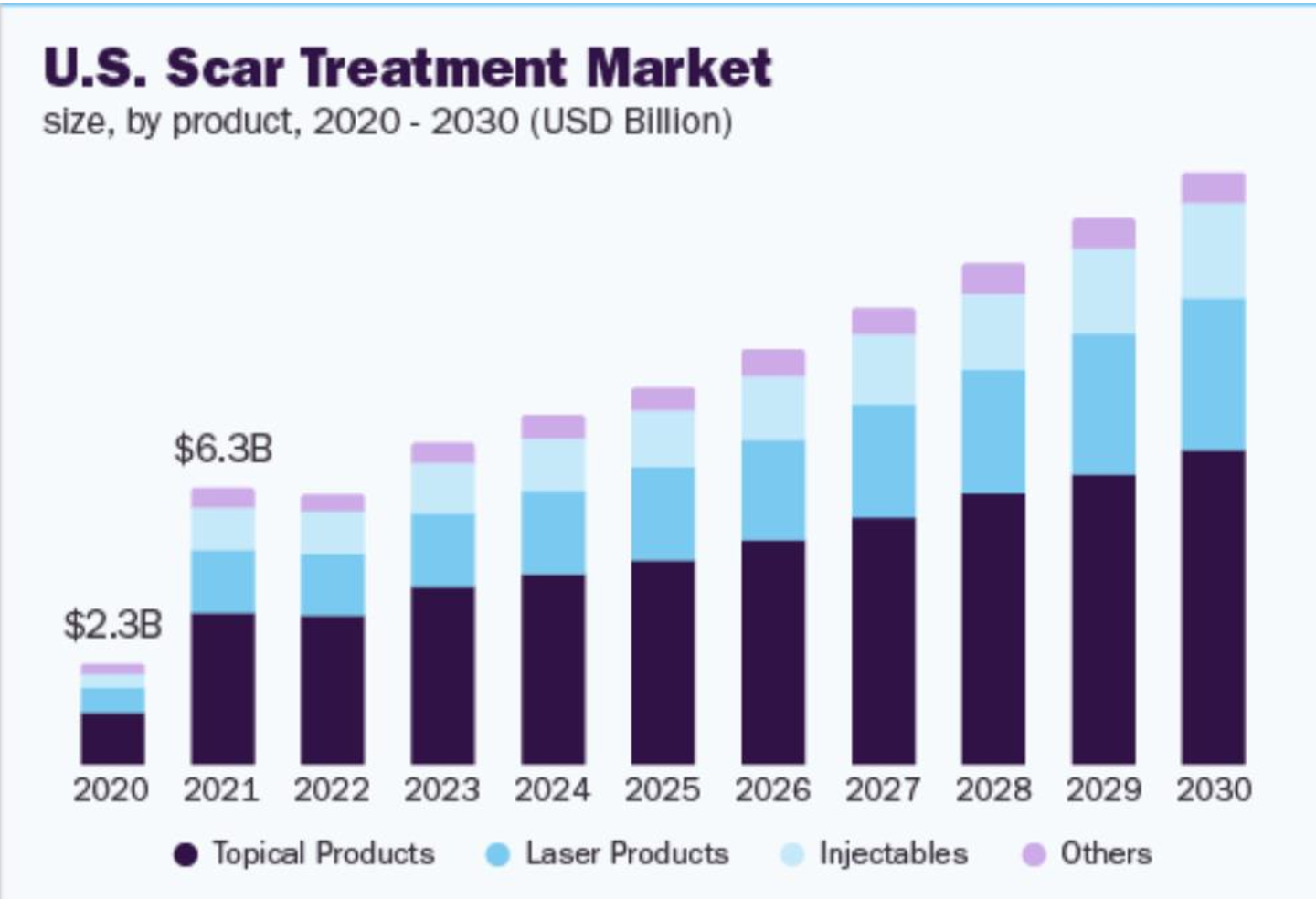
Figure 7 US Scar Treatment Market Expected Growth Trend.15
Apart from topical treatments, Figure 8 reveals the second most popular treatment are laser products.15 Laser treatments can destroy scar tissue, and are a non-invasive and painless option. Next are injectables, where substances like hyaluronic acid and corticosteroids are injected into the scars to improve their appearance. 15
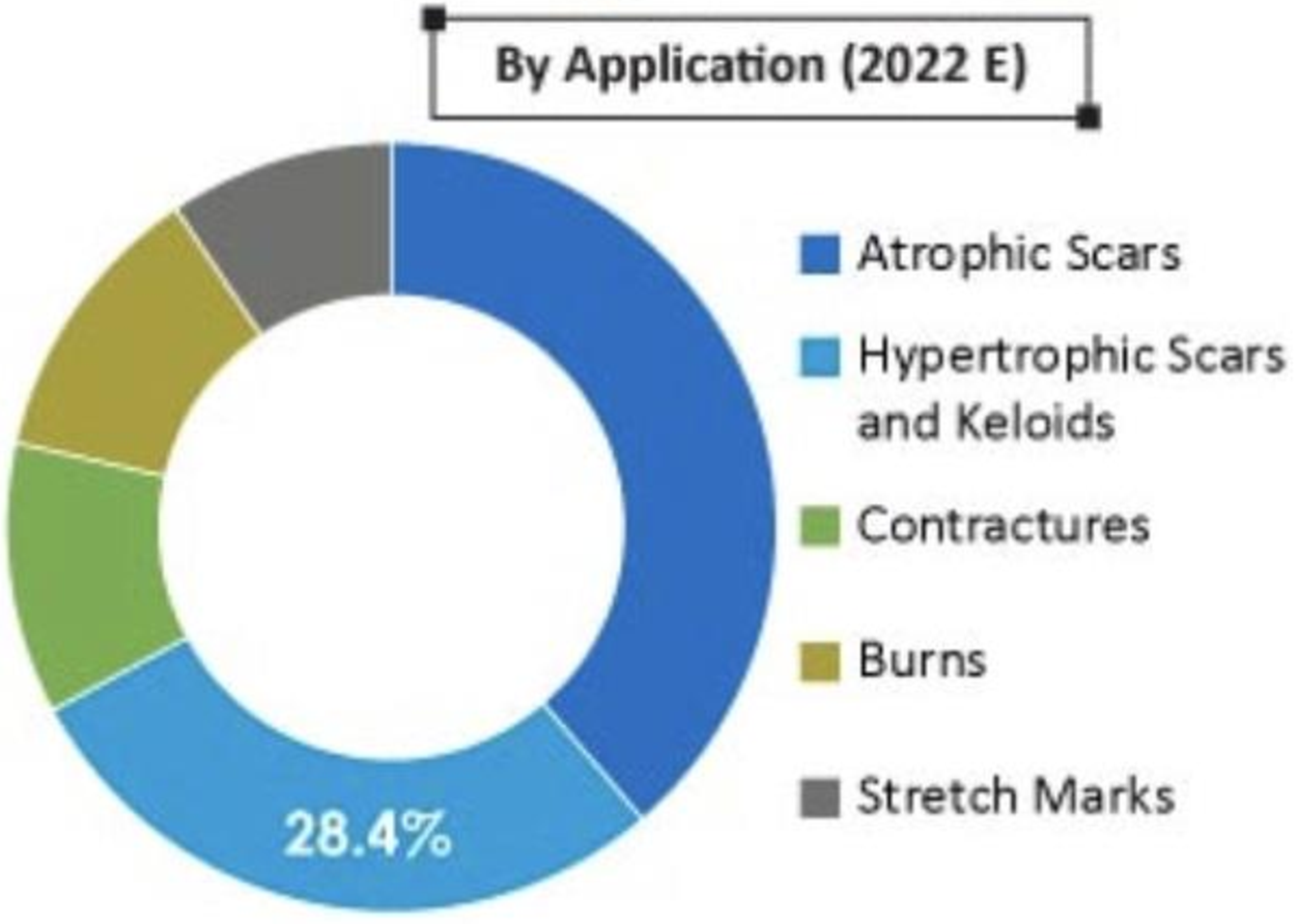
Figure 8 Market size treatment in terms of different types of scars.17
Existing products and treatments
There are 4 main treatment categories: topical treatments, injections, laser treatments, and surgery. Topical products share the same disadvantage – they are not completely effective and require daily application for a long period of time, which can be hard to do since people tend to forget to apply the product daily. 24 Some topical products that are produced by newer companies can have even less efficient scar healing properties. In a research study that studied the efficacy of silicone gel for treatment of hypertrophic and keloid scars, the researchers discovered that silicone gels produce 86% reduction in scar texture, 84% in color, and 68% in scars. 19 Although topical treatments like silicone sheets can improve the condition of the scar, it cannot completely rid the scar and its associated uneven pigmentation and texture.19
Figures 9- 11 summarize the leading products and treatment methods in each category.
There are many substances that can be injected into the scar tissue to obtain healing effects, and the most popular substances are corticosteroid, fillers, botulinum toxin, and platelet rich plasma.25 Overall, the advantages of scar injections include targeted treatment, and quick and non-invasive procedure.6 The disadvantages are that the results are temporary, there is lower scar reduction effectiveness, it’s expensive, and the procedure can cause swelling and inflammation.25
The third option is laser treatments, where laser technology is used to improve scar appearances.6 Direct concentrated beams of light are shone onto the scar tissue, which heats the deeper skin layers to trigger a wound healing response that stimulates collagen production and remodeling of collagen fibers.26 Laser treatment can also directly break down scar tissue, remove excess collagen fibers, and treat hyperpigmentation by targeting and removing unwanted melanin. 33 Advantages of scar laser treatment are targeted scar reduction, short recovery time, and versatility.26–32 Compared to more invasive surgeries, the recovery time from a laser treatment is shorter. The depth to which the laser reaches in the scar tissue can also be adjusted depending on the scar, allowing the treatment to be customized to the patient’s specific needs.33 Disadvantages of scar laser treatment are that it involves multiple sessions, side effects, and is expensive.26 Patients need to do multiple laser treatments to achieve the optimal scar reduction effect. On top of that, temporary side effects such as swelling and itching can occur around the scar. 33
The last scar treatment category is surgery, where the 4 common scar treatment surgeries are excision, Z-plasty, skin grafting, and dermabrasion.6 Figure 2 summarizes each surgery. In general, scar surgeries are not ideal since the treatment is expensive, requires a lot of time to heal, and are very invasive.22 Scar surgeries are also not suitable for widespread scars such as burn or keloid scars.27 However, advantages of scar surgeries include effective scar improvement physically and functionally, long lasting results, and the procedure can be customized and tailored to the specific scars of different patients.28
Recent developments
There are currently many emerging treatments and research dedicated to correcting scar discoloration and eliminating the chances of scarring during the wound healing process.
In 2021, Stanford researchers applied mechanical strain and drug verteporfin to surgical wounds in mice and discovered that the healed skin looked completely normal. The regenerated skin also successfully developed healthy glands. The researchers concluded that verteporfin could be used to intervene and stop fibroblasts from sensing mechanical force when skin wounds heal.29
To fix abnormal skin pigmentation, other researchers are experimenting on different ratios of eumelanin and pheomelanin to produce different skin colors and the signaling pathways that result in the production of melanin.11 The researchers found that the ratio between pheomelanin and eumelanin produced is determined by tyrosinase activity and the substrate concentrations of tyrosine and cysteine. Furthermore, interactions between Melanocortin 1 Receptor (MC1R) and melanocyte stimulating hormone α-MSH play a significant role in melanin synthesis and determining susceptibility to ultraviolet radiation (UVR). By expanding our knowledge in these areas, we can gain a more comprehensive understanding of the complex relationship between melanin, MC1R, and their impact on both pigmentation and immune response in wound healing.11
Another popular research topic for scar treatment are scaffolds seeded with proteins, polymers, stem cells, and growth factors to improve wound healing and ensure a scarless healing.24 Researchers found that tissue engineered artificial skin should contain enough polysaccharides, proteins, oxygen, and nutrients in the grafting stages to better reduce scar inflammation and eliminate scar formation.6 The polysaccharide and protein components mimic skin tissue, and the stem cells and growth factors promote wound healing and inhibit scarring. The scaffold should also continuously release oxygen, accelerating wound vascularization and reducing excessive collagen deposition. A limitation to this scaffold is that the product might be extremely expensive to produce since growth factors alone require a long time to extract and the process is very costly.
Moreover, new therapies are also being proposed for scar treatment: first, intralesional injection of botulinum toxin A has shown promise by inducing paralysis of the musculature surrounding scars, reducing tension, and leading to improvements in scar appearance. Second, mesenchymal stem cell (MSC) therapy has demonstrated the ability to modulate inflammation and exert an antifibrotic effect through the release of growth factors. Preliminary studies using MSCs in cell and animal models have shown positive results, supporting further exploration of this treatment modality. Third, fat grafting, involving the injection or grafting of fat tissue, is being investigated as an adjuvant therapy. Adipose-derived stem cells (ASCs) found in fat tissue possess properties that may improve cutaneous fibrosis and promote angiogenesis, potentially enhancing scar appearance. Fourth, interferon-α-2β, when administered with triamcinolone or postexcision of keloids, has demonstrated significant reductions in scar volume and depth, although side effects such as pain and flu-like symptoms have led to high dropout rates in some studies. Last, neutralizing transforming growth factor-beta (TGF-β) via human recombinant TGF-β1,2,3 neutralizing antibodies shows promise in inhibiting fibrosis, but such treatment options are currently unavailable. 30
Overall, these emerging therapies and research provide insights into the underlying mechanisms of scar formation and pigmentation, opening new possibilities for the development of novel approaches to enhance the wound healing process and improve scar outcomes.
Wound healing and scar formation are complex processes influenced by various factors such as the depth and size of the wound and the type of injury.15 Scars be abnormally pigmented and textured, causing aesthetic concerns and potential complications.18
The prevalence of scars worldwide is substantial, with millions of individuals affected by scars annually.31–34 The scar treatment market has experienced and will continue to experience significant growth, especially for topical products as retail pharmacies and E-commerce platforms become more popular.16,19
There are many existing products and treatments for scars, but their efficacy remains limited, necessitating further advancements in scar treatment.35 However, advancements made in scar treatment hold promise for the future of scar treatment. It is important to note that new products will be difficult to develop because there is limited knowledge of pigment production in the skin since there are many factors and patterns of scar pigmentation that are unpredictable. 4,8 Perhaps researching deeper into the science of melanin and pigmentation could help develop more innovative scar pigmentation treatments.36–45
None.
Authors declare that there is no conflict of interest.

©2023 Kelsey, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.