International Journal of
eISSN: 2574-9889


Research Article Volume 5 Issue 1
1Department of Community Health, Faculty of Medicine, Universiti Kebangsaan Malaysia, Malaysia 2
2Department of Obstetrics and Gynecology, Faculty of Medicine, Universiti Kebangsaan Malaysia, Malaysia
3Department of Pediatrics, Faculty of Medicine, Universiti Kebangsaan Malaysia, Malaysia
Correspondence: Rosnah Sutan, Public Health Specialist (Family Health Group), Community Health Department, Medical Faculty, Universiti Kebangsaan Malaysia, Bandar Tun Razak Cheras, 56000 Kuala Lumpur, Malaysia, Tel 603-91455900
Received: January 08, 2019 | Published: January 28, 2019
Citation: Sutan R, Azmi NAM, Ahmad S, et al. Prevalence of normally formed macerated stillbirth and its contributing factors: a 7 years retrospective cross sectional study in a single hospital in Malaysia. Int J Pregn & Chi Birth. 2019;5(1):19-23. DOI: 10.15406/ipcb.2019.05.00141
From the public health’s perspective, there is a need to explore possible factors for antepartum stillbirth. Stillbirth rate acts as an important health indicator reflecting quality of antenatal care and delivery services. It acts as a direct indicator for the quality of maternal care and indirect indicator for socio economic and health behaviours outcomes. This indicator is essential for planning future programmes related to maternal health services. The study aims at assessing retrospectively the 7 years’ compilation of perinatal deaths occurred in a single teaching hospital in Malaysia. There were 44,994 births reported from the year 2004-2010 in sampled hospital and 453 cases were reported as perinatal mortality. According the Perinatal Stillbirths and Neonatal Deaths Rapid Reporting form (PNM1/97), a total of 283 were identified as stillbirth and 53.6% was classified as normally formed macerated stillbirth. From the analysis conducted of stillbirth cases, the normally formed macerated stillbirth is more prevalent in mothers from the group aged between 21-34 years, primip, having associated medical problems and among the Chinese. Majority of cases have a regular follow up of antenatal care and only 9.6% do not have regular follow up. In conclusion, stillbirth prevention is the best to be prevented before the mother become pregnant. The pre-pregnancy care services must be able to reach universally to all reproductive age group women for proper screening in order to identify risk and treat health problems before the mother become pregnant. Regular antenatal follow up is the best way to do foetal surveillance but both mother and care provider should optimise the visit with provision quality of care.
Keywords: stillbirths, normally formed macerated stillbirth, factors
Stillbirth is a circumstance that no pregnant women would want to experience. The causes of stillbirth are not fully known but some identified causes are shown preventable. Lack of in-depth knowledge on the risk factors of local stillbirth cases can help in reduction of the stillbirth rate if specific intervention related to the root problems are able to be implemented and monitored. Focussing on the reduction of mortality among children below 5 years old had resulted in positive accomplishments, in both developed and developing countries. Lately, many scientific papers discussed on the stillbirth issues.1–5 It has been reported that many efforts towards reducing the rate of stillbirth globally has been on going in the form of early detection using growth velocity measurement that customize to the mother’s factors especially on the targeted risk groups or implementing early preventive measures in hospital settings have yet to be materialized on its effectiveness.
It was estimated that the global stillbirth cases were 2.6 million in 20156 and majority (98%) of stillbirths occur in low and middle-income countries. It has been reported by many countries that each year the stillbirth rate has not shown a good declining rate. When compared to high income countries, the rate of stillbirths in low income countries is still high.7 Furthermore, many countries showed the stillbirth rate as plateauing and some showed inclination as reported by stillbirth group in Lancet Series.3 There was a regional variation reported in the estimated stillbirth rates which showed uncertain ranges and the proportion of intrapartum stillbirth for year 2015.3 The proportion of intrapartum birth to antepartum birth was higher in Southern Asia and sub Saharan Africa compared to other regions and these two regions had low percentages of stillbirths born in health facilities.3
In Malaysia, the perinatal death rate was reported dropped markedly from the year 1965 to 2013.7 The Malaysia health fact reported that the stillbirth rate was almost plateauing between 4.3-4.6 per 1000 livebirths from the year 2011 till year 2017 with fluctuation to 5.2 seen in year 2016 and reduced back to 4.5 per 1000 livebirth in year 2017.8 One of the contributing factors as the decrease in stillbirth rate in Malaysia was the improvement of healthcare services.7 Available report published on classification of perinatal deaths showed that the proportion of normally formed macerated stillbirth was the majority since the report published in 1998–2006.9
According to the World Health Report,10 the reduction of normally formed macerated stillbirth is a reflection of the effectiveness of antenatal services at the community level. The decline in rate of stillbirth is an important health indicator and study on this matter has yet to be conducted in Malaysia. The objective of this study is to identify the factors that lead to the occurrence of normally formed macerated stillbirth in the Universiti Kebangsaan Malaysia Medical Centre (UKMMC) as the selected resource centre for the research.
A retrospective cross-sectional study was conducted at Universiti Kebangsaan Malaysia Medical Centre (UKMMC), which is one of the public hospital in Malaysia that acts as one of the referral centre for specialist care under the Ministry of Education. It is situated in the urban setting population coverage within Kuala Lumpur. The sample of the data was obtained from the Department of Obstetrics and Gynaecology UKMMC who compiled and audited their perinatal deaths cases. The data was retrieved using the Perinatal Stillbirths and Neonatal Deaths Rapid Reporting form (PNM1/97), from a period of 2004 to 2010. Stillborn, as used in the Perinatal Mortality Report (PNM1/07), is classified as a foetal death occurred with the birth weight of at least 500g or when the gestational weeks has reached at least 22 weeks. Classification of stillborn and macerated stillbirth adopted in this study is based on a modified Wigglesworth pathophysiology.11 The normally formed macerated stillbirth is defined as, a foetal death with no obvious defects found at the time of death and antenatal in the womb, before labour start.
The descriptive analysis was presented as ratio and percentage of normally formed macerated stillbirth among the cases compiled within the study period. Comparison with other causes of perinatal deaths was made to identify the related factors.
According to the data which was obtained for seven years (2004-2010), 44,994 births was uses and there were 453 cases of perinatal mortality was reported. A total of 283 were identified as stillbirth cases, suggesting a stillbirth rate of 6.3 in 1,000 live births. The incidence of normally macerated stillbirth (n=149) was still the highest causes of perinatal mortality for the period of seven years. The present study found that the number of births were the highest among the Malays (24,734 births), followed by the Chinese. However, when the incidence rates of stillbirth were adjusted based on total births, the study found that the Chinese dominated the occurrence of stillbirths (6:39 per 1,000 births, n = 58); compared to the Malays (5.90 per 1,000 births, n = 146). The study also found that the normally formed macerated stillbirth mortality was higher among the Chinese (4:16 per 1,000 births) than the Malays (3.64 per 1,000 births). The distribution of normally formed macerated stillbirth incidence was found mainly among mother with the maternal age of 33 and 38 weeks of gestation on the third trimester of pregnancy. The trend of stillbirth was seen to decline beyond 39 weeks of gestation. Figure 1 shows several antenatal complications found among mothers who experienced a stillbirth. Based on present study, a history of vaginal bleeding was the most frequent antenatal complication found among mothers who experienced normally formed macerated stillbirth, followed by high blood pressure (34.8%).
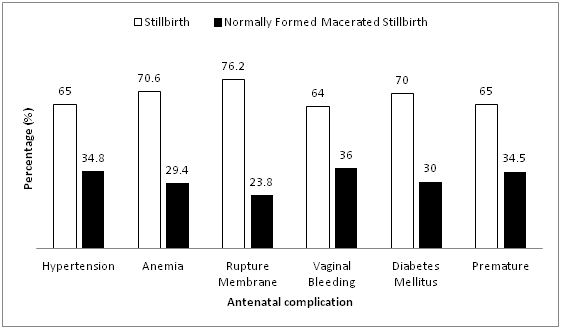
Figure 2 shows a total of 46 cases of stillbirth, with term babies. About 41.3% (n=19) stillbirth cases were classified as normally macerated stillbirth. Overall, the majority of the normally formed macerated stillbirths were among the term babies and primigravida. The results also show that, among mothers with term pregnancies, 97.8% of them had received scheduled antenatal services and nearly all of them did not experience any complications during pregnancy. The highest percentage of term babies suffering from normally formed macerated stillbirth was usually among women aged 21-34 years, with the median at 26 years old and mean at 34 years old.
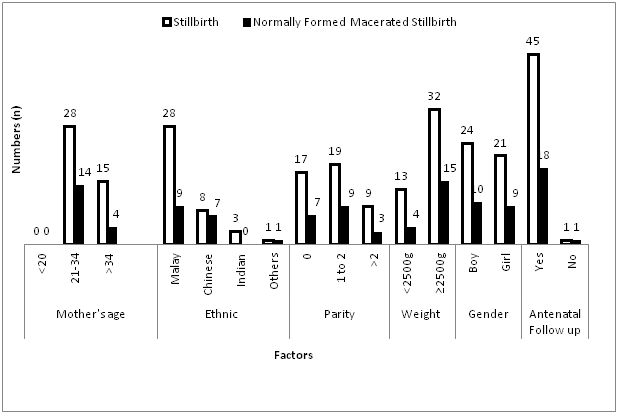
Table 1 shows the comparison between normally formed macerated stillbirth (antepartum) and intrapartum stillbirth. It was found that low parity, previous history of abortion, lower gestational week at delivery of stillbirth, no antenatal follow up and low birth weight are more prevalent in normally formed macerated stillbirth (antepartum) compared to intrapartum deaths.
Item |
Antepartum normally formed macerated stillbirth, n (%) |
Intrapartum stillbirth |
Mother’s Age |
median age 28.8 years |
median age 31.2 years |
Ethnic |
||
Malay |
90(72.0) |
239(72.6) |
Other |
35(28.0) |
90(27.4) |
Parity |
||
0-2 |
128(86.5) |
308(85.8) |
≥3 |
20(13.5) |
51(14.2) |
History of abortion |
||
0-2 |
146(98.6) |
344(95.8) |
≥3 |
2(1.4) |
15(4.2) |
Gestation age (weeks) |
median gestation 27.3 |
median gestation 29.5 |
Antenatal follow up |
||
No |
13(8.8) |
22(6.1) |
Yes |
135(91.2) |
340(93.9) |
Babies weight |
||
<2500g |
120(84.5) |
288(80.0) |
≥2500g |
22(15.5) |
72(20.0) |
Babies gender |
||
Boy |
87(60.0) |
206(58.7) |
Girl |
58(40.0) |
145(41.3) |
Table 1 Comparison between the risk factors of normally formed macerated stillbirth
Table 2 shows some factors assessed in the perinatal mortality reporting form. The normally formed macerated stillbirth has less prevalent in receiving antenatal care as compared to intrapartum death. The intrapartum stillbirth is more prevalent if the mother has associated medical condition like hypertension, Anaemia, Diabetes Mellitus and the obstetric problems like ruptured membrane and vaginal bleeding.
Criteria |
Category |
|
|---|---|---|
Normally Formed Macerated Stillbirth (Antepartum) |
Intrapartum stillbirth |
|
Received antenatal service |
135(28.4) |
340(71.6) |
Hypertension |
24(35.3) |
44(64.7) |
Anaemia |
5(29.4) |
12(70.6) |
Ruptured Membrane |
5(14.3) |
30(85.7) |
Vaginal Bleeding |
9(36) |
16(64) |
Diabetes Mellitus |
9(27.3) |
24(72.7) |
Table 2 Normally formed macerated stillbirth and intrapartum stillbirth by prenatal complication
From the result of this study, stillbirth rate at Universiti Kebangsaan Malaysia Medical Centre stood at 6.3 for every 1,000 livebirths for the study period. This figure is considered as high when compared to Malaysia’s stillbirth rate for year 2017 (4.5 per 1,000 live births). As the UKMMC is a referral centre, it is expected to receive high number of stillbirth cases referrals. UKMMC is a referral medical centre where most cases were referred and came from other various areas and locations. There were instances where the referred cases involved mothers suffering from current medical illnesses and antenatal complications. Although most referral hospitals are sufficiently equipped with facilities and expertise, in cases of stillbirth, the situation is difficult since there is no specific treatment to be given other than to investigate into the cause of death. Several cross-sectional studies in referral hospitals in other developing countries also produced similar results. Harare Maternity Hospital, the largest referral hospital in Zimbabwe discovered a stillbirth rate of 56 over 1000 live births in a one-year retrospective cross-sectional study it conducted as compared to the overall stillbirth rate in the country which was only 26 per 1000 live births for the same year.12
Antenatal services
The descriptive assessment of present study found an opposite result of existing literature findings. Attended scheduled antenatal clinic visits should able to screen and have early risk detection. However, this require quality of care and good tools to identify the risk. Observing mothers’ health status, placental factors and foetal factors, it is crucial to consider evaluating the risk assessment checklist during the antenatal visit. Mothers who attended the public clinic have carried a homebased antenatal card in Malaysia for foetal surveillance. The mother can have access to any other types of health facilities like private health facilities and hospitals for further check-up. Proper assessment of foetal growth measurement, maternal weight gain recorded, scan evaluation, foetal kick chart monitoring for 3rd trimester, fundal height measurement has been suggested in many studies. However, it requires an effort of standardised measurement and proper interpretation and management plan when the risk of stillbirth is identified as it may end up delivering a premature baby, an underweight baby and choosing safer method of delivery is crucial.
Antenatal services are not the major solution for the problems of stillbirth especially in normally formed macerated stillbirth. Based on a more detailed study, this problem can be solved if the service covers an optimal antenatal visits,13 and the type and the quality of services provided by each visit.2,6 According to the Ministry of Health Malaysia Report, almost all pregnant citizens received antenatal care services. This was shown in the attendance percentage of pregnant mothers which was 97.5% received minimum of 4 visits,14 in accordance with the recommendations of the World Health Organization,15 which outlined a minimum of four antenatal visits for mothers who did not experience any complications during pregnancy. Present study has shown that 90.6 % of the total rate of normally formed macerated stillbirth had attended the antenatal services during the pregnancy. Out of that number, only 14.6% were from full-term gestation who did not have antenatal follow up. Majority had duly received antenatal services during pregnancy (97.8%).
Indeed, the frequency of antenatal attendances influenced the effectiveness of foetus care during pregnancy. A study conducted among the pregnant mothers16 reported that the pregnant mothers were still not satisfied and considered the duration between each antenatal service was much too long, even for mild cases. It has been suggested to take into consideration of the patient perception, needs and experience in improving the flow of required antenatal screening and follow up.
The effectiveness of an antenatal service is not only measured in the attendance of pregnant women to the unit, but also in the quality of service rendered. A survey conducted in UKMMC assessing the antenatal service satisfaction survey noted that, nearly 52.6 % of pregnant mothers who came to the clinic expected the doctors to be more friendly and approachable and 62% would like to receive clarification on matters relating to their pregnancy.17 More frequent monitoring should be made during pregnancy through antenatal services, especially when they reached the third trimester. The patient also required answers to their questions, as well as a thorough examination and clear explanation such as about the baby kick charts, inspection and performing scanning onto the baby. Several essential laboratory tests should be performed, especially in cases of suspected hypertension and diabetes.
Mother’s age
Present study shows the majority (60%) of the normally formed macerated stillbirth occurred among women aged between 21 and 34 years. Even though this age group is considered as non-high risk, the findings proved that this group still exposed to the risk of normally formed macerated stillbirth. However, many studies have found that the opposite extreme age group is more risky.3,18,19 In Malaysia, women involved in employment sector as early as 18 years old and age of 21-34 is at the beginning of their career pathway. As a worker, changing life from a student to a worker, from a child to a couple looking after family, meeting living expenses needs in urban setting population would lead people to stress. It has been reported that working women are exposed to the risk of miscarriages, defects, stillbirths, infant’s weight and premature babies.20–22 The data obtained from this study however, did not supply the occupational information. Thus types of occupation can be considered as one of the factors that may contribute to an increased incidence of stillbirths among this group of women. The lack of time to undergo prenatal screening due to busy work schedule resulted in the lack of attention to the unborn child as well as to any pregnancy complications. This could also be the cause of antepartum death.
Gestational age
Normally formed macerated stillbirth was reported more prevalent at early 3rd trimester and intrapartum stillbirth is more prominent at late 3rd trimester. This is consistent with the results obtained from most studies.22,23 The improvement of medical facilities and expertise also allow high-risk cases to be identified earlier. Problems dealt at earlier stage for foetal identified with expected low birth weight, or with signs of intrauterine retardation, and mothers with high risk such as hypertension and diabetes may need to go through induced delivery. Although the rate of stillbirth is reduced as the gestation reaches the mature phase, such reduction should have also been achieved in normally formed macerated stillbirth as baby monitoring is usually increased during the third trimester. Antenatal visit at this point is conducted weekly until the day of labour, thus allowing the identification of a case in advance. However, when risk factors for induced birth or surgery are not detected, the pregnancy will prevail. Therefore, normally macerated stillbirth still occurs.
Ethnicity
According to the published Report of Perinatal and Neonatal Death,24 Indians had the second highest percentage of normally formed macerated stillbirth, and the Chinese had the lowest percentage. However, based on the results obtained from this study, the Chinese are the highest contributor to the normally formed macerated stillbirth. This could be explained by the population served by the UKMMC is covering the urban setting area that highly populated to Chinese and Malays. In Malaysia, there has yet to be any in-depth study over ethnicity particularly in relation with pregnancy and the factors that affected it.
Birth weight
Normally formed macerated stillbirth rate among full-term infants is a condition that should not occur, since the rate of survival of life among these babies is high. This study found that 50% incidences of normally formed macerated stillbirth among full-term infants were from infants with weight more than 2500g. A study among Asian babies predicted life survival rates for infants with weight 1500g to 2499g increased up to 99% 25. The ability to identify high risk mothers should start at the beginning or before the pregnancy, thereby increasing awareness should be emphasized until the pregnancy reached maturity. Among the factors that can be identified are accompanying existing diseases like diabetes, hypertension, thyroid disease, and blood-related diseases such as lupus, thrombophilia and blood group problem26. Factors that can be altered such as obesity and smoking habit should be addressed by educating the mothers with a more appropriate lifestyle intervention pattern.
The actual cause of normally formed macerated stillbirth for each individual is in fact, not yet known. This is because usually, a comprehensive investigation has not been made, and could not be done. Several investigations need to performed onto stillbirth cases, which include amniocentesis, serology for Rubella, Syphilis, Cytomegalovirus and Toxoplasma, full blood test including blood group, liver function and kidney function test including uric acid, anticardiolipin, and lupus factor; and vaginal swabs for bacteria culturization.25,26 New mothers experiencing stillbirth should be advised to space their pregnancy until the investigation is complete. Apart from letting their body recover, the investigation onto normally formed macerated stillbirth incidents could be done in a more thorough manner and would be able to prevent future similar occurrence.
Exploring possible contribution to the occurrence of normally formed macerated stillbirth, particularly at the end of their pregnancies should be handled and compiled for rectifying possible solution and planning. Strengthening pre pregnancy care clinic to identify those with medical or health problem s and treated before they plan for their pregnancies. Attended scheduled antenatal care and comply to health education given, early identification and refer appropriately to specific management team should be emphasised. Monitoring and evaluation of foetal surveillance should be emphasized on both care provider who deliver the management and to the mother to monitor the baby kick chart, healthy life style and avoid stress during pregnancy.
Limitation of the study
The present study using data of perinatal auditing year 2004-2010. The generalization to current time and population may be of limited use.
This study has found several factors which are indirectly related to stillbirth occurrence especially normally formed macerated stillbirth, and these factors should be taken seriously to overcome these cases. Although the obtained data was not the exact data that can be used to identify the cause of normally formed macerated stillbirth accurately, the information obtained from these data could reflect the occurrence of stillbirth in general, and the factors associated with it. A more detailed study by reviewing the case notes of each stillbirth patient can be conducted in the future to examine the causes and risk factors. Hopefully, a more accurate data collection with a variety of variables can be examined from the use of the new format. It is also recommended that a report on stillbirth cases are recorded every year for every state in Malaysia based on PNM format. This report will enable the identification of cases in a more accurate way, not only in determining the contributing factors of each incident, but the audit and evaluation process can also be duly conducted. This kind of efforts are done in hopes of opening eyes of the general public, particularly those directly involved in dealing with perinatal mortality at the national level.
We would like to express our appreciation towards staffs of the Department of Obstetrics and Gynaecology UKMMC for their help as well as to the Ethical Committee of University Kebangsaan Malaysia for approving this study (UKM-CGPM-TKP-070-2010).
The author declares there are no conflicts of interest.

©2019 Sutan, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.