eISSN: 2574-9838


Case Report Volume 5 Issue 6
Konya Numune State Hospital, Department of Physical Medicine and Rehabilitation, Turkey
Correspondence: Zerrin Kasap, Konya Numune State Hospital, Department of Physical Medicine and Rehabilitation, Konya, Turkey Ferhuniye Mah. Hastane Cd. No:22, 42060 Selçuklu Konya, Turkey, Tel +905554165266, Fax +9033223567 86
Received: December 22, 2020 | Published: December 9, 2020
Citation: Kasap Z, Gerek AM. Transient osteoporosis of hip: an unusual case. Int Phys Med Rehab J. 2020;5(6):255-256 DOI: 10.15406/ipmrj.2020.05.00267
Transient osteoporosis of hip (TOH) is a rare disease with unknown etiology, generally seen in middle-aged men and pregnant women. It usually shows a benign course but rarely may be complicated. TOH usually presents with sudden onset hip and thigh pain. In this case report, a woman with TOH, who had no risk factors, misdiagnosed at the first evaluation and heals completely with conservative treatment, is presented.
Keywords: transient osteoporosis of the hip, hip pain, bone marrow edema
Transient osteoporosis of the hip (TOH) is a rare disease, commonly seen in middle-aged men and pregnant women in third trimester, and usually presents with sudden onset hip pain.1 In these patients, an antalgic gait begins within days and becomes severe enough to require the use of crutches or canes. While the patient suffers from such intense pain, physical examination does not reveal any significant findings other than minimal limited range of motion in the hip.2 The etiology of TOH is unknown. It is thought to be associated with conditions such as smoking, alcohol consumption, inflammation, vascular diseases, corticosteroid, drug usage or osteogenesis imperfecta.3 In early stage of disease, plain radiographic images are not diagnostic.4 Magnetic resonance imaging (MRI) is mainly used in diagnosis. TOH is a self-limited condition and it responds to conservative therapy in most of cases. The pain and the radiological abnormalities disappear within a few months spontaneously.1 In this report, a case with TOH without any risk factors is presented.
A 46-year-old female patient was admitted to physical medicine and rehabilitation clinic with complaints of right hip and low back pain which started 3 months ago. The patient's pain radiated to the groin and anterior thigh; it increased with standing and walking, and decreased with resting. There were no complaints of numbness, tingling, weakness, incontinence or morning stiffness. There was no history of chronic illness, smoking or alcohol consumption and any other drug usage, trauma or menopause. There was no fever or weight loss in her medical history. Lumbar MRI was performed in another local hospital, and non-steroidal anti-inflammatory and myorelaxant drugs were prescripted with the diagnosis of degenerative disc disease. The patient did not relief with that treatment. On physical examination, right hip movements were limited with pain at 100 degrees of flexion, 40 degrees of abduction, 30 degrees of internal and external rotations. Lumbar movements were within normal limits and painless. Antalgic gait was present. Knee, ankle and ankle joint movements were within normal limits. Neurological examination was normal. There was no pathological finding in pelvic plain radiography. Intramedullary bone marrow edema in the right femoral head and femoral neck, mild effusion at acetabulofemoral joint and no joint space narrowing were noted on the MRI of hip. MRI findings were relevant with transient osteoporosis of the femoral head. Bone mineral density (BMD) testing revealed Tscore of -1,4 of lomber spine and 0-5 of femur neck. In blood tests including erythrocyte sedimentation rate, hemoglobin, thyroid stimulating hormone, parathyroid hormone, calcium, phosphorus, alkaline phosphatase levels were normal. After evaluation of clinical, laboratory and radiological findings, the patient was diagnosed with transient osteoporosis of the hip. Non-steroidal anti-inflammatory drug (NSAID) and calcium/vitamin D3 treatment was initiated; rest and use of cane were recommended. 10 days after treatment initiation, since the pain of hip decreased slightly, range of motion exercises were started. After 2 months, the patient was independently ambulatory without walking aid; hip joint movements were within normal limits and painless.
Transient osteoporosis of the hip is a self-limiting, benign disease characterized by bone marrow edema in the femoral head. Symptoms and radiological findings of the patients spontaneously resolve completely within a few months.1 Rarely it may be complicated by fracture or progression to avascular necrosis.3 TOH is seen between the ages of 20 and 80 and the mean age of onset is 40. The well-known risk factor for TOH is pregnancy. Other reported risk factors include; genetic predisposition, smoking, alcohol consumption, corticosteroid usage, small vessels ischemia, hypothyroidism, low testosterone level, hypophosphatasia, low vitamin D level, osteogenesis imperfecta, bone medullary hypertension and compression of the obturator nerve.3,5 It is usually seen in middle-aged men and pregnant women in third trimester. It can rarely be seen in adults without any risk factors,6,7 as in this case. Patients with no risk factors may be misdiagnosed, as well. The woman in this case report was diagnosed with degenerative disc disease, in her first clinical setting. In disorders of low back region, the pain can radiate to the hips and lower extremities, as well as in disorders of hip, the pain can radiate to low back region. In addition, low back pain may develop secondary to gait disturbance caused by pain of hip. For this reason, it is important to determine the pain localization clearly with a comprehensive physical examination and to evaluate the patient with appropriate laboratory and imaging modalities.
MRI and plain radiographic images should be used in combination in the diagnosis of TOH. At the onset of the symptoms, presence of femoral head marrow edema with/without mild joint effusion on MR imaging and osteopenia on plain radiography 8 weeks after the onset of symptoms support the diagnosis. Osteonecrosis and septic arthritis should be considered in differential diagnosis of TOH.8 In this case plain radiaograhy wasn’t applied 8 weeks after the onset of symptoms. However the MRI findings were completely relevant with TOH.
Conservative treatment is highly recommended, since TOH responds well. It includes; rest, preventing from weight-bearing, using walking aids, analgesic drugs and physiotherapy.3 In order to prevent contractures and muscle weakness, range of motion exercises and strengthening exercises (esp. abductor muscle) should be started as early as possible.9 The patient in this case report relieved with conservative treatment including rest, cane usage, NSAID and range of motion exercises. There are some reported cases in literature which are treated successfully by calcitonin10,11 bisphosphonates12–14 or teriparatide15 but further controlled studies are needed to support these findings (Figure 1).
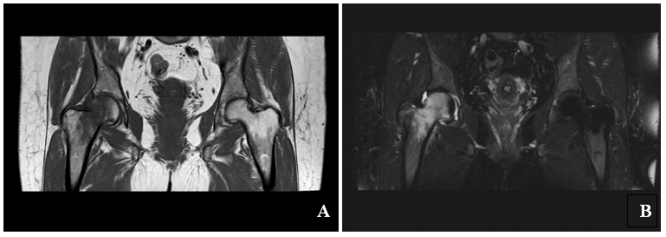
Figure 1 1 MRI of the right hip.
A. T1 coronal- T1W coronal image shows extensive edema with signal hyperintensity in head and neck of right femur with concomitant joint effusion.
B. T2 spair coronal- Coronal T2 fat-saturated image shows extensive marrow edema in the femoral head and neck, mild edema in the medial acetabulum and
a small joint effusion.
In cases of sudden onset hip and thigh pain, transient osteoporosis of the hip is one of the diagnoses that should be considered. It often heals completely spontaneously, but since rarely it may be complicated, early diagnosis and treatment is of great importance.
None.
No potential conflict of interest relevant to this article was reported.

©2020 Kasap, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.