International Journal of
eISSN: 2574-9889


Mini Review Volume 2 Issue 6
Department of Obstetrics and Gynecology, Grant Medical Foundation, India
Correspondence: Laxmichaya D Sawant, Department of Obstetrics and Gynecology, Grant Medical Foundation, Ruby Hall Clinic, Pune, MS, India
Received: May 29, 2017 | Published: October 23, 2017
Citation: Sawant LD. Sexually transmitted infections in pregnancy. Int J Pregn & Chi Birth. 2017;2(6):179-181. DOI: 10.15406/ipcb.2017.02.00044
Sexually transmitted infections (STIs) have increased by many folds across all age groups. During pregnancy STIs are associated with increased morbidity and mortality in infant. In some way, this can be described as a health crisis in reproductive and sexual health of women, which constitute as a public health emergency worldwide. A women patient diagnose with one STI is at higher risk for other STIs and so antenatal screening for all STIs including HIV testing is required during the antenatal visit. Pregnant women with STIs should receive comprehensive intervention that includes counselling and behavioral therapy, early notification to the partner and screening, advice on safe sex practices, along with management plan to treat the disease and reduce the risk of potential life threatening complication to the fetus and improve the outcome of the pregnancy. This article presents a brief overview of scope of STIs in pregnant women and its effect on overall women’s health and on their pregnancy along with comprehensive interventional strategy against STIs.
Keywords: STIS, HIV, syphilis, gonorrhea, chlamydia, trichomoniasis, HSV
Sexually transmitted infections (STIs) or sexually transmitted diseases (STDs) are spread primarily through sexual activity, but can also be transmitted through non-sexual means through exposure to blood or blood-related products, needle sharing, and via vertical transmission from mother to child during pregnancy and childbirth. STIs include several pathogens such as bacteria, viruses, and parasites, and out of all, eight pathogens have very high incidence rate. Currently, of these eight infections, syphilis, gonorrhea, chlamydia, and trichomoniasis are curable and the other four are viral infections that 2 include hepatitis B, herpes simplex virus (HSV), human immunodeficiency virus (HIV), and human papillomavirus (HPV).1-5 These viral infections are incurable but their symptoms or the disease process can be curtailed or altered through therapeutic intervention. Another infection which does not get categorized under STIs is bacterial vaginosis (BV), but it is very common in sexually active women. BV is a condition where normal vaginal flora gets altered to pathogenic bacteria leading vaginal discharge.
Majority of women with BV are asymptomatic, but during pregnancy there is increased risk of preterm delivery and postpartum endometritis associated with BV.3-5 The general symptomatology seen in women with STIs are vaginal discharge, urethral discharge, genital ulcers, and abdominal pain, however STI can be present without having apparent symptoms of disease. STIs can cause more serious complications in women such as pelvic inflammatory disease (PID) and infertility.
Almost all the STIs can increase the risk to HIV, but syphilis and HSV can raises the possibility of HIV acquisition by three times. Moreover, in women, STIs are also predominantly associated with PID and infertility with gonorrhea and Chlamydia constituting the main etiological pathogen in these disease processes. During pregnancy, the presence of STIs determines adverse pregnancy outcome such as spontaneous abortion, stillbirth, prematurity, intrauterine growth restriction (IUGR) with low birth weight (LBW), postpartum endometritis, and serious complications in newborn including congenital deformities. It has also been reported that the pregnant women, who are diagnosed with STIs and/or their complications, demonstrate high rate of pregnancy termination.1-5
The association between STIs and having pregnancy is very close due to its inherent need to have unprotected vaginal sexual contact. Also, during pregnancy the physiological changes altering normal flora of genitourinary tract should make the pregnant women more prone to STIs. Furthermore, therapeutic intervention during pregnancy would be a very complex process to carry out, since the pharmacological drug must be proven on both the aspect of being highly efficacious but safe on pregnancy with no potential health hazard to the maternal and fetal wellbeing. And therefore, during pregnancy women need to reassure that prompt and proper care and treatment of STIs can deliver favorable outcome of pregnancy.4,5
Sexually transmitted infections (STIs) are increased by alarming rate among all age groups resulting in increased infant morbidity and mortality during pregnancy. This constitutes a sexual health crisis across all age group and gender leading to a pressing health care issue and a public health emergency worldwide. The prevalence of STIs is higher not in the general population but also in pregnant women. Predominantly population under 25 years is highest demographic group to be prone for of STIs, but in general this increase rate relates to all age groups. According to World Health Organization (WHO) statistical data, it is estimated that worldwide more than 1 million of people get infected with STIs every day. Approximate yearly estimates for population infecting from chlamydia is 131 million, gonorrhea is 78 million, syphilis is 5.6 million and trichomoniasis is 143 million, that counts for a total of 357 million new infections per year. Furthermore every year genital HSV infection has been diagnosed in 500 million people and HPV infection in women alone accounts for 290 million. In 2012, close to 900,000 women were diagnosed with syphilis during their pregnancy, which resulted in approximately 350,000 adverse birth outcomes including spontaneous abortion and stillbirth. HIV has become the most prevalent STI in pregnant women with approximately 15-30% of women visiting antenatal clinics are diagnosed with HIV infection. The prevalence rate of BV among the pregnant women is reported to be around 12-15%. Moreover, every year HPV infection is associated with significant number of cervical cancer patients (528,000) and nearly half of those numbers in deaths from cervical cancer (266,000) worldwide. Therefore, STIs is major public health concern worldwide having a more profound impact on women’s health including physical, psychological, sexual, and reproductive health. And the consequences of STIs on over all women’ health goes beyond the specific effect of the infection alone.1-5
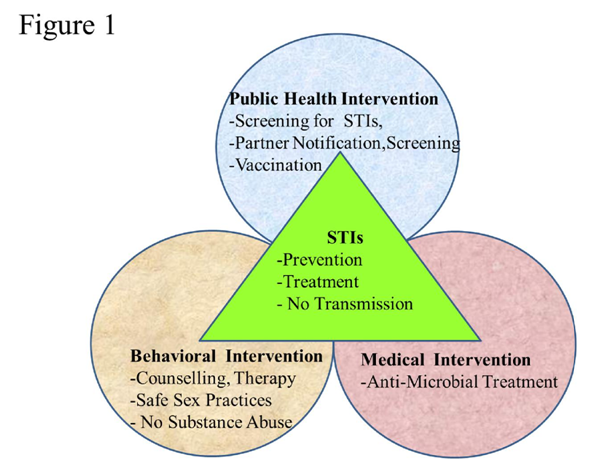
The optimal management for any person diagnosed with STIs should include comprehensive interventional strategy with three important components (Figure 1). The first component is of public health intervention constituting of screening for other STIs and HIV with follow-up repeat screening, early notification to the partner and screening. The second approach will be behavioral intervention constituting counselling and behavioral therapy including safe sex practices. The third component of this comprehensive strategy is therapeutic intervention constituting anti-microbial treatment not only for eradicating the disease process and reducing the risk of complications but also from public health perspective to halt the spread of infection in population.1-5 The primary prevention against STIs is via counselling and behavioral therapy. Such interventional program should include incorporating sex education in regular school and college curriculum with focus on comprehensive education on sexuality that is target towards teenage population. The counselling should also include safe sex practices such as correct use of condoms, reduction in risk taking behavior including substance abuse, along with counselling before and after screening test for STIs. The substance abuse such as alcohol, tobacco, marijuana, cocaine, and various other illicit drugs have been reported to be closely associated with teenage pregnancy and unplanned pregnancy with higher rate of STIs. The public health interventional program will also include providing vaccination to the target population against HPV and Hepatitis B virus. This approach can prevent long term complications of these infections such as gynecological malignancy. However, more biomedical and translational research needs to be done in future to develop safe and effective vaccines against other STIs.1-7
Apart from adolescents, the other key demographic groups will be sex workers, drug abusers, and men indulging in homosexual behavior. Furthermore, this interventional program which includes counselling and educational activity can empower target population with more awareness, knowledge and ability to understand the consequences of getting diagnosed with STIs. Moreover, the people who were subjected to this educational based behavioral therapy and counselling were more responsive to identify the sign and symptoms of different STIs. They were also very keen to get medical help for them and for their sexual partners as well. However, to undergo behavioral change through intervention is a very difficult step to archive. Therefore efforts needs to be taken to develop more effective behavioral therapy targeted towards specific demographic group. This can be done through fostering partnership between the target population and different expert groups such as health care professionals, public health specialists and social workers. Such partnership between target groups and health experts will allow target groups to participate in formulating strategy, application, and assessment of newer intervention based approach against STIs. Therefore, prevention of STIs should be prioritize with importance on increased awareness among the general population, eradicating stigmatization of STIs, vaccination to the target groups, appropriate training of medical professionals, and promoting use of condoms for safe sex practices to enable healthy sexual and reproductive life.1-5
In summary, across all countries there is an increase in prevalence rate among all age groups in STIs constituting a global health concern. In pregnancy this health care concern increases by many folds due to its risk to the developing fetus ranging from spontaneous abortion, preterm delivery, low birth weight, to congenital anomalies and stillbirth. Therefore, the best interventional strategy to manage any pregnant women diagnosed with STIs should be an all-inclusive approach with screening for other STIs including HIV, partner notification, and follow-up repeat screening, along with counselling and behavioral therapy including safe sex practices, and finally therapeutic anti-microbial treatment for good prognosis in pregnancy.1-5
None.
The author has no conflict of interest to disclose.

©2017 Sawant. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.