eISSN: 2574-9838


Case Report Volume 8 Issue 1
1Department of Physical Medicine, Central Region Rehabilitation Medicine Center - Rovisco Pais, Portugal
2Department of Neurology, University Hospital Center of Santo António, Portugal
Correspondence: Xénia Verraest, Central Region Rehabilitation Medicine Center - Rovisco Pais, Rua da Fonte Quente, Tocha, Portugal, Tel +351912877528
Received: February 19, 2023 | Published: March 6, 2023
Citation: Verraest X, Ermida F, Paiva A, et al. Rehabilitation of a rare presentation of tuberculous meningoencephalitis: a case report. Int Phys Med Rehab J. 2023;8(1):51-52. DOI: 10.15406/ipmrj.2023.08.00334
Tuberculous Meningoencephalitis (TBM) is an infectious disease of the central nervous system caused by Mycobacterium tuberculosis. It mainly involves the meninges and brain parenchyma, as well as the spinal cord and meninges. The spectrum of complications of TBM includes hydrocephalus, tuberculoma formation and stroke. Stroke secondary to TBM can cause irreversible brain damage and lead to poor clinical outcomes. TBM diagnosis is challenging due to atypical early symptoms and delayed laboratory examination. Therefore, early identification, diagnosis and treatment are often difficult. Rehabilitation is one of the key components in managing TBM and is expected to enhance recovery and prevent disabilities.
Keywords: tuberculous meningoencephalitis, complications, stroke, rehabilitation
CSF, cerobrospinal fluid; MRI, magnetic resonance imaging; TB, tuberculosis; TBM, tuberculous meningoencephalitis
A 26-year-old man was admitted in our Rehabilitation Unit in May 2022 after being diagnosed with TBM. The patient presented to the emergency department with a 2-week history of fever, disorientation, decreased lower limbs strength and urinary incontinence. He had a recent history of contact with tuberculosis (TB), with a positive interferon gamma release assay test. Brain magnetic resonance imaging (MRI) with gadolinium contrast revealed hydrocephalus and diffuse leptomeningeal enhancement with basal cistern involvement (Figure 1). Acute ischemic brain lesions with hemorrhagic transformation in the right globus pallidus and anterior limb of internal capsule consistent with infarctions due to infectious arteritis, were also noted (Figures 2 & 3). Spine MRI with gadolinium contrast revealed diffuse cervical, thoracic, lumbar and sacral enhancement of meninges overlying the spinal cord and cauda equina nerve roots (Figure 4). These images were suggestive of TB infection. Blood cultures, serologies and cerebrospinal fluid (CSF) culture were negative for TB bacilli and he had no relevant medical history, including risk factors for being immunocompromised. Nevertheless, presumptive diagnosis of TBM was made in the setting of relevant clinical and epidemiologic factors in combination with typical CSF and MRI findings.
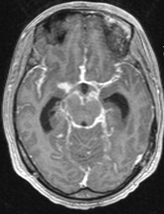
Figure 1 Brain MRI T1 with gadolinium contrast images, axial view - diffuse leptomeningeal enhancement with basal cistern involvement.
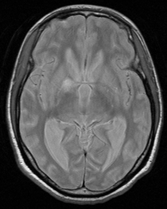
Figure 3 Brain MRI T2 images, axial view - acute ischemic lesions with hemorrhagic transformation in the right globus pallidus and anterior limb of internal capsule consistent with infarctions due to infectious arteritis.

Figure 4 Spine MRI with gadolinium contrast, sagittal view - diffuse cervical, thoracic, lumbar and sacral enhancement of meninges overlying spinal cord.
The patient was treated with a regimen of four anti-tuberculous drugs combined with corticosteroids and rehabilitation was started. During hospital stay, the patient revealed progressive clinical and imaging improvement and was transferred to our Rehabilitation Unit for further treatment.
At the admission in our Rehabilitation Unit, the patient was conscious, with preserved spatial and temporal orientation, preserved higher functions and cranial nerve functions. He presented left leg impaired pinprick sensation and muscle weakness, rated as grade 4 on hip flexion and knee extension, grade 0 on foot dorsiflexion and grade 3 on foot plantar flexion (Medical Research Council scale). The patient could walk with help of a third person and needed mild assistance in most activities of daily living. Physical therapy was arranged, including limb and trunk motion, posture and balance training and progression on ambulation training. Sensory rehabilitation was also included in order to improve sensation of the lower limb. At first, an ankle-foot orthosis was required for ambulation, but this was no longer needed as the lower limb gained strength.
After proceeding the anti-tuberculosis regimen and rehabilitation plan, the patient was able to walk without assistance and acquired independency in most activities of daily living. On physical examination, muscle strength on the left leg was grade 5 in all segments, except for foot dorsiflexion, which was grade 4.
Tuberculosis is a serious infectious disease that causes high morbidity and mortality, especially in developing countries.1 TB typically affects the lungs, but the pathogen can travel through the bloodstream and damage virtually any organ in the body. Mycobacterium tuberculosis is the most common organism causing tuberculous infection in the central nervous system. TB affecting the central nervous system accounts for 10 to 15% of all extrapulmonary manifestations of the disease and develops mostly in immunocompromised patients with pulmonary TB.2,3
TBM is a non-suppurative, inflammatory disease of the meninges and brain parenchyma caused by Mycobacterium tuberculosis. TBM accounts for 1 to 2% of cases of active TB.4 It is one of the most serious manifestations of tuberculosis infection, with one of the highest disability rates.5 Fever, headache, nausea with or without vomiting and altered consciousness and mental state are the most common manifestations. Rarely, TBM can be associated with other manifestations that seriously affect the patient’s prognosis, including cerebral infarction, subarachnoid hemorrhage and intracranial vein thrombosis. A systematic review showed that the global frequency of stroke in TBM is approximately 30%, meaning that 3 out of 10 patients with TBM will eventually develop a stroke.6,7
The pathophysiologic mechanism responsible for cerebral infarction includes obliterative vasculitis, intimal proliferation and hypercoagulable state.3 Among the involved vascular territories, the most affected by TB are those from the anterior circulation specifically the lateral striate artery, the medial striate artery and the middle cerebral artery. This corresponds to the brain region usually affected by stroke, specifically the basal ganglia and the internal capsule.6,8
Sy et al.6 found that the frequency of poor outcomes among patients with TBM experiencing stroke was 51%, with a mortality rate of 21%. Thus, early initiation of appropriate therapy is crucial to improve prognosis. The current treatment guidelines recommend as first-line therapy for 2months regimen of isoniazid, rifampicin, pyrazinamide and ethambutol followed by 10months of combined therapy with isoniazid and rifampicin. Other therapeutic interventions to reduce the frequency of stroke in patients with TBM included steroids and antithrombotic therapy.6,9
Rehabilitation programs are an effective way to prevent and reduce disabilities caused by severe illness, especially if they are started early in the course of the disease. When the rehabilitation program is started only after the infection is cured, it is more challenging to treat the disability that has already occurred.10
Although relatively uncommon, stroke can be a manifestation of TBM. An early diagnosis and treatment are fundamental to improve the patient´s prognosis. Our case report underlines the importance of rehabilitation in managing TBM and its associated complications.
None.
The authors have no conflicts of interest to declare.
None.

©2023 Verraest, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.