eISSN: 2574-9838


Case Report Volume 9 Issue 2
1Resident Physician in Physical Medicine and Rehabilitation. University Hospital of Donosti, San Sebastian -Gipuzkoa, Spain
2Specialist in Physical Medicine and Rehabilitation. Ceadac Centro de Referencia Estatal de Atención Al Daño Cerebral, Madrid, Spain
3Resident Physician in Physical Medicine and Rehabilitation. Hospital Clínico Universitario San Carlos de Madrid, Spain
Correspondence: Buran Sevik Öznur, Resident Physician in Physical Medicine and Rehabilitation. University Hospital of Donosti, San Sebastian -Gipuzkoa, Spain
Received: July 31, 2023 | Published: May 31, 2024
Citation: Öznur BS, Carlos GA, Pilar CRM, et al. Gait assessment by means of portable devices in patients with acquired brain damage. Int Phys Med Rehab J. 2024;9(2):70-73. DOI: 10.15406/ipmrj.2024.09.00377
Introduction: Currently, there is a large part of the adult population affected by a stroke or cerebrovascular accident, and it is the second cause of death and the first cause of acquired disability.1 The high incidence of stroke pathology and the dependency caused by hemiplegia make gait retraining necessary as the main objective in order to recover the patient's autonomy in terms of functionality in activities of daily living and social inclusion.2
Material and Methods: In this study we present the case of a 46-year-old male patient diagnosed with hypertensive hemorrhagic stroke in the left basal ganglia with right hemiparesis. The objective of this study is to objectively analyze gait using portable devices and indicate the appropriate rehabilitation treatment in patients with acquired brain damage. We objectively analyze gait using portable devices and indicate the appropriate rehabilitation treatment in the patient affected by acquired brain damage. As portable devices we use the Bgait mobile application and superficial electromyography to measure neuromuscular involvement.
Results: Functionally, the patient presents a significant increase in the capacity of the walking without the need for support products, reaching a community speed without Limitations after opportune treatment based on assessment using portable devices.
Conclusion: We think that carrying out the study of gait using portable devices with the incorporation of new technology such as mobile applications, easy to apply in clinical practice, demonstrates the objective values allowing for a precise evaluation.
Keywords: stroke, gait assessment, portable devices, acquired brain damage
ADL, activities of daily living; FES, functional electrical stimulation
Currently, a large part of the adult population is affected by stroke or cerebrovascular accident, and it is the second leading cause of death and the first cause of acquired disability.1 As a result of the stroke tissue damage to the central nervous system, there is a decrease in the ability to perform activities of daily living that greatly reduces the quality of life and increases comorbidities and health care.2,3 Increased dependence on third parties for the performance of basic activities of daily living (ADL) is one of the negative consequences that suddenly appear in the lives of stroke survivors and that has an undeniable influence on their quality of life.4 The high incidence of stroke pathology and the dependence caused by hemiplegia make it necessary to retrain walking as a main objective in order to recover the patient's autonomy with a view to functionality in activities of daily living and social inclusion.5 After a period of three months, approximately 20% will need a wheelchair and 60% will have limited walking, so that one of the main objectives in post-stroke rehabilitation will be the early recovery of walking, since this has a major impact on the patient, his environment and the expense involved for social and health services.6 Furthermore, the ability to walk is a determining factor in a person's ability to return home after a stroke.7 Motor deficits include alterations in postural control of the trunk and walking ability, characterized by irregular movement patterns, reduced speed and asymmetric positions.8,9 The most characteristic manifestation of moderate stroke is gait asymmetry, in terms of a longer stance phase duration in the non-paretic limb.9 There is a continuing need to improve the efficacy of gait rehabilitation for stroke survivors.9 The aim of this study is to analyze gait using portable devices in an objective manner and to indicate the appropriate rehabilitation treatment for patients with acquired brain injury.
Personal background
No history of known drug allergies. Hypertension without previous treatment, mixed dyslipidemia, grade I obesity and altered basal glycemia controlled with dietary measures. Operated on traumatic right epidural hematoma in 2016 and no present sequelae. In the same polytrauma he suffers from dorsal costal and vertebral fractures.
Present illness
After performing imaging tests, left basal ganglia hemorrhage (LBBG) was evidenced and the patient was admitted to the stroke unit with an initial diagnosis of intraparenchymal hemorrhage of the left LBBG with possible hypertensive etiology. In the control of imaging tests, the hematoma persists with a decrease in size with mild perihemorrhagic edema. Resolution of the subarachnoid hemorrhage component with only antihypertensive treatment. In the following days, blood pressure was monitored and the clinical and radiological evolution was favorable, ruling out macrovascular etiology. In the functional assessment in the days prior to hospital discharge 20 days after the hemorrhagic event, she tolerated sitting with persistent paresis of the right lower extremity and plegia of the right upper limb with a value of 4 on the modified ranking scale, for which a transfer to our rehabilitation center was requested. While waiting to be transferred, he underwent physiotherapy for gait re-education for four months, walking with a 4-point cane for short distances, alternating with a wheelchair for long distances, supervised by a third person.
Initial physical examination at the center
On physical examination he is conscious and cooperative with no alterations of language, voice or articulation. Cranial nerves not affected except for slight left facial paresis. Swallow reflex present and without swallowing disorders. Good trunk control with ease of turning and transition to sitting independently. Joint balance in left hemi body without alterations. Right hemi body with pain at active mobility in all arcs of movement. Hands and fingers are free without pain. Increased tone in right upper limb. Exalted osteotendinous reflexes in elbow extension and exhausted clonus in right lower limb. Muscle balance in left hemisphere without alterations. In the right hemisphere with the fist and fine gripper weak against resistance with difficulty to overcome gravity in dorsal flexion of the wrist. In the right lower limb at the level of ankle flexion is able to overcome gravity but with more weakness compared to the contralateral side being unable against resistance.
Altered tactile and proprioceptive sensitivity in the palmar side of the right hand without alterations in the rest of the body. No involuntary movements. He is able to move from chair to standing independently. Negative balance maneuvers. In the functional assessment by means of scales, she scored 3 out of 5 on the modified Rankin scale, 55 out of 100 points on the Barthel index with a 5 needing help in feeding, toilet dependence, dressing, grooming, a 10 with minimal dependence in transfers, a 10 needing help in ambulation and a 5 needing help in stairs. In instrumented activities according to the Lawton scale, she scored 0 points, which corresponds to total dependence. On the functional independence scale (FIM) 80 points out of 126 points. In the Nottingham extended ADL Index scale, she scored 1 point out of 22 points. Urinary and anal continent. In the observational assessment of the gait with the support of a 4-point cane, which she handles correctly. Slow and cautious. Alternating steps with asymmetry in the control of hip flexion-extension and right knee. Correct heel/toe plantar support. Correct weight transfer. Broad base rise and turn. After the initial assessment, treatment is indicated with the objective of gait reeducation with techniques oriented towards functional recovery that include electromechanical methods (treadmill, functional electrical stimulation (FES), to improve the pattern. It is included in the rehabilitation program with multiple sessions. Performs four supervised physiotherapy sessions, for one hour a day 4 days a week, one of which is treadmill training with Fesia walk Figure 1. Exercises with Fesia walk, supervised by the rehabilitation physician indoors, in the hallway of the center, for half an hour 3 days a week. She participates in group motor workshops supervised by the physiotherapist 3 days a week. Finally, he participates in sports workshops monitored by the center's trainer for half an hour 2 days a week.
Six months after the initial examination at the center, a gait study was performed using multiple portable devices in three consecutive stages:
Assessment protocol: timed measurement of 10-meter gait.
Results:
Conclusion: > 0.8 m/s which corresponds to a walker in the community without limitations.
Assessment protocol: Balanced Gait Test using BGait smartphone app Figure 2. It is based on the identification of the four phases of the gait cycle. It calculates the average value of accelerations and the duration of these phases in each cycle. The movement of one leg is compared to the opposite leg (gait symmetry) and one step is compared to the next (gait homogeneity). These parameters allow the evaluator to differentiate unbalanced gait (less homogeneous and symmetrical) from balanced gait.
It is particularly suitable for monitoring the state of gait during rehabilitation processes, using a cell phone app that measures the accelerations that occur when walking.
As a summary: The patient obtains a value of 31.75% of dynamic stability and a value of 36% of swing impulse. Both the Dynamic Stability value (which is a measure of gait quality that aggregates in a single value all the symmetries and homogeneities obtained in the test) and the Swinging Impulse value (which represents the propulsive impulse generated in the affected lower limb in the final phase of stance) present a low level of symmetry. The gait analyzed is considered to be rather unbalanced.
Assessment protocol: study performed with Surface Electromyography (Delsys System), with recording of the signal amplitude of the right and left external gemellus and right and left tibialis anterior muscles during a 15-second gait.
Results: In relation to the signal amplitude obtained from the right external calf and left external calf muscles, 85.6% more of the healthy calf than the affected calf was obtained during a 15-second gait Graph 1, 85.5% in a gait cycle Graph 2 and 97.9% in the take-off phase of a gait cycle Graph 2.
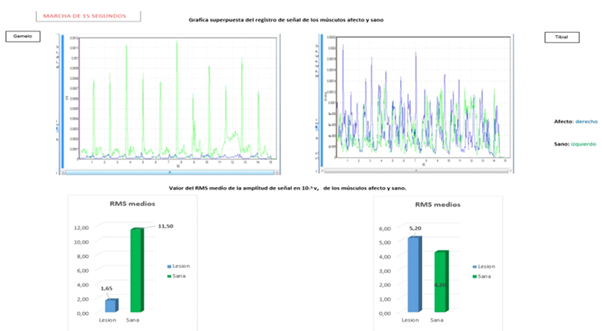
Graph 1 In 15 second walking cycle. Gemeli and tibialis activity on both sides. Average RMS values. RMS: root mean square output.
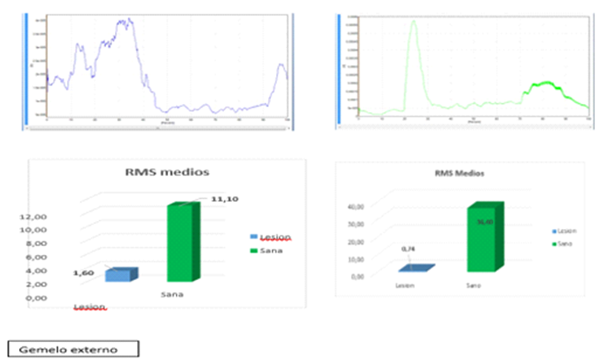
Graph 2 Gait cycle, external gastrocnemius activity in both limbs; Value of the average RMS of the signal amplitude at 10-5 V, of the affected and healthy muscles in the complete gait cycle. RMS: Root Mean Square Output - right external gastrocnemius, - left external gastrocnemius; Value of the average RMS of the signal amplitude in 10-5 v, of the aged and healthy calves in the take-off phase of gait. RMS: Root Mean Square Output.
Regarding the signal amplitude obtained from the left tibialis anterior and right tibialis anterior muscles, 23.8% more of the affected tibialis anterior is obtained with respect to the healthy tibialis anterior during a 15-second gait (Figure 1) and 60% in a gait cycle. In the swing phase of an average gait cycle, 39% more of the healthy tibialis is obtained with respect to the affected tibialis.
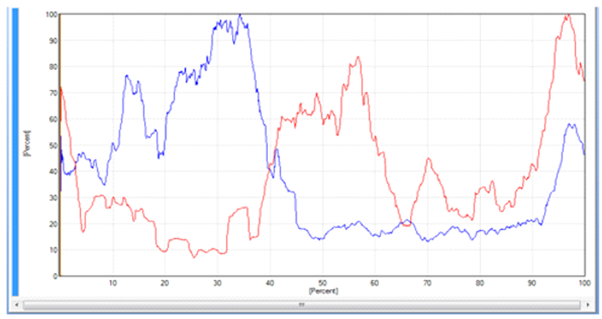
Graph 3 Gait cycle of: Right lateral gastrocnemius and anterior tibial in percentage of signal amplitude.
Conclusion: there is a significant contraction deficit of the affected calf in the stance phase, and to a lesser degree in the tibialis anterior in swing. Stance and swing phase durations are very close to normal. The co-contraction ratios are especially high in the initial contact and swing.
There is a significant contraction deficit of the affected calf with respect to the healthy calf in the swing phase (the greatest degree of contraction occurs in the mid-stance phase). In the case of the tibialis anterior there is also a deficit in the swing phase, although to a lesser degree. The duration of gait phases in the affected lower limb is within the reference ranges. Therefore, the main alteration in the gait cycle is the lack of activation of the affected calf in the swing phase, with a lesser degree of alteration in the activation of the tibialis anterior in the swing phase.
The measurements of the maximum (1.01 m/s) and self-selected (0.89 m/s) gait speed correspond to the upper level of the unrestricted community walker. Considering together the low level of gait symmetry, the low level of swing impulse and the very low activation of the plantar flexors as well as the high hip flexion in swing it can be concluded that the propulsion deficit resulting from the lack of activation of the calf is compensated to reach a sufficient speed, possibly at the expense of the contralateral lower limb and to a lesser extent of the hip flexors of the affected lower limb Figure 3. After gait study, treatment is indicated mainly to improve the gait pattern with the aim of reeducation of the affected limb trying to improve propulsion during the swing phase by means of functional electrostimulation. It can be used with specific programming to activate plantar flexion in the swing phase. Rehabilitative therapies such as orthoses and botulinum toxin are discarded.
Functionally, the patient presented a significant increase in walking capacity without requiring support products, reaching a community speed without limitations. In the analytical study of gait, there is a limitation in plantar flexion activation in the swing phase. The propulsive force is achieved with compensations to maintain the speed that allows a community gait. In terms of daily activities, there was an improvement of 40 points (from 55 points in the initial evaluation to 95 points in the second evaluation) according to the Barthel index. Regarding the subjective perception of balance assessed in 16 items according to the balance confidence scale (ABS- The activities- specific balance confidence scale), there was an improvement of 60%, so the patient is more confident when performing daily activities. The improvement in the Nottingham scale score from 1 to 19 points is noteworthy.
In patients with acquired brain injury, gait disturbance is one of the determining factors of the degree of disability and quality of life.2 Patients use compensatory strategies to achieve sufficient propulsion to maintain the speed compatible with community walking. However, these adaptations require a higher energetic cost, so it is important to try to correct them. Therefore, high speed treadmill gait training can be performed with possible programming in plantar flexion of the FES. Recovery of the same means improvement of functionality allowing patient autonomy. Therefore, correct assessment during the rehabilitation process is crucial. In the literature there are several methods of gait evaluation, although there is equipment for biomechanical assessment, in general they are expensive and are not available for routine clinical practice. For this reason, we believe that gait study by means of portable devices with the incorporation of new technology such as mobile applications, easy to apply in clinical practice, demonstrates the objective values allowing an accurate assessment. It also increases the safety of the rehabilitation process after confirming the deficits by numerical measurements.
None.
The author declares that there is no conflicts of interest.
None.

©2024 Öznur, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.