International Journal of
eISSN: 2574-9889


Short Communication Volume 10 Issue 1
1ASL Frosinone, Ospedale Santissima Trinità di Sora, Italy
2Università Roma Tor Vergata, Maternal Fetal Division, Italy
Correspondence: Juan Piazze, ASL Frosinone, Via Armando Fabi snc, FR 03100, Frosinone Lazio, Italy
Received: January 23, 2024 | Published: February 14, 2024
Citation: Juan P, Marta P, Cristina D, et al. Ovarian artery Doppler velocimetry effects after myoinositol and lipoic acid therapy in PCOs patients. Pregnancy & Child Birth. 2024;10(1):16-17. DOI: 10.15406/ipcb.2024.10.00303
Background: Polycistic ovary syndrome (PCOs) is one of the most common endocrine and metabolic disorders in premenopausal women. This is the second part of an extended report regarding the significant effects of the therapy based on an Alfa Lipoic Acid (ALA)/Myoinositol (Myo) combined drug on adnexal parameters, as assessed by ultrasound technique.
Methods: A prospective cohort trial. Data regarded thirty four italian nulliparous women considered for the study, control cases were chosen from an initial group of sixty-nine healthy women group paired by age and nulliparous status.
Patients underwent a Myoinositol plus ALA regimen twice a day in a continued fashion in a twenty four months period. Ultrasound examinations were coincident with the fifth day of menstrual period and were set as follows: Time 0 (first evaluation), Time 12 (after twelve months) and finally Time 24 (after 24 months).
Results: The mean age was 31.4 years old. Results regarding any significant change in the endometrial width, number of follicles, and the ovarian volumes within the time of the trial, showed no significant changes in the intervals considered. Conversely, the parameters dealing with color Doppler velocimetry waves of the ovarian arteries showed a significant decreasing trend, considering the first values and after 12 and 24 months.
Conclusions: Considering a consistent and significant decrease in ovarian arteries resistance, we may hypothesize that Inositol plus ALA therapy may block the vascular effects of hyperadrogenism, maybe playing a role in the anti oxidant and anti inflammatory pathways.
Keywords: PCOs, inositol, alfa lipoic acid, Doppler velocimetry
Polycistic ovary syndrome (PCOs) many times it is approached taking in consideration single symptoms of androgen excess and ovarian dysfunction in the absence of other specific diagnoses.1 Even genetic basis of PCOs has been discussed in recent bibliography.2,3 PCOs cases should be considered not as a single pathology. And this is the mistaken approach usually observed in the clinical practice. One hypertensive disorder or a Diabetes Mellitus may have established signs and symptoms and established blood analysis values and other tests. Conversely, the PCOs must be faced as a syndrome further than single dermatology alterations or a menstrual disorder. It must be considered as an incomplete equilibrium between male and female hormonal status, that is more complex than searching for an altered LH/FSH ratio or an established hyperinsulinism.
Considering what underlined before, we decided to analyze the eventual effects of Myoinositol (Myo) associated with Alfa Lipoic Acid (ALA) in our PCOs patients. Data was extensive and hard to be considered in a single report, so we decided to distribute it into two sections, 1) regarding the direct assessed parameters of ovarian blackblog, i.e., ovarian dimensions, number of follicles (4) and 2) regarding the effects on ovarian resistances, as assessed by ultrasound techniques. The present data describes the final report after a two years of a therapeutical paired prospective study.
Trial design and oversight: a prospective cohort trial. The study was performed from January 2019 until January 2021. Cases and controls selection: we selected women coming to our clinic, recruited under the following criteria: nulliparous women, women with a documented diagnosis of PCOs, women not using contraceptive or any kind of hormonal therapy and women not affected by other comorbidities. Only bilateral ovarian micropolicystic pattern patients were considered for the study. The research group: the trial was designed by two of the authors. All authors analyzed data, collaborated in the first draft of the report and participated in the decision of submitting the publication.
Participants: Trying to insert complete data, we excluded from the selection: pregnant women, lost to follow up women and women who initially accepted but afterwards refused to participate. After the above considerations from an initial sixty nine PCOs group, we selected thirty four PCOs italian nulliparous women that were considered for the data analysis. Cases were compared to data taken from a women control group paired by age and nulliparous status. The mean age was 31.4 years old. Patients underwent a Myoinositol (2000 mg) plus ALA (400 mg) regimen twice a day in a continued fashion in a twenty four months continuous period. Ultrasound examinations included ovarian arteries evaluation by means an endocavitarian high frequency probe (Siemens Elite NX 3) within a restricted color flow window, studying the resistance index for statistical analysis (Figure 1), ultrasound and clinical evaluations were coincident with the fifth day of menstrual period and were set as follows: Time 0 (first evaluation), Time 12 (after twelve months) and finally Time 24 (after 24 months). Ethical approval was obtained at the trial site after a decision of the operative ethical committee (CDA 0013_19) and all women accepted participation signing an individual written informed consent. Statistical analysis: Statistical data was analyzed by means of the Open Stat program (Softonic) and the Jamovi Project 2021 Statistical Software (version 1.6), based meanly in paired T test analysis.
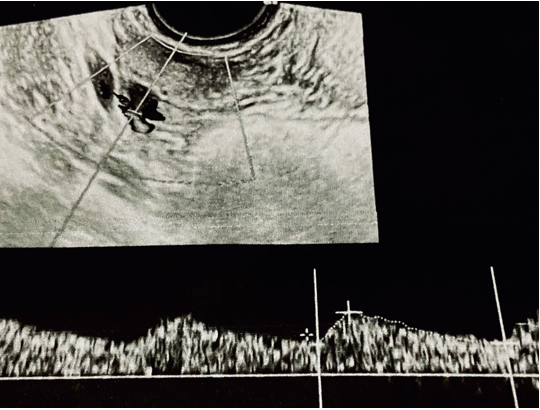
Figure 1 Ovarian artery color Doppler waveform assessed by endocavitarian probe, in the fifth day after starting menses.
COVID 19
The delay in the execution and conclusion of the trial, other than unexpected logistic difficulties, were explained by the COVID/19 waves and all the concerning events.
All participants were Caucasian italian women, with a mean age o 31.4 yrs (min 21,max 38), parity 0. Data regarding follicles, ovarian volume and endometrium were described in the first part of this trial.4 Regarding the Doppler velocimetry evaluation of ovarian arteries resistance indexes, a significant decreasing trend considering left and right ovarian resistances, was observed. Moreover, confirmed when mean values (left + right/ 2) were considered (Table 1).
Statistics |
P |
RI mean T0-RI mean T12 2.33 |
0.02 |
RI mean T0-RI mean T24 5.31 |
<0.001 |
RI mean T12-RI mean T24 2.98. |
0.004 |
~Friedman test. X2 20.4, df 2, p<0.001 |
|
Table 1 The repeated measures of the ovarian artery resistances mean show a decreasing trend in time. The Pairwise Comparisons depicts the differences between groups. The Friedman test represents the repeated non parametric ANOVA statistical probability
Ozay et al have found that the Myo therapy reduced ovarian vascularization after 3 months, and this decrease was specially noticeable in women with PCOs compared to healthy women.5 Regarding the action of the combination of Myo and ALA, the Italian Advisory Board in Polycistic Ovary Syndrome published a report from observations to clinical experiences on the use of Myo/ALA combinations to improve the pictures of the syndrome.6 The Myo/ALA combination in our trial has shown a significant effect on menstrual pelvic pain and in the regulation of menses rhythm, however no significant differences were found on volume and and antral follicles number between PCOs cases versus controls.4 It remains stated that treating PCOs with inositol derivates, improves the ovarian function and fertility, decreases the hyperandrogenism including acne and hirsutism, affecting positively metabolic aspects and various hormonal parameters.7–9 Many interesting studies have been published describing ovarian changes assessed by ultrasound technique. Pascual et al have conversely suggested that a 3D power Doppler angiography index may not be useful for discriminating between normal and PCOs ovaries.10 Mala et al in the 2008 concluded that 3D power Doppler indices were higher in women with PCOs than in control groups.11
In conclusion, we may hypothesize that Inositol may block the vascular effects of the hyperandrogenism, and that ALA in combination may play an important role dealing with anti inflammatory pathways. The Myo/ALA combination has shown in our trial a sustained and significant effect as stated by the decrease in the ovarian resistances.
We wish to express our highest gratitude and acknowledgment to the Centro Diagnostico Arce (Arce, Frosinone) for their unconditional support regarding material, schedule, trained personal and technical assistance. To the Laborest Laboratories (Uriach Italy Srl), who supported generously the whole therapy in order to guarantee the full compliancy of the whole study, and for their patience, sincere thankfulness.
And finally, a great thanks to all collaborators not mentioned, that permitted to go ahead nevertheless all the difficulties and technical and logistic problems due to COVID-19 pandemy.
There is no Conflicts of interest.
None.

©2024 Juan, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.