International Journal of
eISSN: 2573-2838


Research Article Volume 8 Issue 2
1Biomedical engineering, Universidade Brasil, Brazil
2Faculty of Medical Sciences, UNICAMP, Brazil
3Doctorate in Physiotherapy, Federal University of São Carlos, UFSCAR, Brazil
4Allergy and Immunopathology, University of São Paulo, USP, Brazil
Correspondence: Danielle Bastos da Silva Ventura, PhD in progress in biomedical engineering, Universidade Brasil, Brazil
Received: May 03, 2023 | Published: September 21, 2023
Citation: Ventura DBS, Magalhães DSF, Garcia LA, et al. Analysis of cutaneous microrelief after the use of dermaplanage using three-dimensional digital photogrametry. Int J Biosen Bioelectron. 2023;8(2):46-48. DOI: 10.15406/ijbsbe.2023.08.00232
The skin surface is a barrier and can selectively communicate with the internal biological environment and the external environment, it is not flat and contains several straight grooves that can be classified according to depth, and therefore, these conditions that define its micro relief are related to its exchanges and its breathing, so the photogrammetric analysis instruments allow its amplification, making it possible and necessary to describe them. Dermaplaning is a technique used in qualified aesthetic protocols, facial rejuvenation and the treatment of atrophic scars, based on the concept of physically removing the superficial layers of the skin by dragging a blade of sterile, disposable butter from a scalpel. The three-dimensional photogrammetry analysis instruments are modern resources of current tissue bioengineering and allow a form of tissue enlargement in a precise and non-invasive way. Two dermaplaning intervals with 21-day intervals were performed in women between 18 and 38 years old, divided into 2 groups (control n = 21, test n = 21) with complaints of skin texture alteration. The effectiveness of the treatment was evaluated using three-dimensional digital photogrammetry and photothermographic imaging before and after the preparations. The treated group had positive changes in the three-dimensional topographic analyzes of the cutaneous microrelief after the use of dermaplaning.
Keywords: dermaplaning, skin surface, skin microrelief, bioengineering
The surface of the skin is not flat, but contains several straight grooves, which can be classified according to their depth and therefore the magnification that is possible and necessary to describe them. The most visible are wrinkles that are between several millimeters deep, depending on age and environmental factors. They are found in specific areas, for example frown lines on the face and plicatures on the joints and can be seen at low magnification. The first consequence of this complex network of lines of varying depth is to increase the real surface area of the human body compared to its apparent area. Depending on body location and age, the actual area appears to be between 10% and 50% larger than it appears to the naked eye.1 The surface of the skin shows a network that is known as micro relief or texture, presenting rectilinear or parallel grooves that cross each other to form shapes of rectangles, squares, trapezoids and triangles.2
In cicatricial conditions, the cutaneous microrelief also undergoes changes in its depth lines and in such a way as not to follow its evolutionary appearance, andthat when studied in mutually orthogonal directions in the plane of the skin and scars can provide us with information about the directionality of healthy tissue and how directional properties change after injury, suggesting less total collagen in the tissue cross-section. The analysis of the cutaneous surface through three-dimensional images has been used to structurally evaluate the possible damages and can help in the existing structural findings and suggest new treatments for scar tissue remodeling and other disturbances of the cutaneous micro relief through tissue bioengineering, more accurate and non-invasive.3 There are several 2D and 3D techniques that are intended to offer a more objective analysis of wrinkle treatments. This includes line scanning based techniques, which are used for indirect measurement of skin relief, in addition to mechanical and optical microscopy among them.4
The practical applicability of these technologies so that measurements and characteristics of skin parameters can be evaluated. Studies on abnormalities of the cutaneous barrier, such as the amount of water, microcirculation, pigmentation, elasticity, emerged with the creation of standardized equipment, which made it possible to develop methods and obtain reproducible measurements. These methodologies, commonly known as cutaneous bioengineering techniques, proved to be useful in the evaluation of skin diseases and lesions, as well as providing elements for evaluating treatments for these same diseases.5 Such equipment made possible the development of methods and new techniques, being able to offer, in a non-invasive and detailed way, the different characteristics of the skin relief, as well as offering more objective measures, such as the quantification of phenomena. Standardize locations, techniques and environmental conditions, be able to evaluate without interfering with treatments or the spontaneous course of the patient's conditions, and be fundamental to standardize environmental conditions, for the collection of measurements, so that there is reproducibility.1
The image processing technique was recently investigated for inspection of the surface of the skin from its imperfections with cameras capable of producing a 3D shape of the skin, which provides significant information about its conditions. Therefore, from the development of this study, it is intended to demonstrate that Dermaplaning is capable of modifying the cutaneous micro relief and in the conditions of the cutaneous biotype and to identify, through surface microscopy, the alterations of the micro relief before and after the use of dermaplaning and it will be possible to evaluate the changes in the levels of hydration, lubrication, percentage of collagen and elastic fibers from skin analysis using digital photogrammetry. Dermaplaning or Dermaplaning was initially described as a treatment for various skin lesions such as folliculitis and soon after in its new studies it already suggests for the treatment of dermatitis and acne sequelae. This procedure was used in two ways: one using a handheld device with a scalpel blade or the other using an automated dermatome similar to those used for skin grafting, but in a much more superficial way.6
Since the first description of dermaplaning, five decades ago, little information about its effectiveness has been published. In short, the word ''dermaplaning or dermaplaning'' has multiple implications in the aesthetic or dermatological routine, but unfortunately, until the present day, there are few studies and current clinical findings on this subject.7 Literally, it means to scrape away layers of skin. In reality and in practice, it tends to be limited to scraping the upper epidermis (stratum corneum) and is most often used for superficial skin resurfacing. Most countries require medical supervision because the procedure involves a sharp blade, but some beauticians do this as long as they stay within the confines of the epidermis. This is sometimes difficult to control, but dermal bleeding, when it happens due to professional error, usually represents a safe limit and does not leave scars. Furthermore, the licensing process is inconsistent and varies from country to country.8
Pryor et al., in 2011, carried out a systematic review with 24 female volunteers, with 3 sessions of dermaplaning associated with oxygen therapy and photodynamic therapy. findings that Dermaplaning can be a technique to improve the skin biotype inserted in the aesthetic and dermatological routine. Townsend et al., in 2017, conducted a case study using Dermaplaning as a means of treating atopic dermatitis in the retroauricular region. Considering that atopic dermatitis is one of the main factors in the impairment of the skin barrier function and the process that normally causes superficial cells to fall is interrupted, dermoplaning resulted in an improvement in skin desquamation, a decrease in local itching, as well as facilitating the penetration of topical corticosteroids and emollients that were administered after scraping in order to limit eczema flare-ups.
Twenty-two female volunteers, aged between 18 and 38 years, phototype I to IV according to the Fitzpatrick scale, with complaints of changes in skin texture or rough skin, were recruited.9 A clinical interview, anamnesis and facial clinical examination form were carried out, after the evaluation interview, the volunteers consented to participate in the study and were informed about the exclusion criteria and signed the TCLE - Term of Free and Informed Consent being informed about their knowledge and commitment to respect them during the research, according to the consolidated opinion of the Ethics Committee n 4,652,924 approved on April 24, 2021. The volunteers received two sessions of dermaplaning, the face being subdivided into 2 groups: right side of the face, being the placebo group and the left side of the face, being the test group. Two sessions were performed with an interval of 21 days between the same sessions. Voluntary absence of gestational period, lactation, uncontrolled diabetes, as well as aesthetic or cosmetic treatments, use of anticoagulants, corticoids or systemic and/or topical anti-inflammatory drugs in the last six months were excluded.
Three-dimensional Digital Photogrammetry was performed with a digital skin analyzer model EH-900U from Shenzhen Legend Beauty Equipment Co., Ltd. Guangdong, China (figure 12), for the volume, height, depth, surface, perimeter and roughness quantification analysis module, for three-dimensional photometry of skin micro relief. The collection was performed by demarcating the treatment quadrant of the middle third of the face with an area of 6 cm2 below the lacrimal rim on each side (Figure 13). The photos were collected in the 1st and 2nd treatment sessions. Dermaplaning protocol was performed with scalpel handle n.03 model Cooperflex Prime, registration ANVISA n. 80756530004, manufactured by Allen Surgical Co. and model 10R disposable stainless steel scalpel blade, registration ANVISA 10302860096, manufactured by Swann Morton Limited, England and imported by H. Strattner e Cia Ltda.
The cutaneous microrelief measurements were categorized into two possibilities, positive or negative, according to the following criteria: 1) skin thickness 2) cutaneous invaginations 3) cutaneous interreflections and 4) correlation of secondary and tertiary lines of the two-dimensional image (Figure 1). After this analysis, it was nominally defined as positive for images presented with evidence of two or more of the criteria and negative for evidence of only one or none of the criteria listed above. For statistical analysisFrom the cutaneous microrelief, we set up a contingency table and, from it, we tested the proportion of variables using Fisher's exact test. We considered statistically significant differences for tests with p<0.05. Microsoft Excel version 2107 was used for data tabulation and GraphPad Prism 5.01 for tests and graphs.
The qualitative analysis record of the three-dimensional image was performed through visual comparison before and after the placebo and treated groups, during observation in the standard reference base of cutting the 3D image for the axes x=3.0, y=2.0 and z=1.0 and after this analysis, it was nominally defined as positive for images presented with evidence of two or more of the criteria and negative for evidence of only one or none of the criteria listed above (Figure 1, 2). Thus, negative and positive nominals were converted to the ordinal value = 0 for negative cases and value = 1 for positive cases and recorded in the tables for sum and correlation of results after the first and second treatment session (Table 1, 2).
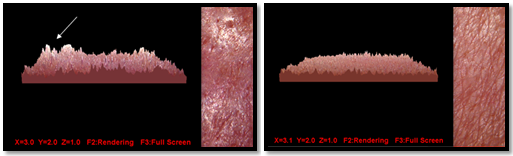
Figure 1,2 Correlation of the qualitative analysis of the 3D image for positive or negative respectively in relation to the cutaneous microrelief after two treatment sessions.
|
Data analyzed - 1st session |
Negative |
Positive |
Total |
|
Placebo |
18 |
4 |
22 |
|
Treated |
6 |
16 |
22 |
|
Total |
24 |
20 |
44 |
Table 1 Record of the 3D image qualitative analysis for negative and positive cases, in relation to changes in the skin microrelief after the first treatment session
|
Data analyzed - 2nd session |
Negative |
Positive |
Total |
|
Placebo |
8 |
14 |
22 |
|
Treated |
5 |
17 |
22 |
|
Total |
13 |
31 |
44 |
Table 2 Record of the 3D image qualitative analysis for negative and positive cases, in relation to changes in the skin microrelief after the second treatment session
On the findings of this study on the comparison of the 3D image of the cutaneous microrelief between the groups, after visual qualitative analysis, and converted in ordinal form, the Fisher test was performed and found p-value equal to 0.007 after the first session (Figure 3) ep value equal to 0.5098 after the second session (Figure 4), concluding that there was a difference between the groups only after the first Dermoplaning session.
Dermaplaning is a technique already described in the literature, as a form of physical exfoliation of the superficial layers of the skin, carried out by dragging a sterile and disposable blade of a scalpel, which can be used in aesthetic protocols aimed at facial rejuvenation and the treatment of scars. and acne sequelae to improve skin microrelief.7 The positive change found after the first Dermaplaning session in the cutaneous microrelief suggests that the physical exfoliation performed by the blade can interfere with the response of the skin's fibrous cells and contribute to the improvement of the cutaneous microrelief, and the three-dimensional images collected in this work, corroborating with the findings of Rigde et.al. carried out in 1966, on the evidence of the relationship between the mechanical properties of the skin and its microrelief structure. Therefore, it is worth noting that we observed that the findings were not progressive and that the findings of the second session were not as positive as those of the first session, which may suggest that the interval between sessions in this study was shorter than the average time of the process. of normal epithelization and may lead to situations of excessive thinning of the surface layers of the skin, interfering with its microrelief orimpairment of the skin barrier function and the natural process of shedding and shedding of surface cellsof the skin.10–14
This work was important to verify that there are changes in the cutaneous microrelief after the use of dermaplaning and opens perspectives for new future studies about image markers and cutaneous microrelief that can demonstrate new findings about the possible benefits of this technique, as a non-negotiable resource. invasive and low cost, to be included in the routine of aesthetic and dermatological facial treatments.
None.
Authors declare that there is no conflict of interest exists.

©2023 Ventura, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.