eISSN: 2574-9838


Research Article Volume 4 Issue 4
Department of Physical Therapy, California State University, Fresno, USA
Correspondence: Monica J Rivera, Department of Physical Therapy, California State University, 5315 N. Campus Drive, Fresno, CA, 93740-8019, USA, Tel (599) 278-2052, Fax (559) 278-3635
Received: June 26, 2019 | Published: August 1, 2019
Citation: Rivera MJ. Does a multi-modal intervention program influence sensory systems in persons with parkinson’s disease. Int Phys Med Rehab J.2019;4(4):166-169. DOI: 10.15406/ipmrj.2019.04.00193
Background: Persons with Parkinson’s disease (PD) display a progressive decline in function, particularly in postural control. There are however, limited investigations on the sensory deficits contributing to postural dysfunction. The Sensory Organization Test (SOT) is an outcome measure that quantifies the sensory systems. Many researchers implement the SOT in research with persons with PD, however there are limited SOT studies that compare persons with PD to same age community dwelling (CD) adults. In addition, few PD intervention studies have used the SOT as an outcome measure.
Objective: To determine if there are significant differences in the SOT between 60-70 year old persons with PD and same age CD adults. Second, to determine if there are significant gains in the SOT after a five-week multimodal intervention program in individuals with PD.
Methods and materials: In a one-group pre-post intervention design, twelve participants with PD participated in a five-week multimodal intervention program. Participants completed the pre and post-test SOT protocol, which produced an equilibrium score (ES), composite score (CS) and sensory analysis (SA) ratio score. In addition, ten CD 60-70-year-old adults completed the SOT protocol.
Analysis: The Mann-Whitney U test will analyze if there are significant differences in SOT scores between CD 60-70 year old adults compared to same age persons with PD. The Wilcoxon Signed Ranks test will analyze if there are significant differences in SOT scores pre and post intervention. IBM SPSS 26 will analyze the data. p value set at <.05
Results: The Mann-Whitney U revealed significant differences between 60-70 year old CD adults and the PD group in SOT ES 1-3 and CS, P<.05 There were no significant differences between pre and post intervention SOT scores. However, condition five ES and the SA vestibular ratio score exhibited large gains from pre to post intervention.
Discussion: The comparison results revealed significant difference in static and dynamic postural controls. In PD participants, the vestibular system displays more deficits compared to other sensory systems, but also demonstrates the capacity for larger gains after a multimodal intervention.
Keywords: parkinson’s disease, sensory organization test, multimodal intervention
Parkinson’s disease (PD) is a multifaceted neurodegenerative disease that presents with profound deficits in function, particularly in postural control.1,2 As PD is a progressive disease, there is a steady decline in cognitive, sensory and motor performance, which inevitably leads to postural instability and a higher risk in falls.3 The known motor contributors of postural instability are bradykinesia, reduced postural responses, axial rigidity and agonist antagonist co-activation.4,5 While the literature has clearly identified the motor impairments, there is not a clear consensus of the sensory contributions to postural control deficits in PD.6–8 Computerized dynamic posturography (CDP) provides a quantitative measure of sensory interactions in static and dynamic postural control.9 A specific CDP assessment is the Sensory Organization Test (SOT), which quantifies the sensory contributions in a postural activity. The SOT follows a set protocol that examines six postural conditions and calculates an equilibrium score (ES) for each condition. Additionally, the test computes sensory analysis (SA) results, which allocates a ratio score for the visual, vestibular and somatosensory systems. Researchers have implemented the studies in PD with the SOT to ascertain fall risk, establish reliability and to compare sensory function to other neurologic conditions.10–12 In addition, there are SOT studies that have compared community dwelling (CD) elderly adults to individuals with PD.13 However, there is limited research on the effects of rehabilitation interventions on sensory systems in PD and comparisons of persons with PD to healthy same age CD adults.
Multiple studies have documented the benefits of a particular therapeutic regime (aerobic, stationary bicycle, tai chi, resistive exercise).14–18 As such, a combination of aerobic, strength, balance and flexibility may serve as a more effective approach, as it may ameliorate more facets of the disease. Currently in rehabilitation, there is growing support for multi-modal interventional approaches in PD.19 Central to this approach are personalized programs, which adapt the exercise regime to the individual’s level of mobility and balance. Given the limited research on multimodal intervention programs on postural control and in particular, the effects on the sensory system, the purpose of this study is two-fold. First, to determine if there are significant differences in the SOT results between 60-70 year old CD persons with PD and same age CD adults. Second, to determine if there are significant gains in the SOT SA score and ES 1-6 after a five-week multimodal intervention program in individuals with PD.
The study was a single group pre-post intervention design in individuals with PD. Inclusion criteria were 40-85 years of age, Hoehn and Yahr (H&Y) Scale 1 to 4, stable medical regiment for over one month and the ability to follow an exercise program. Exclusion criteria were hospitalization within the last three months, a second neurologic diagnosis, cardiopulmonary disease or uncontrolled hypertension.
Recruitment for the persons with PD was a sample of convenience from the Greater Fresno Parkinson’s Support Group. Recruitment for participants began in October 2017 to December 2017 with the study beginning in February 2018 to March 2018. The study recruited 15 individuals for the study. One individual dropped out because of medical reasons, one participant dropped out of the study and one left the study for a family emergency leaving 12 individuals. There were seven males and five females with an average age of 66.6 years. The mean years of diagnosis for the participants were 6.1 years (Table 1). The 60 to 70 year old CD group was a sample of convenience from the local Fresno, CA community. The study recruited 10 individuals in this age group from January 2016 to September 2016. There were eight females and two males.
|
Age (years) |
Sex |
Hoehn & yahr |
On med |
No. falls 6 months |
Years diagnosed |
|
59 |
M |
2 |
Y |
0 |
5 |
|
59 |
F |
2 |
Y |
1 |
3 |
|
76 |
M |
2 |
Y |
0 |
3 |
|
65 |
F |
2 |
Y |
0 |
6 |
|
58 |
F |
2 |
Y |
0 |
ND |
|
74 |
F |
2 |
Y |
1 |
1 |
|
59 |
M |
1 |
Y |
2 |
2 |
|
64 |
F |
2 |
Y |
0 |
12 |
|
70 |
M |
3 |
Y |
1 |
7 |
|
82 |
M |
4 |
Y |
1 |
8 |
|
73 |
M |
3 |
Y |
2 |
12 |
|
61 |
M |
3 |
Y |
0 |
8 |
|
Me 66.6 |
7M, 5F |
2.3 |
12Y |
0.66 |
6.1 |
Table 1 Demographics (n=12)
Abbreviations Med, medication; No, number; M, male; F, female; Me, mean
Instrumentation
The CDP Bertec Balance Advantage (Bertec Incorporated, Columbus, OH), analyzes upright posture by way of force plates that detect deviations from the center of mass. The SOT assesses the vestibular, visual and somatosensory systems with a set protocol of six static and dynamic postures. Conditions 1–3 are postures with a fixed base of support (BoS) with these additional conditions: Condition 1: eyes open, Condition 2: eyes closed, and Condition 3: eyes open with a sway-referenced virtual visual environment. Conditions 4-6 consists of a sway-referenced mobile BoS with addition of the following: Condition 4: eyes open, Condition 5: eyes closed, and Condition 6: eyes open with a sway-referenced virtual environment.20 Participants undergo three trials in each of the conditions with the mean of the trials establishing an equilibrium score (ES). An ES score of 100 indicates perfect stability (no sway) while a score of zero indicates a fall. The composite score (CS) calculates a weighted average for all six conditions with the dynamic conditions 3–6 allocated higher weighting.21 To examine the individual sensory systems, the sensory analysis (SA) ratio score provides a calculation of the specific sensory system.22 Test-retest reliability of the SOT stated good to excellent reliability (ICC=.78-.90) for individuals with PD.23
Testing of participants took place at California State University, Fresno in the Department of Physical Therapy laboratory. For safety purposes, each participant donned a harness prior to the initiation of the SOT. Each participant followed the SOT procedure for force plate positioning with the medial malleolus set on the horizontal line and the lateral calcaneus set to the small, medium or large vertical line. Each participant conducted three 20-second trials for each condition. Four personnel were trained on the SOT and the protocol. These individuals tested the participant’s pre and post intervention. The primary researcher was blinded to the SOT testing.
Intervention
The multidimensional intervention consisted of 50-minute sessions 3 times per week for five weeks. Two days per week, the intervention comprised of three 15-minute intervals of exercise (agility, gait activities, and postural exercises). Agility activities consisted of side-to-side drills, obstacle course, step-ups, 90 degree turning drills, sit to stand with variations in speed and ladder drills; gait activities included ambulation in a crowded environment, mobility on uneven surfaces, transitions in gait speed, head turns while walking, and backwards walking. Postural exercises involved training in the CDP, emphasizing dynamic skills such as increasing limits of stability and virtual environmental training. Participants exercised in groups of two with supervision from trained assistant researcher. One day per week, subjects attended an adapted Yoga class, participated in flexibility exercises in various functional postures (chair, prone, supine and supported standing). The instructor is a physical therapist with expertise in Yoga.
Analysis
For the PD and CD adult analyses, the mean of three trials for SOT conditions 1-6 were calculated to produce an ES. The CDP software calculated the CS and SA ratio scores. The Mann-Whitney U test determined if there any significant differences in SOT ES 1-6, CS, and SA scores between CD 60-70 year old adults versus same aged persons with PD. For the intervention analysis, the Wilcoxon Signed Ranks test determined if there were significant differences in the ES, CS, and SA scores between pre and post intervention testing. IBM SPSS 26 analyzed the data with the p Value set at .05. If there are significant results in the study, it will include the effect size for non-parametric data, r=Z/√N.
The Mann Whitney U test revealed that the CD 60-70 year healthy adults had significant larger ES scores in condition 1(Mdn=93.0) than 60-70 year old persons with PD (Mdn=89.0), U=3.0, P=.006, r=.70. Additional findings showed the CD group showed larger ES scores in condition 2 (Mdn=92.0) than persons with PD (Mdn =88.0), U=2.5, P=.005, r=.72; and the CD adults had larger ES scores in condition 3 (Mdn=91.5) compared to persons with PD (Mdn=85.6), U=5.0, P=.014, r=.63. For the CS, the CD group showed larger ES scores (Mdn=74.5) than the persons with PD (Mdn= 66.7), U=7.0, P=.027, r = .57. There were no statistical differences in SA scores between 60 to 70 year old CD elderly adults compared to same aged persons with PD. Figure 1.
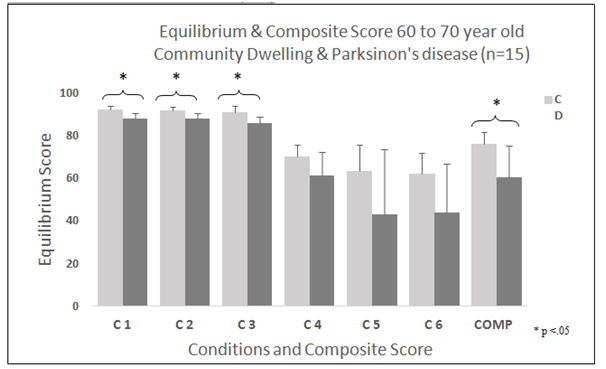
Figure 1 SOT Equilibrium and Composite Score: 60-70 year old Community Dwelling Adults versus same age Persons with Parkinson’s Disease (n=15).
Abbreviations SOT, sensory organization Test; C, conditions; CD, community dwelling; PD, parkinson’s disease
For the results of the intervention study, the pre and post ES, CS, and SA ratio scores did not reveal statistical differences. Condition 5 showed an increase from pre-intervention ES (CON5) = 51.12 to post intervention ES (CON5) = 60.48, a change of 9.16 points Figure 2. The SA vestibular (VES) ratio score revealed a pre to post-intervention gain of .082, in which 67 percent of participants increased their ratio score Figure 3. Similarly, SA vision (VIS) ratio documented a gain of 0.53. In comparison, in the SA (SOM) there was a decrease from the pre to post ratio score.
The results of the SOT comparison between the 60-70 year old CD adults and persons with PD showed significant differences in conditions 1-3 and in the CS. Conditions 1-3 involve static postural control indicating less complex tasks, while CS is a combination of all the condition scores. Notably, the numerical difference between CD adults and persons with PD was observed in ES(CON5), which was 21.8, much larger than the established minimal clinical difference of 13.33.24 Several studies in persons with PD revealed similar results, with greater deficits in ES (CON5) and SA (VES) ratio scores than ES and SA scores in their respective studies.23,25 To shed light on the differences between both groups, all CS for CD elderly adults were above the cutoff score for falls (cut off score CS<67)3, while 50% of persons with PD scored below the cut off score. Given these results, the 60-70 year old individuals with PD display substantial deficits across all conditions in comparison to same age healthy CD adults.
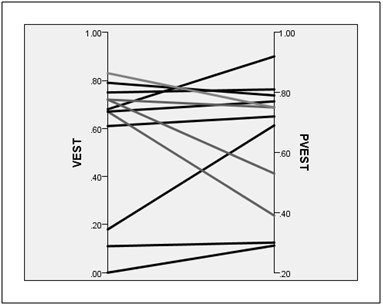
Figure 3 Pre and Post-Test Vestibular Sensory Analysis Ratio Score (n=12).
Abbreviations Pre-Vest, pre-test vestibular Ratio Score; Post-Vest, post-test vestibular ratio score
In the intervention results, there were larger gains in the dynamic conditions 4-6 compared to the static conditions 1-3, with the largest ES gains in condition 5. Condition 5 (eyes closed, engagement of the somatosensory system via the adaptable platform), represents the vestibular system. Furthermore, the largest gains in the SA ratio score was the vestibular system. It is important to note that post intervention ES for conditions 1-3 were lower than the pre-intervention scores. These results mirrors the rehabilitation approach, as the interventions emphasized dynamic posture and agility with limited emphasis on static postures. Additionally, the program included varying velocities in sit to stand activities (vertical accelerations) and walking with repetitive horizontal head turns. While there are limited PD studies investigating rehabilitation interventions in the vestibular system, researchers are hypothesizing that the vestibular system and the central processing of vestibular information may be a critical factor postural instability in PD.25–27
Future studies that focus on the sensory system in PD will need to consider the vestibular system. These investigations could include cervical vestibular evoked myogenic potentials. In addition, embedding vestibular exercises may be beneficial to a therapeutic regime. Programs can easily add alternating velocity in sit to stand, horizontal and vertical head turns in static and dynamic conditions, and vestibular-ocular activities (visual search activities in large spaces). Given the vestibular changes observed in this study, an increased emphasis on vestibular function may lead to increased sensory performance and reduce the risk of falls.
There are several limitations in this study. The first is the small sample size, the second is the lack of control group and lastly the study only applied one outcome measure to quantify the sensory systems. In the SOT comparison of CD elderly adults and the participants with PD, the small sample may lead to a type II error. Therefore, one must consider the results with some caution. Secondly, the intervention study was a one-group design, which is a threat to internal validity. Therefore, the results from this comparison study are not conclusive. Finally, a consideration is to add an additional vestibular outcome measure to better quantify the otoliths from the semicircular canals.
In comparison to CD healthy 60-70 year old individuals, persons with PD have significant differences in the SOT, specifically in conditions 1-3 and in the CS. Twelve individuals with PD who participated in a five-week multimodal intervention program showed gains in the vestibular systems; SA (VES), and ES (CON 5). Future research will need to include vestibular measures and specific vestibular activities to understand the relationship between the vestibular system and the postural control system in persons with PD.
None
I wish to thank the following individuals: Jessica Chellsen, Nazanin Ghanadan, Danielle Roche, Bethany Shirk, and Audrey Tan DPT for their assistance in this research.
The author declares no conflict of interest.

©2019 Rivera. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.