International Journal of
eISSN: 2574-9889


Case Report Volume 9 Issue 2
1Departamento de Pediatria, Hospital de Santa Maria, Centro Hospitalar Universitário Lisboa Norte, Portugal
2Serviço de Pediatria, Hospital Vila Franca de Xira, Portugal
3Serviço de Ginecologia e Obstetrícia, Hospital Vila Franca de Xira, Portugal
Correspondence: Ana Cristóvão Ferreira, Hospital de Santa Maria, Centro Hospitalar Universitário de Lisboa Norte, Avenida Professor Egas Moniz MB, 1649-028, Lisboa, Portugal
Received: April 10, 2023 | Published: April 21, 2023
Citation: Ferreira AC, Soares IP, Sousa S, et al. Umbilical cord hematoma a successful case of a non-frequent acute fetal distress etiology. Pregnancy Child Birth. 2023;9(2):75-76. DOI: 10.15406/ipcb.2023.09.00281
Background: Umbilical cord hematoma is a rare condition, with mortality rates up to 50%. Most of the literature describes cases with poor prognosis.
Case description: In this case, a healthy pregnant woman in labor presented some variable decelerations on the fetal heart rate monitoring ending in sustained bradycardia. An emergency C-section was performed, giving birth to a 40-weeks male newborn with an umbilical cord hematoma until placental insertion and, slightly stump bleeding. Newborn got pale and, had respiratory distress in the first hour of life. He presented transient metabolic acidosis with hyperlacticaemia and, anemia. There was a favorable evolution with supportive therapy. No risk factor was identified and, histological examination confirmed the diagnosis. The patient remained asymptomatic and, presented normal neurodevelopment during follow-up.
Discussion: This case report aims to demonstrate a good outcome when a high level of suspicion is taken and immediate medical and, surgical interventions are performed.
Keywords: hematoma, umbilical cord, newborn, fetal distress, case report
Umbilical cord hematomas are a rare complication of pregnancy and delivery, with an incidence between 1:5500 to 11000 pregnancies.1,2 Usually, it occurs spontaneously by the rupture of the umbilical vein,3 however, the precise cause remains unknown in most cases.2 Risk factors include anomalies of umbilical cord (short umbilical cord, cord prolapse, traction or shortness of the cord, true knots, vessels anomalies), infection (chorioamnionitis), puerperal abdominal trauma, coagulation disorders, post-maturity or, iatrogenic (in utero interventions like amniocentesis).2–4 It appears at the fetal extremity of the umbilical cord as a reddish-purple swelling of variable size.5,6
Perinatal ultrasound diagnosis is uncommon.2,3,6 Once it happens, close clinical surveillance may be done, as the risk of fetal death is high, due to constriction of maternal-fetal circulation with probable hypoxia or, anemia.5,7,8 In most cases, the diagnose is done at birth or, in the early postpartum period. In these cases, the occurrence of umbilical cord hematoma can be asymptomatic7 or, presented only with an abnormal fetal heart rate (FHR) tracing,5 implying an emergency C-section.2 Anatomopathological examination of placenta and, remaining umbilical cord should be made.7 If asymptomatic newborn or, incidentally found, the umbilical cord hematoma may have a benign course.2,9 However, higher morbidity and, perinatal mortality rates are described, the latter going up to 50%.1,2,10
A healthy 30-years-old pregnant woman presented to the delivery department at 40+2weeks of gestation with premature membrane rupture, following an uneventful pregnancy with regular scans and, serologies. Rectal/vaginal Streptococcus agalactiae screening was negative. No history of invasive fetal procedures or, trauma during pregnancy were described. No history of known hematological diseases in the family. She was placed on continuous FHR monitoring and, labor was induced with jugal misoprostol. After 12-hours of ruptured membranes, due to the increase of inflammatory parameters, empiric antibiotherapy with intravenous ampicillin was started. There was no fever during the labor. The Bishop score had changed and, the labor induction was continued with intravenous oxytocin. Approximately two-hours later, the FHR showed some fetal variable decelerations, ending in sustained fetal bradycardia (Figure 1).
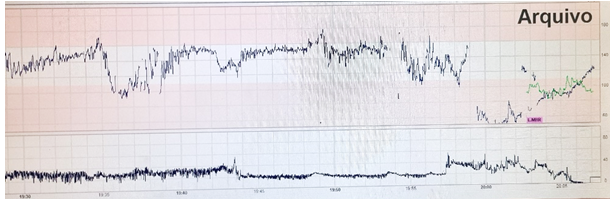
Figure 1 Fetal heart rate tracing, with fetal variable decelerations, ending in sustained fetal bradycardia.
Emergency C-section was performed due to acute fetal distress. A male infant was born with Apgar scores of 8/9/9, stimulation and, brief intermittent positive pressure ventilation was needed. The umbilical cord had normal vessels but presented a black-reddish and nontender swelling until placental insertion and, slightly stump bleeding (Figures 2–3). No major morphological placenta changes had been observed. Somatometry was adequate to gestational age and, physical examination was otherwise unremarkable. Vitamin-K intramuscular was given.
Minutes after delivery, he got pallor, moaning and, tachypneic. Venous gasimetria revealed a metabolic acidosis (pH 6.9) with hyperlacticaemia (10 mmol/L). He was admitted to the neonatal intermediate care unit for observation. Due to infectious risk, intravenous antibiotics with ampicillin and, gentamicin were started. Blood analysis revealed anemia (minimum value at 12-hours-of-live: 11,2 g/dL) without criteria for transfusion and, a normal hemostasis. After two-hours, the umbilical cord still had a slight bleeding, whereby an additional vitamin-K intramuscular was given, with resolution. The newborn did not require respiratory or, hemodynamic support. Normal abdominal and cranial ultrasound and, chest X-ray were performed. Neurological examination was normal and, there was a favorable evolution with supportive therapy.
He completed five-days antibiotherapy (negative septic scan and, negative hemoculture). He was discharged after five-days. Anatomopathological examination of placenta revealed congestion of the chorionic plate vessels and focal intervillous hematoma and, an umbilical cord with an extensive hematoma with perivascular hemorrhage and, parietal dissection. Umbilical cord stump evolved to mummification and, had fallen at 15-days-of-live without specific treatment. Clinical and, analytical follow-up at one and three months were normal and, at 12 months he presented a normal neurodevelopment.
Although most of the literature includes cases with poor outcomes, with higher rates of morbimortality being reported, our case demonstrates an eventful event. The majority of these situations is an unexpected finding, but a good outcome is possible, requiring, however, a high level of suspicion on the diagnosis, especially in fetus with unexplained cardiotocography anomalies.11 This case represents an uncommon etiology of acute fetal distress, highlighted by the decreased FHR. It appears to have been a spontaneous cord umbilical hematoma, once no risk factors were detected. The big hematomas are usually associated with neurological consequences,6,12 however our infant had a normal neurodevelopment until 12 months of follow-up. The early diagnosis and immediate medical and, surgical interventions were determinant for the good prognosis.
Awards and presentations: Clinical case presented as a poster at the “VIII Jornadas de Pediatria”, 1st April 2022, Vila Franca de Xira, Portugal.
Authors’ contributions
Ana Cristóvão Ferreira, Inês Pereira Soares and Sara Sousa were responsible for data collection, data analysis and, manuscript writing.
Patrícia Ferreira and Daniela Ramos were responsible for manuscript revision.
The authors declare that there is no conflict of interests.
There were no external funding sources for the realisation of this paper.

©2023 Ferreira, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.