International Journal of
eISSN: 2574-9889


Research Article Volume 4 Issue 4
1NI Pirogov Russian National Research Medical University, Russia
2Clinical Hospital Lapino, Russia
3Perinatal Medical Center, Russia
Correspondence: Grigoryan Ashot M, chief of the Department of endovascular methods of investigation and treatment, Clinical Hospital Lapino, 143081, Moscow region, 1-st Uspenskoe highway, Lapino, 111, Russia, Tel 74955266060
Received: February 22, 2018 | Published: July 31, 2018
Citation: Kurtser MA, Grigoryan AM, Yu Breslav I, et al. Comparative characteristics of endovascular methods of stopping bleeding in placenta accrete. Int J Pregn & Chi Birth. 2018;4(4):195-200. DOI: 10.15406/ipcb.2018.04.00109
Introduction: Currently, relatively rare complications of the early twentieth century, placenta accretes was transformed into perhaps the most common obstetric pathology requiring removal of the uterus. In the modern development of endovascular surgery becomes possible to significantly reduce the blood loss during childbirth and to preserve fertility.
Material and methods: The paper presents the experience of using endovascular methods to reduce blood loss. Depending on the kind of care for endovascular patients were divided into two groups. The first group (n=38) consisted of patients whose delivery is accompanied by temporary balloon occlusion of the common iliac arteries on both sides, and the second group (n=59) – the patient underwent embolization of the uterine arteries.
Results: Patients in both groups the use of modern technology – temporary balloon occlusion of the common iliac arteries and embolization of the uterine arteries in conjunction with hardware reinfusion of autologous eritrotsity–allowed to perform organ-sparing surgery all patients. The average intraoperative blood loss in patients of group I amounted to 1642±1146 ml (27.5±22.0% BCC), 26.3% of patients recorded minimal blood loss (700ml). Complications of the postoperative period was observed in 2 (6.25%) patients – in one case there was thrombosis of the common femoral artery requiring thrombectomy and execution in one patient, massive blood loss (4000 ml), filled with large doses of fresh frozen plasma and donor red blood cell mass. In group II, the intraoperative blood loss averaged 1974±1445ml or 29.7±22.4% BCC, the volume of blood loss in one patient, demanded its transfer to the ventilation.
Conclusion: Temporary balloon occlusion of the common iliac arteries and uterine artery embolization are effective methods of reducing blood loss during delivery of patients with placenta accretа and uterine scar after cesarean section. With the availability of both techniques, preferably holding a temporary balloon occlusion, providing a significant reduction in blood loss volume.
It can be recommended for use in hospitals level III.
Keywords: placenta accretа, organ surgery, temporary balloon occlusion of the common iliac artery, embolisation, uterine artery
Placenta growth (placenta accreta) is currently defined at a frequency of 1:1,200 genera, and according to several authors is the cause of extirpation of the uterus in 38-64% of observations.1–3 Placenta accreta remains the leading cause of massive obstetric haemorrhage due to the inability to contract the thinned lower uterine segment. Contributes to bleeding and gestational reconstruction of the vessels of the myometrium, which turn into a non-muscle hollow tube. The volume of blood loss reaches 3000-5000 ml, and in some patients reaches 16000ml.4 For a long time hysterectomy was considered as an obligatory attribute in the delivery of patients with placenta accreta.5–10
Maximally reduce the arterial blood supply of the uterus can be by bandaging the main arteries of the pelvis or endovascularly. An invaluable contribution to the reduction of intraoperative blood loss is caused by endovascular interventions: transcatheter embolization of uterine arteries (EMA), often used when placenta is left in situ; Temporary balloon occlusion of internal iliac, common iliac arteries or aorta, used both for hysterectomy and metroplasty. Selective EMA is an alternative to surgical hemostasis, and with placenta accreta is successful in 50-87% of patients.11,12 Failures are usually associated with a well-developed network of collaterals, as well as a discrepancy between the size of the emboli and the diameter of the vessel.13 For the first time, temporary balloon occlusion of internal iliac arteries with abnormal attachment of the placenta was described in 1997. J Dubois et al.12 Since then, many publications have dealt with efficiencies up to 90% and complications associated with the installation of cylinders in a. iliaca interna.14–16 However, dissatisfaction with an insufficient decrease in the volume of blood loss contributed to a change in endovascular tactics. In 2005, an attempt was made to inflate balloon catheters in the common iliac arteries, which made the operating field practically "dry"17 In the literature, information is extremely meager. In the available publications, temporary balloon occlusion a. iliaca communis was accompanied by extirpation of the uterus during cesarean section.18,19 Complications such as ischemic injury of the lower extremities due to thrombosis of the internal iliac or femoral artery in 15-16% of patients have been described.20 The lack of a single point of view on the preference for a particular type of endovascular aid in the growth of the placenta, a small number of articles devoted to the temporary occlusion of common iliac arteries on both sides, led to this study.21
Hypothesis
Temporary balloon occlusion of common iliac arteries on both sides in patients with placenta accreta and uterine scar after cesarean section is a more effective procedure compared with uterine artery embolization, allowing to significantly reduce the volume of blood loss, reduce postoperative and recovery periods.
Study design
The criteria for inclusion of patients in the study were: 1) gestation period ≥28 weeks; 2) pregnant women with a scar on the uterus after the previous operation of caesarean section; 3) placenta previa on the anterior wall of the uterus and in the region of the cicatrix; The study did not include patients with a gestation period of less than 28 weeks; Pregnant women with placenta previa without previous operation of cesarean section.
All patients, depending on the type of endovascular intervention, were divided into two groups: group I-patients whose delivery was supplemented by temporary balloon occlusion of common iliac arteries on both sides (n=38), group II-patients who before selective embolization performed selective embolization of the uterine arteries (n=59). In both groups, blood loss, hemoglobin, erythrocyte, hematocrit before and 24 hours after surgery, postoperative bed-day, volume of autohemotransfusion, the volume of blood products required (fresh frozen plasma, donor erythrocyte mass) were estimated.
Clinical characteristics of patients
A retrospective examination of patients delivered at the Family Planning and Reproduction Center of the Moscow City Health Department, the Perinatal Medical Center in Moscow and the Lapino Clinical Hospital between 2009 and 2016 was carried out. All patients met the inclusion criteria. In all the observations, the diagnosis of placenta ingrowth was established by ultrasound examination, in which the following signs were observed: the presence of placental lacunae, the obliteration of the hypoechoic zone between the placenta and myometrium, the thinning of the myometrium less than 1 mm, the absence of a clear boundary between the uterine wall and the bladder. In order to clarify the diagnosis, magnetic resonance imaging was carried out, the pathognomonic signs of placenta accreta were aneurysm of the inferior uterine segment, thinning of the myometrium adjacent to the placenta, various vascular placental lacunaes, the presence of pathological vessels that extend beyond the organ. Despite the comparability of sensitivity (80-90%) and specificity (98%) of both diagnostic methods, preference is given to a more economical method-ultrasound diagnostics.23
Depending on the type of endovascular intervention, all patients were divided into 2 groups. The first group consisted of 38 patients, whose delivery was supplemented by temporary balloon occlusion of the common iliac arteries on both sides, and the second group consisted of 59 patients who underwent selective uterine artery embolization prior to removal of the placenta. Both groups were statistically comparable in age, weight, number of pregnancies, labor and scars on the uterus, gestation period, uterine aneurysm area (Table 1).
№ |
Parameter |
I group |
II group |
p |
1 |
Age (years) |
33.6±4.2 |
33.7±4.4 |
0.05 |
2 |
Weight (kg) |
74.3±9.8 |
76.5±11.5 |
0.05 |
3 |
The number of pregnancies |
4.4±2.2 |
4.1±1.9 |
0.05 |
4 |
The number of births |
3.1±1.7 |
2.7±1.0 |
0.05 |
5 |
Number of scars on the uterus |
1.7±0.8 |
1.5±0.6 |
0.05 |
6 |
The gestational age (weeks) |
35.5±2.5 |
36.8±1.8 |
0.05 |
7 |
Area of uterine aneurysm (сm²) |
274.4±173.8 |
196.1±106.2 |
0.05 |
Table 1 Comparative characteristics of patients in groups I and II
In patients of the first group, varicose veins were prominent among somatic diseases - in 9 (23.6%), chronic pyelonephritis-in 5 (13.1%), hereditary thrombophilia-in 1 (2.6%). Of the gynecological diseases, the subserous uterine fibroids were observed in 2 (5.2%) women, paraovarian cyst in 1 (2.6%). All pregnancies were spontaneous, of them 3 (7.9%) twins. All patients had a caesarean section in their history. The scar after one operation was in 17 (44.7%), after two operations-in 14 (36.8%), after three-in 5 (13.2%), after four - in 2 (5.3%). Artificial or spontaneous abortions in the history had 19 (50.0%) patients. In 1 (1.6%) patients of group II, autoimmune thyroiditis took place. Among gynecological diseases, uterine fibroids were observed in 2 (3.3%) patients. All pregnancies were spontaneous.The scar after one operation was in 32 (54.2%), after two operations - in 22 (37.3%), after three - in 5 (8.5%) of the examined. The gestation period at the time of delivery in patients of groups I and II is presented in Table 2.
|
Duration of gestation (weeks) |
I group |
% |
II group |
% |
1 |
< 34 week |
12 |
31.6 |
4 |
6.8 |
2 |
35–38 |
23 |
60.5 |
49 |
83.1 |
3 |
> 38 week |
3 |
7.9 |
6 |
10.1 |
|
Total |
38 |
100 |
59 |
100 |
Table 2 Duration of gestation of patients with placenta accreta
The majority of patients of groups I and II - 23 (60.5%) and 49 (83.1%) were delivered at 35-38 weeks.
In 8 (21.1%) women of group I, according to the results of MRI, it was impossible to exclude the involvement of the posterior wall of the bladder, which was intimately soldered to the thin lower segment of the uterus. In group II of such patients there were 4 (6.8%). Technique of endovascular operations. In the case of temporary balloon occlusion of the common iliac arteries, the endovascular stage is performed after the extraction of the child. According to the method of Seldinger, the puncture of the common femoral artery is performed from one side and the other, after which introducers are installed. The diameter of the introducer is chosen according to the diameter of the balloon catheter. In the abdominal aorta, diagnostic J-conductors of 0.035 "are placed and installed. Conductors conduct and install in the projection of the bifurcation of the abdominal aorta with the transition to the common iliac artery balloon-catheters Opta (Cordis), Admiral (Invatec). The diameter of the balloon catheter is selected in such a way that it does not exceed more than 1/3 the diameter of the total femoral artery, determined from the data of the duplex scan at early gestation. After positioning the balloon catheter, the latter is inflated with a syringe-manometer at a pressure of 6-8 atm. Through the lateral port of one of the inflated cylinders the conductor is temporarily removed and the contrast medium Omnipak or Nycomed is injected. The absence of a contrast agent distal to the balloon catheter indicates a reliable overlap of the artery lumen. After being convinced that the blood flow distal to the balloon catheter is absent, the conductor is again injected into the lateral port and installed in the abdominal aorta. Balloon catheters are fixed to the skin of the thigh to prevent their dislocation during manipulations to remove the placenta. During the midwifery phase with a 20-minute interval, the cylinders are alternately deflated for 30-40 seconds to restore blood flow to the common iliac arteries in the pelvic organs and lower limbs. After completion of the obstetric phase, balloon catheters are blown off, haemostasis is removed and performed.
Embolization of the uterine arteries also begins with a puncture according to the Seldinger method of the common femoral artery on the one hand. After the introduction of the introducer, selective catheterization of uterine arteries is performed sequentially from one side and the other side by a catheter such as Cobra (Cordis) or AUB (Terumo). After catheterization of the uterine arteries, particles of PVA (Cook) 510-700 mk are inserted into each of them. Control angiography demonstrates the absence of blood flow through the uterine arteries, followed by the obstetric phase. After extraction of the placenta, the introducer is removed and hemostasis is performed.
Statistics
Statistical processing of data was carried out using the SPSS for WindowsVersion 19.0 application package (IBM Corp.). The data are represented by the median and interquartile latitude - Me (P25; P75). The normality test was carried out using the Kolmogorov-Smirnov test. To evaluate the results of treatment in each group, the Wilcoxon sign criterion was used, to compare data between subgroups, the Mann-Whitney U test. Statistically significant differences were considered for p <0.05.24
Results of the study
When performing the delivery with endovascular support, all patients managed to perform an organ-preserving operation. Metroplasty, consisting in excision of altered tissue of the uterus with a pathologically attached placenta, was performed in all puerperas. In 8 (21.1%), a resection of the bladder was required because of the impossibility of its separation among the patients of group I and in 4 (6.8%) in group II.
Delivery was routinely performed in 29 (76.3%) women of the I group, while in 9 (23.4%), it was performed according to emergency indications caused by bleeding from the genital tract.
The bottom incision on the uterus during cesarean section was performed in 37 (97.3%) patients, corporal over the placenta-in 1 (2.7%).
All children were born in a satisfactory condition. The body weight ranged from 1200 to 3690 grams, an average of 2581±562grams. Fifteen (37.5%) of newborns were weighing from 1200 to 2500 grams, and 25 (62.5%) with a body weight of more than 2500 grams (2530 to 3690).Among the patients of Group II, 58 (98.3%) were surgically operated, in an emergency 1 (1.7%) maternity wards. All patients of group II underwent a bottom incision on the uterus. As in Group I, all children of Group II patients were born in a satisfactory condition. The body weight at birth was on average 3143±536 grams, ranging from 1300 to 4690 grams. With a body weight of up to 2500 grams. 8 (13.6%) children were born, and over 2500gr. -51 (86.4%) children. In the first group of patients, after the extraction of the fetus for the purpose of hemostasis, temporary balloon occlusion of the common iliac arteries on both sides was performed before metaplasty, and in the second group for this purpose embolization of the uterine arteries was performed on both sides. The effectiveness of endovascular support methods was assessed by: the level of blood loss (volume and percentage of circulating blood volume), changes in red blood before surgery and in the postoperative period (hemoglobin, erythrocyte, hematocrit), reinfusion volume of autologous eritrovissivities and infusion therapy (NWP use and donor erythrocytes). The volume and magnitude of blood loss for patients of both groups is presented in Table 3. For group 1 patients, the blood loss value ranged from 400 to 4800 ml, or 27.5±22.0% BCC, averaging 1642±1146ml. Have the majority of patients-29 (76.3%)-the blood loss value did not exceed 2000 ml (18 patients with blood loss to 1000ml and 11 from 1000 to 2000ml).
|
2016 Completed |
|
|
|
|
|
|
|---|---|---|---|---|---|---|---|
|
The volume of blood loss (ml) |
|
|
|
Total |
||
< 1000 |
1001–2000 |
2001–3000 |
3001–4000 |
4200–4800 |
> 4801 |
||
I group (number of pts) |
18 (47.4%) |
11 (28.9%) |
4 (10.5%) |
3 (7.9%) |
2 (5.3%) |
--- |
38 (100%) |
II group (number of pts) |
18 (30.5%) |
25 (30.5%) |
7 (11.8%) |
2 (3.4%) |
2 (3.4%) |
5 (3.4%) |
59 (100%) |
Table 3 The volume of blood loss in patients with placenta accretа
In group II, the blood loss volume averaged 1974±1445ml, or 29.7±22.4% BCC, varying from 400 to 6000ml. In this group, the number of patients with blood loss up to 2000 ml was 43 (72.9%), while, in contrast to group I, patients with blood loss from 1000 to 2000 ml prevailed (25.4%), while with blood loss to 1000ml was 18 (30.5%) of the patients. With the aim of replenishment of blood loss, hardware reinfusion of autoerithrocytes, transfusion of FFP and donor erythrocytes was carried out. In group I, the hardware reinfusion of the autologous erythrocyte suspension was performed in 37 (97.4%) of the puerperas. Among the patients who underwent hardware reinfusion, in 29 (78.4%) cases it was performed using one Cell Saver device, and in 8 cases by means of a combination of two devices - Cell Saver and CATS. An average of 1754±1660ml of blood was collected, reinfusion - 804±643ml. 26 (68.4%) patients needed transfusion therapy, 19 (73.1%) required transfusion of FFP in volume 1474± 556ml, and in 7 (26.9%) - erythrocyte mass in the volume of 1082±474ml. Among the patients of group II, the proportion of those who needed the hardware reinfusion of the autologous erythrocyte suspension was 91.5% (54 patients). All women used only one device - Cell Saver, through which an average of 1900±1304ml was collected, and the reinfusion volume was 1057±820ml. 39 (66.1%) patients needed transfusion of blood components: 33 (84.6%) cases, FFP transfusion in the volume averaged 1531±846ml, 6 (15.4%) - donor red blood cells in the volume of 600±176ml.
The change in red blood indices (hemoglobin, erythrocytes and hematocrit) for patients of both groups before and after the operation is shown in Figure 1. The hemoglobin level for patients of the I group at the preoperative period ranged from 76 to 130 g / l, averaging 104.5 (95.25 ; 115), and for patients of Group II 112 (107; 118) (it ranged from 53 to 141 g / l). In the postoperative period, this indicator was 91 (80.25, 101.25) for patients of Group I and 96 (87.5, 105.5) for patients of Group II, respectively. The erythrocyte index was 3.4 (3.29, 3.7) in the preoperative period in the preoperative period, ranging from 2.3 to 4.4 x 10x12, and for patients of Group II 3.8 (3.5, 4.01), ranging from 1.9 to 4.4 x 10 x 12. In the postoperative period, the level of erythrocytes for group I was 2.9 (2.6, 3.4), and for group II - 3.2 (2.7, 3.74). The level of hematocrit in the patients of the I group was 30.8 (27.5, 34.1)% (varied from 21 to 42%), while in the patients of the II group it was 32.7 (31.1, 34.9)%, varying from 18.5 to 44.6%). In the postoperative period, the hematocrit was 27.65 (23.1, 29.1) and 27.75 (25.13, 29.6), respectively, for patients of groups I and II.
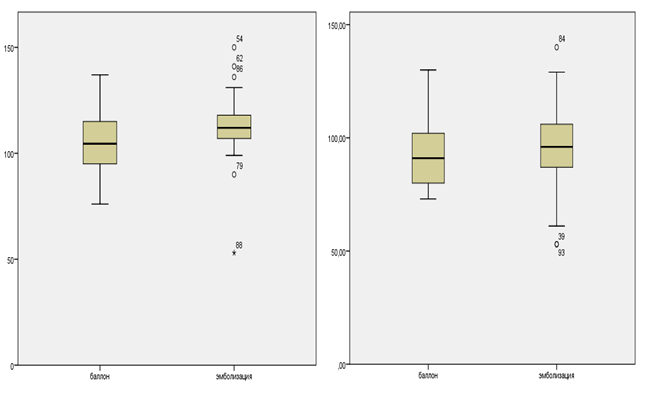
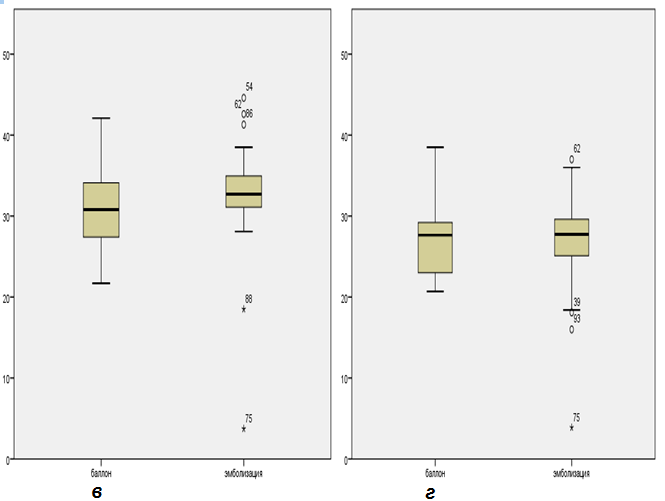
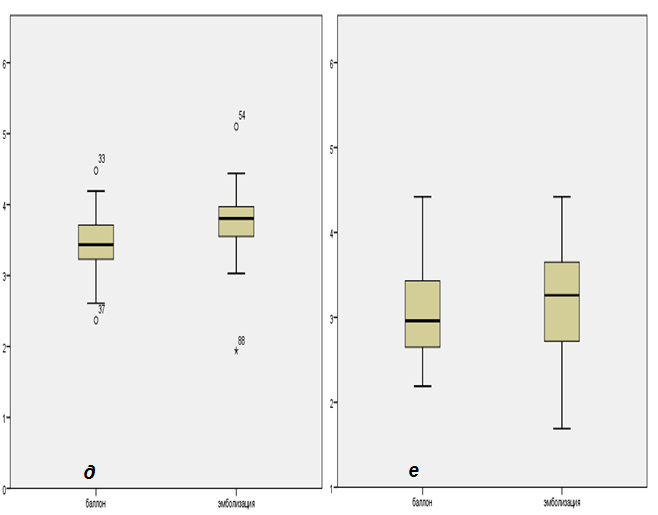
Figure 1 Change in hemoglobin (a, b), hematocrit (c, d) and erythrocyte (e, e) in both groups before and after the intervention.
The duration of surgical intervention for Group I patients was 161.5 [128.7;200], and for Group II-175 [145;218.7] min (Figure 2). The duration of the postoperative period was comparable in patients of groups I and II and was 9 [7;11] days for patients of Group I and 9 [8; 11] days for patients of Group II, respectively (Figure 3).
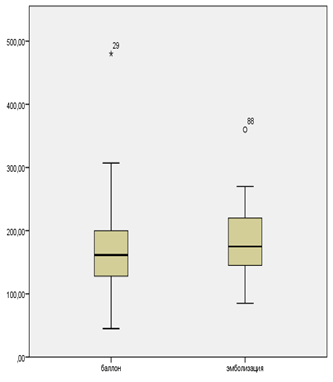
Figure 2 Duration of surgical intervention in patients with placenta accreta, depending on the type of endovascular care.
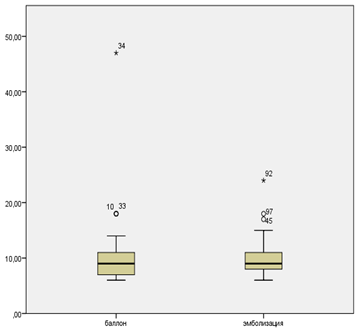
Figure 3 Length of stay of patients with placenta accreta in a hospital depending on the type of endovascular care.
Complications of the nearest postoperative period were observed in 5 (13.2%) patients of group I. Among complications of the postpartum period associated with placenta accrete, it should be noted: uterine bleeding in the early postpartum period in one patient and on the 7th day in the second patient, which required the embolization of uterine arteries to both puerperas; intraperitoneal bleeding of 1000 ml volume 10 hours after the operation, in connection with which relaparotomy and additional hemostatic sutures were performed; tamponade of the bladder with a clot, which was diagnosed by ultrasound on the 5th day, was eliminated during urethrocystoscopy by coagulation of the bleeding vessel; thrombosis of the femoral artery in the early postoperative period in connection with the rupture of the balloon at the next injection of the mixture by a syringe-manometer, was eliminated by thrombectomy. It should be noted that among the five complications of the postpartum period, only one-thrombosis of the common femoral artery was directly related to the endovascular support provided, in the remaining cases the developed complications are related to the technical features of the operation being performed.
The results show the possibility and effectiveness of the application of temporary balloon occlusion of common iliac arteries in patients with scar on the uterus after a cesarean section and placenta acreta. The duration of surgical intervention in the puerperas who underwent a temporary balloon occlusion of the general iliac arteries was significantly lower than in patients whose delivery was supplemented by uterine artery embolization - 161.5 [128.7; 200], and 175 [145; 218.7]min respectively. There was a slight predominance in the reduction of red blood for patients of Group II. Thus, the level of erythrocytes in patients of group I decreased 1.17 times from 3.4 (3.29, 3.7) vs 2.9 (2.6, 3.4), while in patients of group II it was 1.18 times (3.8 (3, 5, 4.01) vs 3.2 (2.7, 3.74) The level of hemoglobin 104.5 (95.25, 115) vs 91 (80.25, 101.25) (a decrease of 1.14 times for patients of group I) and 112 (107; 118) vs 96 (87.5, 105.5), a decrease of 1.16 times for group 2. In turn, the hematocrit in group I decreased from 30.8 (27.5, 34.1) vs 27.65 23,1, 29,1) (decrease by 1.1 times), and in group II 32.7 (31.1, 34.9) vs 27.75 (25.13, 29.6) - 1.2 times Also among the patients I group was significantly lower than the blood loss amount of 1642±1146ml (or 27.5±22.0% bcc) versus 1974±1445ml (or 29.7±22.4% OC.
However, it should be noted that this study is the first study in the country in which the experience of just one clinic is used. For a final understanding of the advantages of this or that method of preventing massive obstetric hemorrhage through endovascular methods, a multicenter, randomized trial is needed.
None.
The author declares there is no conflict of interest.

©2018 Kurtser, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.