International Journal of
eISSN: 2470-9980


A high-sensitivity c-reactive protein (hs-CRP) is one of the acute phase proteins which remarkably increased in systemic inflammation and considered to be an independent risk factor for Cardio Vascular Diseases (CVD). The present study was conducted to evaluate the level of (hs-CRP) in pre and post menopausal women. Two study groups were enrolled in the present study .The first group included (100) samples from healthy pre menopausal woman of age ranged (27-45)years. The second group included (90) samples taken from healthy postmenopausal women their age ranged (51-67)years .The following Kit from (i-CHRomTM hs CRP-25) was used as an immunoassay pattern to evaluate hs-CRP from Boditech MedIne . The results of the present study showed a significant differences between the two groups under study , in which the level of hsCRP in pre- was( 1.81_+1.02) with a significant increase (p<0.05) in post menopausal women (4.02+_1.67mg/L).This study concludes that there is approximately 3 fold significant increase in hs-CRP levels in post menopausal Iraqi’s women.
CRP is a pathogenic inflammatory protein as it was elevated in people with a variety of illnesses including cancer.1 Is the prototype a cute - phase protein primary synthesized in the liver and its release is stimulated by interleukin 6 (1L-6).2 The normal range has to be less than 3mg/l in healthy people .in different study have show that the average value between (0.9 -2.05mg/l).
This protein needs 6-12hour at the initiation of the disease to reach it peak in blood and could increase to reach 100 folds .this protein the half life is 15-25hour but decrease to its normal values at the recovery state. It has been found that CRP concentration are actually relatively constant in an individual, both with regard to time of day, and over days and months, even over months to years.3
Two functional properties of CRP have been demonstrated Firstly, it’s ability to recognize foreign pathogens, as well as, phospholipids constituents of damaged cells resulting in elimination of the target cells by the interaction with both humeral and cellular effecter systems, secondly, it’s ability to modulate the function of phagocytes cells.4
A growing body of evidence has supported the idea that cardiovascular diseases including coronary heart disease, ischemic stroke, and acute myocardial infarction, develop, at least in part, because of a chronic low-level CRP of the vascular endothelium.5 Apparently, besides of being directly involving in low grade chronic systemic inflammation, high-sensitivity CRP (hsCRP) is emerging as the strongest and most independent predictive risk factor for atherosclerosis and CVD.6,7 Cardiovascular risk assessment cut-offs have been recommended by American Heart Association (AHA) as Low risk: (<1.0mg/L), Average risk: (1.0 ~ 3.0mg/L) and High risk: (>3.0mg/L). The present study was conducted to evaluate the level of (hs-CRP) in pre and post menopausal women in Iraqis’ women.
The collection of blood samples was done from January to 30 June 2015. following the taken of blood sample the serum was submitted to evaluate the hs -crp by using i-CHROMATM hsCRP along with i-CHROMATM Reader is a fluorescence immunoassay that measures CRP in serum, plasma, and whole blood. The test is used as an aid to see infection and inflammation. Immunoassay for Quantitative Measurement of High-Sensitivity C-Reactive Protein (hsCRP) in Human Whole blood with i-CHROMATM Reader System.
Test principle
i-CHROMATM hsCRP is based on fluorescence immunoassay technology 7,8. The i-CHROMATM hsCRP uses a sandwich immunodetection method, such that by mixing detector buffer with blood specimen in test vial, the fluorescence-labelled detector anti-CRP antibody in buffer binds to CRP antigen in blood specimen. As the sample mixture is loaded onto the sample well of the test device and migrates the nitrocellulose matrix of test strip by capillary action, the complexes of detector antibody and CRP are captured to anti-CRP sandwich pair antibody that has been immobilized on test strip. Thus the more CRP antigen is in blood specimen, the more complexes are accumulated on test strip. Signal intensity of fluorescence of detector antibody reflects amount of CRP captured and is micro processed from i-CHROMATM Reader to show CRP concentration in blood specimen. The default result unit of i-CHROMATM hsCRP is displayed as an mg/L from i-CHROMATM Reader. The working range and the detection limit of i-CHROMATM hsCRP system are 0.1-10mg/L. and 0.1mg/L, respectively.
Procedure
The full procedure was performed following the detailed leaflet of the Kit
i-CHROMATM Reader calculates hsCRP Test results automatically and displays CRP concentration on the screen as form of mg/L. For further information, refer to the Operation Manual for thi-CHROMATM Reader.
Statistically data using statistical analysis software (MINITAB) according to T_test test. Have been obtained on the arithmetic mean and standard deviation of the data in the study and use. P_value statistical significance as the level significantly (p <0.05) and significantly high (P <0.01)
Table 1 and Figure 2 showed that there were a significant difference s (p<0.05) of hs-CRP values of premenopausal (1.81±1.02) when compared to postmenopausal women (4.02±1.67) with no significant differences (p>0.05) between study age groups and subjects illustrated in Table 1.
Subjects |
Total No. |
Study Groups |
Mean SD hs-CRP mg/L |
Total |
Premenopausal Women |
100 |
(27-34) yrs. |
1.64 ± 1.01 |
1.81 ± 1.02 |
N= 63 |
||||
(35-45) yrs. |
1.93 ± 1.09 |
|||
N= 37 |
||||
Postmenopausal women |
90 |
(51-58) yrs. |
3.69 ± 0.87 |
4.02 ± 1.67 |
N= 67 |
* |
|||
(59-67) yrs. |
4.33 ± 1.53 |
|||
|
|
N= 23 |
|
|
Table 1 The effect of age groups on high sensitivity CRP level in healthy pre and post menopausal women
hs-CRP highly sensitive C-reactive Protein
** Highly significant p≤ 0,01.
*Significant p≤ 0.05.
ns: Non significant p> 0.05.
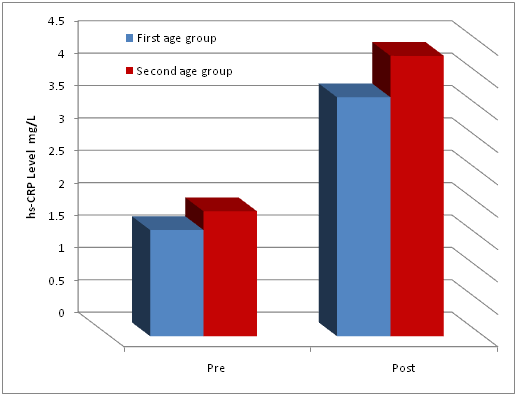
Figure 2 The effect f age groups on high sensitivity CRP level in healthy pre and post menopausal women.
The result of the present study is agreed with published result of8 which is been found a significant differences in the levels of the studied hs-crp regarding pre and postmenopausal women with approximately 3 fold increase of hs-crp in the serum of postmenopausal healthy women when compared to pre menopausal.
On the other hand, this study was comparable to that of9 which found no significant differences between pre and post.
An elevated level of hs-crp in post is contributable to the deposition of lipids according to the life style and estrogen shortage and the role of lipids in the production of proinflammatory mediators like hs-crp. Moreover, the decreased function of ovaries and the significant changes in sex hormone. CRP binds to oxidized LDL which leads to an increase in adhesion molecules promoting complement proteins and trigger inflammation in atherosclerotic plaques. Furthermore, CRP promote the induction of tissue factor, the remarkable factors on monocyte surface which is considered to be one of the important coagulation factors, also increase adhesion molecules and manipulate the production of nitric oxide.8 The removal of the regulatory effect of estrogens up on hs-crp leads to an increase of hs-crp level in postmenopausal women accumulating the increased risk of cardiovascular disease (CVD).
The cross sectional nature of the present study limits the ability our results to evaluate the relationship between hs-crp and menopause. That needs a long term study with large scale population and sample size. It needs to be emphasized that the significant increased levels of hs-crp in pre and post indicate clearly and increased risk of CVD in postmenopausal women in Kirkuk city in Iraqis women, this increase may be more than the other ethnicities in different world populations. This was clearly indicated by Rifai et al. & michelle et al.,10,11 and the late suggestion of AHA American heart association for those women to be less-clearly sick women and they are candidate to be prevented for CVD. Goff et al.,12 is proved that CRP is a prominent indicator and one of the independent and important risk factors to develop CVD rr=4.4 in patient’s future, LDL come secondly to hs-crp in this regard13,14 (Figure 2).
None.
Author declares there are no conflicts of interest.
None.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.