International Journal of
eISSN: 2573-2889


Case Series Volume 4 Issue 5
1Department of ENT, Government Medical College, India
2Department of ENT, All India Institute of Medical Sciences, India
Correspondence: Dr. Darwin Kaushal, Associate Professor, Department of ENT, Room 408, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India
Received: October 19, 2019 | Published: October 31, 2019
Citation: Yadav V, Kaushal D, Gugliani A. Pediatric temporal bone langerhans cell histiocytosis: report of 2 cases with review of literature. Int J Mol Biol Open Access. 2019;4(5):185-187. DOI: 10.15406/ijmboa.2019.04.00118
Introduction: Langerhans cell histiocytosis is a rare multiorgan disorder, commonly seen in the pediatric age group. Commonest presentation of the disease involving the temporal bone is ear discharge. This entity is often underdiagnosed and the patient is treated with multiple courses of antibiotics which leads to delay in diagnosis and initiating apropriate treatment.
Case report: We present case reports of 2 children who presented to us with this rare disease. The line of management followed is discussed briefly. Our aim is to increase awareness of this disease amongst otolaryngologists and pediatricians so that they can identify such cases in a timely manner.
Conclusion: Langerhans cell histiocytosis can affect any age group but is commonly seen in children. It can involve any organ system but the temporal bone is involved in most cases. The differential diagnosis of this disease should be kept in mind for any patient presenting with chronic ear discharge that is not responding to the appropriate line of management.
Keywords: langerhans cell histiocytosis, temporal bone, ear discharge, otitis media
Abbreviations: LCH, langerhans cell histiocytosis; CT, computerized tomography; USG, ultrasonogram
Langerhans cell histiocytosis (LCH) is a rare disorder characterized by the accumulation of Langerhans cells. Its presentation may vary from a single lesion to multisystem involvement. Flat bones, especially that of skull are commonly involved.1 50-80% of pediatric LCH are found in the region of head and neck, and of these, about 15-60% involve the temporal bone.2 Clinical presentaion is variable and often non specific and resembles that of otitis externa, otitis media or cholesteatoma. Because of the misleading symptoms, the timely diagnosis is usually delayed. We present 2 such cases of pediatric LCH. Our aim is to create awareness about this rare disease for its early diagnosis and initiation of treatment.
A 11 months old male baby presented with complaints of bilateral ear discharge, dandruff & crusting on scalp and skin rash on right axilla and nape of neck since 4 months. He had a right post auricular swelling followed by post aural discharge since 3 weeks. The child was seen by an ENT specialist and started on broad spectrum intra-veinous(IV) antibiotics along with post-aural wound debridement. The tissue was sent for histopathological examination which showed foci of necrosis, lymphocytes, macrophages and plasma cells.
As the patient did not respond to iv antibiotics, he was referred to our hospital. On examination, child was febrile but taking feeds regularly. Local examination of the right ear showed an infected post aural wound with sutures in situ (Figure 1).
The external auditory canal was edematous and tympanic membrane had a central moderate sized perforation with granulations. Left ear had a small, central perforation of the tympanic membrane. Clinically, facial nerve was intact bilaterally. Based on these findings, differential diagnosis were bilateral chronic suppurative ottitis media, langerhans cell histiocytosis and granulomatous diseases.
Haemogram reports showed hemoglobin of 8.5 gm/dl and the total leucocyte count 20,500 per cumm. Peripheral blood film was suggestive of microcytic hypochromic anaemia.
Urine routine examination was within normal limits. C reactive protein was 4.8 mg/dl (positive >0.6). A contrast enhanced computerized tomography (CT) scan of the temporal bone showed bilateral ottitis media with erosion of right side mastoid bone and right post auriclar abscess (Figures 2&3).
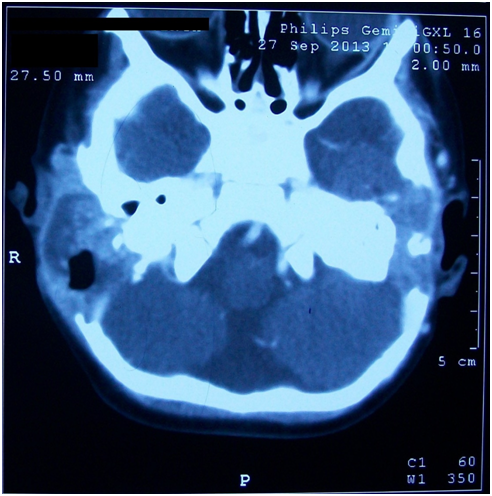
Figure 2 CECT Temporal bone(Axial view) shows bilateral mastoditis and bilateral erosion of posterior cranial fossa dural plate.
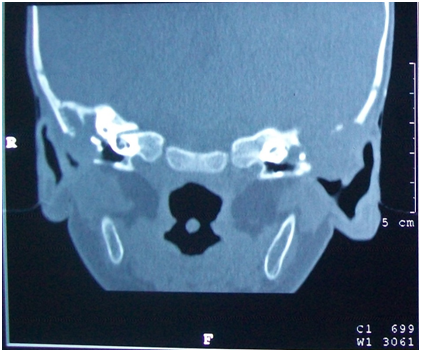
Figure 3 HRCT Temporal bone (coronal view) shows soft tissue density in bilateral middle ear, attic. There is also erosion of bilateral dural plate.
Repeat tissue biopsy was taken from the right mastoid antrum and sent for immunohistochemical examination. It came out positive for CD 100 , CD 68 and Langerin, thus suggesting LCH. Ultrasonogram (USG) of abdomen was done to rule out systemic involvement. The patient was referred to a medical oncologist and started on vinblastine chemotherapy for 16 weeks. The child is on regular follow up and is now in remission.
A 5 year old female child was brought to us with the complaints of right ear mucopurulent, non-foul smelling, non blood stained discharge since 1 year of age and a swelling behind the right ear since 3 months. This was followed by purulent discharge from swelling since 1 month.
Local examination revealed a post auricular fistula. On examination of the tympanic membrane, a moderate sized central perforation was seen with granulations in the middle ear.
High resolution CT of the temporal bone showed a soft tissue density in attic, aditus and antrum. The dural plate and sinus plate were found to be eroded (Figures 4&5).
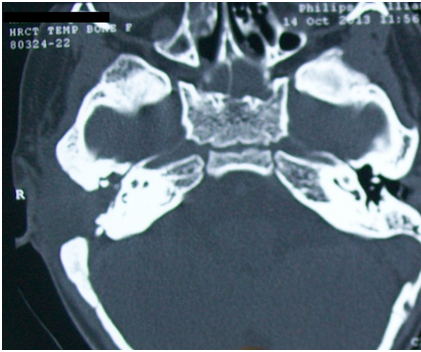
Figure 4 HRCT temporal bone (axial view) shows soft tissue density in right middle ear, mastoid air cells. Left middle ear is normal.
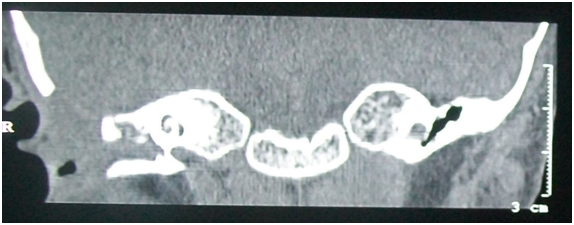
Figure 5 HRCT Temporal bone (coronal view) shows soft tissue density in right middle ear, attic and external auditory canal.
The child was satrted on broad spectrum iv antibiotics and planned for tympanomastoid exploration under general anaesthesia. Granulations were seen in the mastoid antrum, aditus, attic and middle ear.
These were sent for histopathological examination and were positive for langerin. Thus, a diagnosis of LCH was made. The patient was also started on vinblastine chemotherapy for 16 weeks and is in complete remission.
Langerhans cells (LC) were first described by Paul Langerhans in 1868.3 These are dendritic cells derived from the bone marrow and are found in the basal and the supra-basal layer of the epidermis. LC are antigen presenting cells and are thus involved in antimicrobial immunity.4 LCH is a histiocytic disorder and occurs due the clonal proliferation of immature LC along with eosinophils, macrophages, lymphocytes and sometimes, multinucleated giant cells.5 Langerhans cell histiocytosis comprises of 3 entities namely, eosiniophilic granuloma, Hand-Schüller-Christian disease and Letterer-Siwe disease as described by Liechtenstein.6 The characteristic feature is the identification of Birbeck granules on electron microscopy.7 The peak incidence period is between 1-4 years and is twice as common in the males than in females.8
The diagnosis of LCH is based on the hematological and histological criteria given by the Histiocyte Society in 1987 along with positive staining of the lesional cells with CD1a, langerin (CD207) or both.9 For LCH of the temporal bone, the most common site of involvement is the mastoid process, which may present as otorrhoea and a periauricular mass.10 Fernandez-Latorre et al reported series of 62 patients demonstrated temporal bone involvement in 22.6%, and bilateral temporal bone involvement was seen in (28%) of the 12 patients with temporal bone occurrence.11 Buchmann L et al in their study found 17out of 22 (77%) patients of LCH had head and neck involvement.12 CT findings are nonspecific for this disease. Coutte et al found that LCH was impossible to distinguish from cholesteatoma based on CT findings.13
Differential diagnosis to be kept in mind in such cases are chronic suppurative otitis media, rosai-dorfman disease, rhabdomyosarcoma and granulomatous diseases like sarcoidosis and tuberculosis. Treatment options include surgery, radiotherapy, chemotherapy as single modality or different combinations depending on the extent of the disease.
The role of surgery is limited to tissue biopsy and/or debridement as Langerhans cell histiocytosis is a systemic disease. Prognosis is poor in younger patients or those multifocal disease. Therefore, early diagnosis and treatment is important for control and better prognosis of disease.
None.
None.
The author declares there is no conflicts of interest.

©2019 Yadav, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.