International Journal of
eISSN: 2574-9889


Introduction: Depression is a serious psychiatric problem for women affecting their overall health, it has a negative impact on pregnancy and its outcomes maternal depression also increases risk factor for suicide and infanticide. The aim of this study is to determine the prevalence of depression among pregnant women attending ANC follow up clinic at higher two health center, Jimma teaching health center, Shenen Gibe hospital and JUSH.
Methods: A cross-sectional study was conducted among 228 pregnant women having ANC follow up at public health care setting in Jimma town, from May 29 to June 7, 2018, using convenience sampling technique. Data was collected using both interviewer administered and self-administered structured and pretested questionnaire. Collected data was analyzed using the SPSS version20.0 and descriptive statistics and chi-square test was done to assess association between variables, which declared at p-value less than 0.05. Finally obtained results presented using simple frequency tables and charts.
Results: A total of 228 mothers participated in the study, 88(38.6%) of the respondents were between 25-29 years of age, 104(45.6%) were Oromo, 100(43.9%) were Muslim, 90(39.5%) were illiterate, and 67(29.4%) of them were house wife. One hundred thirty eight (71.9%) were multi gravid, 136(59.6%) were second trimester, 48(21.1%) had history of abortion, 128(56.1%) and 152(66.7%) of respondents reported that pregnancy was planned and supported, 12(5.3%) had past history of mental illness, 24(10.5%) reported family history of mental illness, 20(8.8%) had history of khat chewing and 40(20.6%) had history of violence in the past one year. Eighty (35.09%) of them were possibly depressed. Age, ethnicity, marital status, educational status, and occupation of the mother’s were socio demographic characteristics strongly associated with maternal depression (p=0.000), and vidity, history of life time abortion, unplanned pregnancy, personal past history of mental illness, family history of mental illness and history of partner violence were maternal characteristics strongly associated with maternal depression (p<0.001).
Conclusion: Prevalence of depression among respondents was found to be higher. Socio demographic and maternal characteristics were found to be factors strongly associated with maternal depression.
Keywords: prevalence, associated factors, pregnant mothers
Depression is the most prevalent psychiatric disorder during pregnancy and is associated with Psychosocial and clinical obstetric factors. Maternal depression is an all-encompassing term for a spectrum of depressive conditions that can affect mothers (up to twelve months postpartum) and mothers-to-be.1 Epidemiological studies in western societies generally show that depressive episodes occur in 10–20% of pregnant women. Longitudinal studies have demonstrated that antenatal depression is one of the most powerful predictors of postnatal depression. There is also a growing literature that shows that antenatal psychological distress can adversely affect maternal and foetal well being.2 The detection of antenatal depression is important in that it is a predictor of postnatal depression and it has been shown that it can be treated and done so in a cost effective manner. In Africa where medical personnel are scarce, identification of depressed pregnant women can be improved by systematic screening for antenatal depression in the primary health centres using self-report questionnaires.3
A cross-sectional study done on the prevalence and risk factors of depression among 331 pregnant women attending a public health clinic in Brazil shows the prevalence of depression during pregnancy 14.2% and 64.4% were married; 59.2% had a low level of educational attainment; 46.8% were unemployed; and 33.5% were classified as having a low socioeconomic status. The current pregnancy was unplanned for 62.2% of participating women and around 26% reported history of abortion. Out of them 40% were primipara, and 31.2% were in their second pregnancy. 23% of the entire sample reported a previous history of depression, while only 3.3% reported any previous psychiatric treatment. From the sampled women, 10.9% of them are current smokers, 6.3% were current alcohol users, and 1.8% was current illicit drug users.4,5
In a study conducted at three obstetrics clinics for low-income women located in a mid-sized Midwestern city in US. At first and second ante partum interviews, respectively, 27.6% and 24.5% of the women were depressed .Particularly heightened risk for ante partum depression was found among single women who didn’t have a cohabiting partner and none of the other demographic variables predict depression diagnostic status during pregnancy.6 In a study conducted on a sample of adolescent and adult Portuguese mothers to study prevalence as well as risk factors for pregnancy and postpartum depression using Edinburgh Postnatal Depression Scale (EPDS), rates for EPDS>12 are high during the 3rd trimester of pregnancy (18.5%). Adolescent mothers presented more depressive symptoms than adult mothers, both in pregnancy (25.9% versus 11.1%) and at 2–3 months postpartum (25.9% versus 9.3%); moreover, when considering other socio-demographics, adolescent mothers were still at risk for depressive symptoms during pregnancy. Women depressed in pregnancy, and ones who are under 18 years old and who live with the partner, were at risk for postpartum EPDS>12.7
A study done on the prevalence of pre and post partum depression in Jamaica on 73 healthy pregnant mothers indicate that 41(56.16%) mothers were having depression at 28 weeks prepartum. Out of these 41, 23 (31.5%) had mild, 13 (17.8%) had moderate and 5 (6.9%) had severe depression. From the 41 mothers 31 (75.6%) were single or not legally married. Age, parity, miscarriages and employment status was not associated with depression.8 Similarly as part of an ongoing intervention project pregnant women were screened using a brief (10 minute) screening questionnaire in 10 obstetrics clinics in south eastern Michigan. This screen measured demographics, tobacco and alcohol use screening measure, and depression measures, including the Centre for Epidemiological Studies-Depression scale (CES-D), use of antidepressant medications, past history of depression, and current treatment (i.e., medications, psychotherapy, or counseling) for depression. Of women screened, 20% (n = 689) scored above the cut off score on the CES-D, and only 13.8% of those women reported receiving any formal treatment for depression. Past history of depression, poorer overall health, greater alcohol use consequences, smoking, being unmarried, unemployment, and lower educational attainment were significantly associated with symptoms of depression during pregnancy. Maternal age, parity, number of weeks gestation, and race/ethnicity were found to be unrelated to CES-D.9
According to a cluster-randomized controlled trial conducted in Cape Town peri-urban settlements, the prevalence of depressed mood in pregnancy was 39%.The identified strongest predictors of depressed mood were lack of partner support(OR = 0.88, 95% CI =0.8-0.97), intimate partner violence in the previous year(OR = 1.49, 95% CI = 1.13-1.96), having a household income below R2000 per month(OR = 1.52, 95% CI = 1.15-2.01), and younger age(OR = 0.97, 95% CI = 0.95-1.0). On another study done in rural South Africa the prevalence of depression was high, 51/109 (47%), with over half of the depressed women 34/51(67%) reporting episode duration greater than two months and 8/51 reported a prior history of depression.3,10
In a cross sectional analysis of prospective study done in peri-urban health clinics in Dar es Salaam, Tanzania, it was found that there is a 39.5% prevalence of depression in pregnant. Having a previous depressive episode (OR 4.35, P<0.01) and conflicts with the current partner (OR 1.89, P<0.01 were independent predictors of antenatal depression.Over two thirds had completed seven or more years of formal education, but only 6.4%achieved more than the compulsory seven years of primary education. Less than a fourth were employed in a cash earning activity in the year prior to assessment and 28.4% were categorized as having relatively lower household wealth status. More than a quarter were experiencing their first pregnancy. About a fifth (20.7%) had ever experienced an abortion.11
In Nigeria, among pregnant woman who were interviewed during their late pregnancy, 8.3% women met the current (2 weeks) DSM-IV diagnosis of depressive disorder. When the pregnant women were dichotomized into depressed (n515) and non-depressed (n5165), the factors associated with depression included age, marital status, gravidity, and whether pregnancy was planned or not.12 Another study conducted in a semi-urban center in Nigeria to examine the pattern of emotional health profile of women during the three trimesters of pregnancy and compare the level of depressive symptoms between these women and non-pregnant controls, a total of 21 (10.8%) pregnant women were picked with clinically significant depressive symptoms compared with 7 (3.6%) subjects in the control group. Significant depressive symptoms were elicited in 8.7%, 4.3% and 14.6% of the pregnant women during the first, second and third trimesters of pregnancy, respectively. The results also showed that the investigated socio demographic and obstetric factors were not significantly associated with symptoms.13
According to an epidemiological review of depression in pregnancy which included 51 studies for systematic review, most gestational depression prevalence rates found in studies in developing countries were around 20%. Among the risk factors elucidated by these studies, most were associated with poverty such as low income, unemployment, financial hardships and poor educational backgrounds. Other reported factors associated with gestational depression were being single or divorced, having violence and psychiatry histories, and lack of social support.14
Research from Ethiopia has found Common Mental Disorders (CMD) in pregnancy, which are characterized by depressive, anxious, panic and somatic symptoms, to be associated with prolonged labor (of more than 24 hours) and delayed initiation of breastfeeding which is associated with a number of adverse outcomes like increased early neonatal mortality, more diarrheal episodes, failure to establish breastfeeding and impaired mother infant bonding.15,16
Study area and period
The study was conducted at public health care setting in Jimma town, which is found 335km south west from Addis Ababa, in oromiya region, Jimma zone. The town has a latitude and longitude of 7°40′N 36°50′E and found on altitude of the 1763 meters above the sea level. Currently public health care setting found in the town includes three health centers, one primary hospital and one specialized hospital offering services to the dwellers of the town and the surrounding community. The study was conducted from May 29 to June 7, 2018.
Study design
A cross-sectional study design was employed.
Source population
The source populations were all pregnant mothers who are attending ANC follow up in Higher two health center, Jimma teaching health center, Shenen Gibe hospital and JUSH.
Study population
Sample of mothers from source population
Sample size determinations and sampling technique
Sample size determinations
The sample is calculated using this formula
Where, n=sample size
z=the standard normal variance (1.96 for 95% CI)
p=estimated prevalence of population,
Since there was no study done on the prevalence of depression in pregnant mothers in the study area as well in Ethiopia, the investigator used a prevalence of 39% which is the prevalence of depression in pregnancy in South Africa.3
d=reliability confidence (margin error) (5%)
With the correction formula nf = n /1 + n/N the sample size will be 228.
Sampling technique
Convenience sampling technique was employed.
Dependant variables
Depression status.
Data collection instruments and techniques
The data was collected by five (5) medical interns, from Jimma Higher Two Health Center, Jimma Teaching Health Center, Shenen Gibe hospital and JUSH ANC follow up clinics using structured interviewer administered and self administered questioner. The standard questionnaire contains EPDS questions and other variables organized according to study objectives, was adapted after reviewing of different literatures and guidelines, The questionnaire contains socio-demographic characteristics, past psychiatric history, family history of mental illness, history of present pregnancy, history of substance use and experience of partner violence.
Data processing and analysis
The collected data was checked for completion, and consistency at end of each data collection day, cleaned data was analyzed by using SPSS Version 16.0. Descriptive data was employed and chi-square test was calculated to assess association between variables and p-value less than 0.05 declared as statistically significant. Results were presented in graph and simple frequency tables.
Data quality control
Ethical consideration
Formal ethical letter was obtained from medicine and health officer coordinator office; data collection started after permission was obtained from administrative bodies of each facilities. Brief explanation of study objectives given for administrative body and study participants, verbal consent was obtained from the study subjects before actual data collection. Counselling and Treatment service was provided for patients diagnosed with depression in collaboration with the respective clinic found in JUSH.
Socio- demographic Characteristics of respondents. A total of 228 respondents conducted for interview all participated in the study making response rate 100%. Majority 88(38.6%) of the respondents were between 25-29 years of age, 104(45.6%) were Oromo, 100(43.9%) were Muslim, 90(39.5%) were illiterate, and 67(29.4%) of them were house wife (Table 1).
|
Frequency n=(228) |
Percentage |
|
Age |
15-19 |
24 |
10.5% |
20-24 |
84 |
36.8% |
|
25-29 |
88 |
38.6% |
|
30-34 |
24 |
10.5% |
|
35-39 |
8 |
3.5% |
|
Ethnicity |
Oromo |
104 |
45.6% |
Amhara |
56 |
24.6% |
|
Dawaro |
20 |
8.8% |
|
Yeme |
16 |
7.0% |
|
Keffa |
16 |
7.0% |
|
Others |
16 |
7.0% |
|
Religion |
Orthodox |
64 |
28.1% |
Muslim |
100 |
43.9% |
|
Protestant |
52 |
22.8% |
|
Others |
12 |
5.3% |
|
Marital status |
Single |
33 |
14.5% |
Married |
159 |
69.7% |
|
Divorced |
21 |
9.2% |
|
Widow |
15 |
6.6% |
|
Educational status |
Litrate |
90 |
39.5% |
Illitrate |
54 |
23.7% |
|
Formally educated |
84 |
36.8% |
|
Occupation |
Housewife |
67 |
29.4% |
Farmer |
56 |
24.6% |
|
Government employee |
61 |
26.8% |
|
Daily labourer |
26 |
11.4% |
|
Others |
18 |
7.9% |
|
Table 1 Socio-demographic Characteristics of respondents, among ANC attendees of public health care setting in jimma town, Jimma Ethiopia, June 2018
Maternal characteristics of respondents
Ninety two (40.4%) of the respondents were pregnant for second time, more than half 136(59.6%) of the respondents were in the second trimester, 48(21.1%) had history of abortion, 128(56.1%) and 152(66.7%) of respondents reported that pregnancy was planned and supported, 12(5.3%) of the respondents ever had past history of mental illness, while 24(10.5%) reported family history of mental illness. Regarding habit of drug using 20(8.8%) of respondents had history of khat chewing and 40(20.6%) had history of partner violence experience in the past one year (Table 2).
|
|
Frequency(n=228) |
Percentage |
Gravidity |
Primi gravid |
64 |
28.1% |
2nd gravid |
92 |
40.4% |
|
3rd gravid |
40 |
17.5% |
|
4th gravid |
20 |
8.8% |
|
>5 gravidity |
12 |
5.3% |
|
Gestational age |
First trimester |
32 |
14.0% |
Second trimester |
136 |
59.6% |
|
Third trimester |
60 |
26.3% |
|
Abortion |
Yes |
48 |
21.1% |
No |
180 |
78.9% |
|
Planned pregnancy |
Yes |
128 |
56.1% |
No |
100 |
43.9% |
|
Supported pregnancy |
Yes |
152 |
66.7% |
No |
76 |
33.3% |
|
Past mental illness history |
Yes |
12 |
5.3% |
No |
216 |
94.7% |
|
Family history of mental illness |
Yes |
24 |
10.5% |
No |
204 |
89.5% |
|
Current drug use |
Khat |
20 |
8.8% |
No use |
208 |
91.2% |
|
History of violence |
Yes |
47 |
20.6% |
No |
181 |
79.4% |
Table 2 Maternal characteristics of respondents, among ANC attendees of public health care setting in Jimma town, Jimma Ethiopia, June 2018
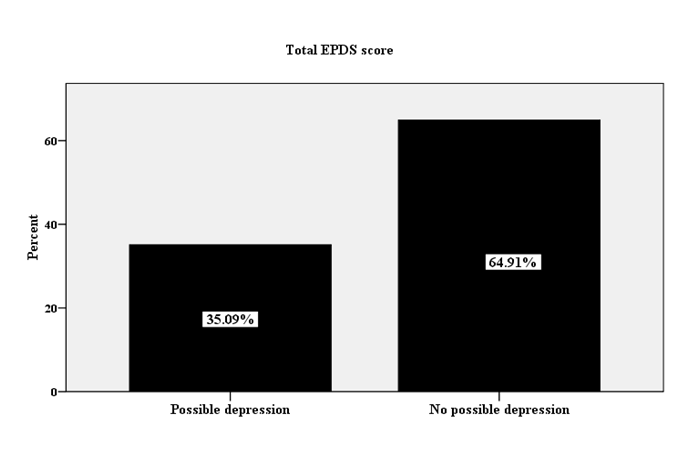
EPDS score of depression
As the results of EPDS score showed that 80(35.09%) of the mothers were possibly depressed (Figure 1).
Factors associated with maternal depression
As the results of the study showed that age, religion, marital status, educational status, low income and occupation of the mother’s were socio demographic characteristics strongly associated with maternal depression (p<0.001) (Table 3). Also study showed gravidity, history of life time abortion, plan for pregnancy, personal past history of mental illness, family history of mental illness and history of violence during life time were maternal characteristics strongly associated with maternal depression (p<0.001) whereas gestational age and current drug use are not associated (Table 4).
|
Possible depression |
No possible depression |
Total |
X2 |
Df |
p-value |
||||
|---|---|---|---|---|---|---|---|---|---|---|
No |
% |
No |
% |
No |
% |
|||||
Age |
15-19 |
16 |
7.0% |
8 |
3.5% |
24 |
10.5% |
55.115 |
4 |
<0.001 |
20-24 |
40 |
17.5% |
44 |
19.3% |
84 |
36.8% |
|
|
|
|
25-29 |
16 |
7.0% |
72 |
31.6% |
88 |
38.6% |
|
|
|
|
30-34 |
0 |
.0% |
24 |
10.5% |
24 |
10.5% |
|
|
|
|
35-39 |
8 |
3.5% |
0 |
.0% |
8 |
3.5% |
|
|
|
|
Total |
80 |
35.1% |
148 |
64.9% |
228 |
100.0% |
|
|
|
|
Marital status |
Single |
29 |
12.7% |
4 |
1.8% |
33 |
14.5% |
50.218 |
3 |
<0.001 |
Married |
39 |
17.1% |
120 |
52.6% |
159 |
69.7% |
|
|
|
|
Divorced |
9 |
3.9% |
12 |
5.3% |
21 |
9.2% |
|
|
|
|
Widow |
3 |
1.3% |
12 |
5.3% |
15 |
6.6% |
|
|
|
|
Total |
80 |
35.1% |
148 |
64.9% |
228 |
100.0% |
|
|
|
|
Educational status |
Literate |
17 |
7.5% |
73 |
32.0% |
90 |
39.5% |
62.098 |
2 |
<0.001 |
Illiterate |
43 |
18.9% |
11 |
4.8% |
54 |
23.7% |
|
|
|
|
Formally educated |
20 |
8.8% |
64 |
28.1% |
84 |
36.8% |
|
|
|
|
Total |
80 |
35.1% |
148 |
64.9% |
228 |
100.0% |
|
|
|
|
Occupation |
Housewife |
7 |
3.1% |
60 |
26.3% |
67 |
29.4% |
66.512 |
4 |
<0.001 |
Farmer |
36 |
15.8% |
20 |
8.8% |
56 |
24.6% |
|
|
|
|
Government employee |
9 |
3.9% |
52 |
22.8% |
61 |
26.8% |
|
|
|
|
Daily labourer |
18 |
7.9% |
8 |
3.5% |
26 |
11.4% |
|
|
|
|
Others |
10 |
4.4% |
8 |
3.5% |
18 |
7.9% |
|
|
|
|
Total |
80 |
35.1% |
148 |
64.9% |
228 |
100.0% |
|
|
|
|
Table 3 Distribution of Socio-demographic Characteristics of respondents, by EPDS score of respondents among ANC attendees of public health care setting in jimma town, Jimma Ethiopia, June 2018
|
Possible depression |
No possible depression |
Total |
X2 |
Df |
p-value |
||||
|---|---|---|---|---|---|---|---|---|---|---|
No |
% |
No |
% |
No |
% |
|
|
|
||
Gravidity |
Primi gravida |
44 |
19.3% |
20 |
8.8% |
64 |
28.1% |
51.643 |
4 |
<0.001 |
2nd gravid |
16 |
7.0% |
76 |
33.3% |
92 |
40.4% |
|
|
|
|
3rd gravid |
12 |
5.3% |
28 |
12.3% |
40 |
17.5% |
|
|
|
|
4th gravid |
8 |
3.5% |
12 |
5.3% |
20 |
8.8% |
|
|
|
|
>5 gravidity |
0 |
.0% |
12 |
5.3% |
12 |
5.3% |
|
|
|
|
Total |
80 |
35.1% |
148 |
64.9% |
228 |
100.0% |
|
|
|
|
Abortion |
Yes |
28 |
12.3% |
20 |
8.8% |
48 |
21.1% |
14.425 |
1 |
<0.001 |
No |
52 |
22.8% |
128 |
56.1% |
180 |
78.9% |
|
|
|
|
Total |
80 |
35.1% |
148 |
64.9% |
228 |
100.0% |
|
|
|
|
Planned pregnancy |
Yes |
36 |
15.8% |
92 |
40.4% |
128 |
56.1% |
6.212 |
1 |
.013* |
No |
44 |
19.3% |
56 |
24.6% |
100 |
43.9% |
|
|
|
|
Total |
80 |
35.1% |
148 |
64.9% |
228 |
100.0% |
|
|
|
|
Past mental illness history |
Yes |
10 |
4.38% |
2 |
0.92% |
12 |
5.3% |
23.433 |
1 |
<0.001 |
No |
70 |
30.07% |
146 |
64.03% |
216 |
94.7% |
|
|
|
|
Total |
80 |
35.1% |
148 |
64.9% |
228 |
100.0% |
|
|
|
|
Family history of mental illness |
Yes |
16 |
7.0% |
8 |
3.5% |
24 |
10.5% |
11.744 |
1 |
.001* |
No |
64 |
28.1% |
140 |
61.4% |
204 |
89.5% |
|
|
|
|
Total |
80 |
35.1% |
148 |
64.9% |
228 |
100.0% |
|
|
|
|
Current drug use |
Khat |
8 |
3.5% |
12 |
5.3% |
20 |
8.8% |
.232 |
1 |
.630 |
No use |
72 |
31.6% |
136 |
59.6% |
208 |
91.2% |
|
|
|
|
Total |
80 |
35.1% |
148 |
64.9% |
228 |
100.0% |
|
|
|
|
History of violence |
Yes |
39 |
17.1% |
8 |
3.5% |
47 |
20.6% |
59.618 |
1 |
.000* |
No |
41 |
18.0% |
140 |
61.4% |
181 |
79.4% |
|
|
|
|
Total |
80 |
35.1% |
148 |
64.9% |
228 |
100.0% |
|
|
|
|
Table 4 Distribution of maternal characteristics, by EPDS score of respondents among ANC attendees of public health care setting in jimma town, Jimma Ethiopia, June 2018
According to some studies, the prevalence of depression in pregnant mothers was found to be high and shows prevalence rates of depression during pregnancy were significantly higher in low-income countries, the finding of this study showed that the prevalence of depression among study participants found to be 35.09%. Even though there was a limitation of literatures in our country on this issue, different literatures showed that prevalence was ranged from 8.3% to 56.16% for study conducted in Nigeria and Jamaica respectively(8, 12). Another epidemiological review of 51 studies on depression in pregnancy, reported that gestational depression prevalence rates in developing countries were around 20%(14). However comparable results reported from cluster-randomized controlled trial conducted in Cape Town and cross sectional study in Dar es Salaam found that 39% and 39.5% respectively(3, 11). In addition literatures showed that the prevalence of depression during pregnancy varied ranging as, 10.8%, 14.2% and 47% for study conducted in a semi-urban centre in Nigeria, in Brazil and in rural of South Africa respectively. The difference between these studies probably may due to difference among study participants in relating to social background. Regarding factors associated with gestational depression, this study showed that socio demographic characteristics such as age, marital status, educational status, and occupation of the mother’s and also maternal factors such as gravidity, history of life time abortion, plan for pregnancy, personal past history of mental illness, family history of mental illness and history of partner violence in one year time were factors strongly associated with maternal depression during pregnancy (p<0.001).
Also studies suggested many factors associated with the problem of gestational depression among that study conducted on a sample of adolescent and adult Portuguese mothers, showed that socio demographics characteristics such as maternal age, and gestational age were risk factors for pregnancy and postpartum depression.7 In addition study from south eastern Michigan. Past history of depression, poorer overall health, greater alcohol use consequences, smoking, being unmarried, unemployment, and lower educational attainment were significantly associated with symptoms of depression during pregnancy.9 Also study from Cape Town reported that strongest predictors of depressed mood during pregnancy were lack of partner support, intimate partner violence in the previous year, having a household income below R2000 per month, and younger age.3
Study from Nigeria showed that factors associated with depression included age, marital status, gravidity, and whether pregnancy was planned or not12 and similarly study done in Dar es Salaam found that having previous depressive episode conflicts with the current partner were predictors of antenatal depression.11 Furthermore according to study of an epidemiological review of depression in pregnancy, among the risk factors elucidated by these studies, most were associated with poverty such as low income, unemployment, financial hardships and poor educational backgrounds. Other reported factors associated with gestational depression were being single or divorced, having violence and psychiatry histories, and lack of social support.14 This implies that many factors contributed to maternal depression during pregnancy besides physiological factors, which needs attention.
In contrary to these results of study conducted in a semi-urban centre in Nigeria showed that the investigated socio demographic and obstetric factors were not significantly associated with symptoms13 and also as reported from a study conducted at Midwestern city in US, showed that none of the other demographic variables predict depression diagnostic status during pregnancy.6 Similar findings reported from study conducted in Jamaica, and Michigan.8,9 The difference may due to difference of sample size of studies, or due to difference of study participants’ socio demography.
This cross sectional study was conducted to assess prevalence and associated factors among ANC attendees on public health care facility in jimma town, from the study findings the following conclusions drawn:
Prevalence of depression among respondents was found to be higher.
Socio demographic and maternal characteristics were found to be factors strongly associated with maternal depression.
Recommendations
Based on findings of the study the following recommendations are forwarded:
As the prevalence of depression among pregnant mothers is high, extensive research should be done to as national level. Medias and non government organizations should be involved in teaching the community about female education, contraception methods as being pregnant as single and unplanned pregnancy are strong risk factors.
The spreadsheet data supporting the findings of this work is available at the hands of the corresponding author.
Ethics statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the declaration and its later amendments or comparable ethical standards. Before the commencement of the study, ethical approval was secured from the Jimma University Ethical Review Board. Written informed consent was obtained from all individual participants included in the study.
Consent
The purpose of the study was explained to the study participants at the time of data collection and verbal consent was secured from each participant before the start of data collection. Confidentiality was ensured by not including names or other identifiers in the data collection tool. The right of the participants to refuse participation or not to answer any of the questions was respected.
I would like to thank the Jimma university specialized hospital,Jimma health center teaching,Shenen Gibe Hospital and Higher two health center as well as the administrative staffs for all the help and support given for us during the data collection period. I also thank Jimma university institute of health for permitting us to conduct this study.
Author contribution
Abiru Neme, conceived and designed the protocol contributed on data analysis, and checked the draft. Abiru Neme prepared manuscript. Author read and approved the final paper.
Author declared that they have no conflict of interests. Jimma University covered only the survey cost for this study and there is no any funding organization.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.