International Journal of
eISSN: 2574-9889


Case Report Volume 4 Issue 1
1Department of Radiology, Fattouma Bourguiba University Hospital, Tunisia
2Department of Radiology, Fattouma Bourguiba University Hospital, Tunisia
3Department of Gynecology Obstetric, Tahar Sfar University Hospital, Tunisia
4Department of Neonatology, Fattouma Bourguiba University Hospital, Tunisia
5Department of Gynecology Obstetric, Fattouma Bourguiba University Hospital, Tunisia
Correspondence: El Mhabrech Houda, Department of Radiology, Maternal and Fetal Unit, Fattouma Bourguiba Hospital, Monastir, Tunisia, Tel 216 25051354
Received: November 08, 2017 | Published: January 18, 2018
Citation: Mhabrech HE, Zrig A, Bouchahda H, et al. Second trimester diagnosis of diastematomyelia: US, CT and MRI features. Int J Pregn & Chi Birth. 2018;4(1):29-31. DOI: 10.15406/ipcb.2018.04.00078
Diastematomyelia is a rare spinal malformation characterized by a sagittal division of the spinal cord. Prenatal diagnosis of this malformation is possible by ultrasound, MRI and CT. In this report we describe a case of fetal diastematomyelia assessed by 2D and 3D ultrasound, MRI, CT scan and X-Ray.
Keywords: diastematomyelia, MRI, x-ray, t2w
Diastematomyelia is rare form of spinal dysraphism characterized by a sagittal cleft in the spinal cord.1 It may be isolated or associated with segmental anomalies of the vertebral bodies.2 Prenatal diagnosis of this malformation is possible by ultrasound, MRI and CT. A case of fœtal diastematomyelia is presented, demonstrating the sonographic, MRI, CT and X-Ray features diagnostic of this condition.
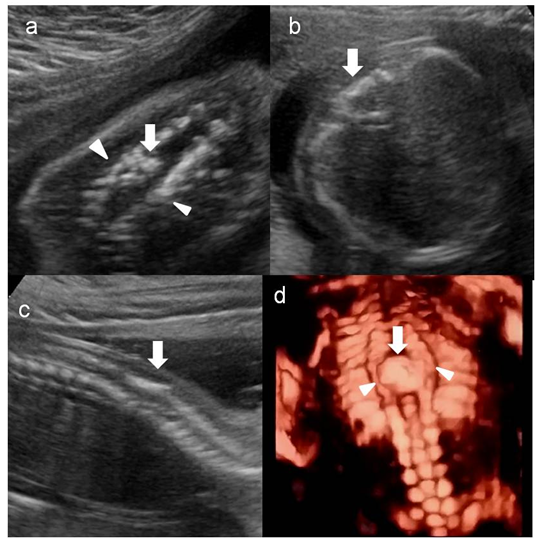
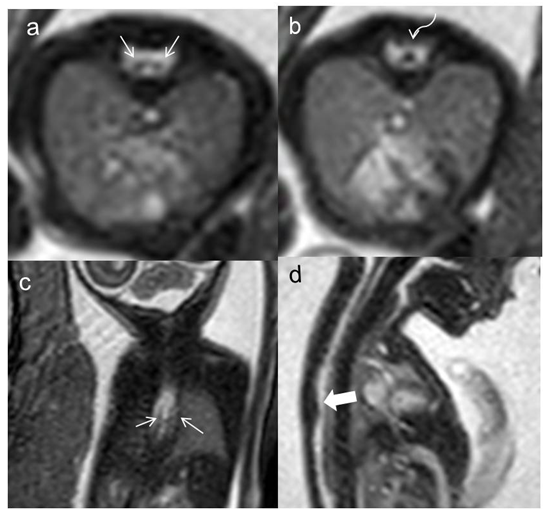
A 26-year-old primigravida presented to the ultrasound unit at 21weeks of spontaneous gestation for routine screening. 2D and 3D Ultrasound examination using Esaote (MyLabSIX) machine equipped with 7 and 10MHz probes detected widening of the spinal canal in coronal section and additional echogenic focus in the widened portion of the vertebral column in axial, coronal and sagittal section with intact skin and soft tissues overlying the affected spinal segment (Figures 1A-1D). The spinal cord was obscured by to acoustic shadowing. We performed fetal MRI two days later. Images were obtained in three orthogonal planes by using fast spin-echo T2 weighted images (T2W) images with 3mm slices thickness. This confirmed the abnormality, showing low signal bony spur in T2W sagittal and coronal images separating two hemicords within a single thecal sac. Both hemicords are of similar size and they are not separated by a midline sagittal septum. In the lower vertebral segments below the bony spur level, the two hemicords fused into one cord (Figure 1E-1H). There were no spinal cord tethering nor other spinal malformations. There was no evidence of additional brain anomalies. With regards to the limitation of the fetal spine evaluation in MR, an informed consent for fetal low-dose CT scan is obtained. The CT scan showed a midline thin bony septum splitting the spinal canal connecting the anterior and posterior vertebral archs in the axial plane with incomplete median sagittal partition of thoracic spine extending from T6 down to T10 level (Figure 1I, Figure 1K & Figure 1l). These findings confirmed the diagnosis of type I diastematomyelia.
The parents were supported and counseled regarding the prognosis of diastematomyelia and decided to terminate the pregnancy. A 610Grams male fetus has been extracted for medical reasons as per Tunisian termination of pregnancy law. In post-mortem examination of the fetus, the skin was normal in appearance in the dorsolumbar area. X-ray examination revealed marked local widening of the vertebral canal from T6 to T10 with partial sagittal partition (Figure 1M). Autopsy was not accepted by patient’s family because of their religious belief(Figures 1-4).
Diastematomyelia is a rare anomaly of the notochord, present in 6–36% of spinal dysraphism.3 It consists of splitting of the spinal cord into two hemicords. Each hemicord contains a central canal. The length of the separation is variable.
There are two types of diastematomyelia.1 In type I, each hemicord has its own thecal sac separated by an osseous or cartilaginous septum. Type II is characterized by single thecal sac containing two hemicords, usually separated by a fibrous septum. This malformation often occurs at the thoracolumbar regions. In our patient, the diastematomyelia was type I and was seen in the thoracic spine.
This entity can be isolated or associated with other segmental anomalies of the vertebral bodies or cutaneous signs.2 In our case, no cutaneous findings or other vertebral anomalies are accompanying diastematomyelia. Identification of an extra echogenic posterior focus in the spinal canal, using both 2D and 3D sonogram is considered as highly specific prenatal sign of diastematomyelia.4,5 MRI can assess the nature and length of the diastematomyelia and is more accurate to detect associated soft-tissue abnormalities. Axial and coronal T1W images are best for showing cord duplication but may not be helpful as CT for the bony anomalies. In some cases, MR is unable to detect the septum traversing the spinal canal as seen in our case. The distal cord and conus could not be well evaluated as they would be very thin.6 Fetal low dose CT could be performed particularly when parents are deciding to terminate the pregnancy.
Fetal low dose CT scans centered on the affected vertebrae can show, in coronal plan, a widening of the spinal canal similar to the one encountered in spina bifida7 and, in a transverse section, three instead of two posterior ossification centers; the posterior soft tissues could be assessed.8 Threedimensional CT reconstructions could be helpful in showing various vertebral segments anomalies such as spina bifida, kypho-scoliosis, partial sagittal partition, butterfly vertebra, hemivertebra, tripedicular vertebra, and butterfly vertebra4 as seen in our case. Prenatal knowledge of spinal cord anomalies is important for prenatal counseling in a multidisciplinary setting.
None.
Author declares that there is no conflict of interest.

©2018 Mhabrech, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.