eISSN: 2471-0016


Case Report Volume 1 Issue 1
1Department of Pathology, Saint Louis University School of Medicine, USA
1Department of Pathology, Saint Louis University School of Medicine, USA
2Division of Gastroenterology and Hepatology, Saint Louis University School of Medicine, USA
2Division of Gastroenterology and Hepatology, Saint Louis University School of Medicine, USA
Correspondence: Jinping Lai, Department of Pathology, Saint Louis University, 1402 South Grand Boulevard, St. Louis, MO 63104, USA, Tel +1 314-577-8475
Received: January 01, 1971 | Published: June 17, 2015
Citation: Jin-Ping L, Quintana AR, Vuong G. Gastric pseudomelanosis (report of a case and review of literature). Int Clin Pathol J. 2015;1(1):90–12. DOI: 10.15406/icpjl.2015.01.00003
Gastric pseudomelanosis is exceedingly rare. To the best of our knowledge, there have been only six reported cases in the literature of gastric pseudomelanosis. We report a case of an 86 year-old woman with marked iron deficiency anemia who was found to have characteristic speckled pattern of grey-black pigmentation on endoscopic examination. Histologically, the gastric biopsy revealed characteristic aggregates of sub epithelial macrophages with coarse brown-black pigment present within the lamina propria. This pigment had focal and patchy positive staining for iron. These changes were consistent with pseudomelanosis. The previously reported six cases had similar clinicopathological features. Although the exact pathogenesis of gastric pseudomelanosis is unknown, it is benign and has not been associated with malignant transformation or worsening of any underlying medical conditions.
Keywords: gastric pseudomelanosis, subepithelial pigmented macrophages, severe mitral regurgitation, hypertension, mild coronary artery disease
Pseudomelanosis is a rare benign condition characterized by pigment deposition within subepithelial macrophages in the lamina propria, typically in duodenal mucosa. Rare cases have been reported in gastric mucosa. It can occur at any age and has been reported in association with upper GI bleeding, chronic renal failure, hypertension and diabetes mellitus. To the best of our knowledge, only six cases have been reported. We describe the clinicopathological features of an interesting case with similar features as the six cases previously described and a review of the literature to better understand this rare entity.
An 86 year old with a history of stage III chronic kidney disease, hypertension, atrial fibrillation, mild coronary artery disease, severe mitral regurgitation, iron deficiency anemia without overt bleeding, and rheumatoid arthritis was admitted to our institution for syncope. The patient complained of occasional right lower quadrant pain that resolved with lying flat, however denied changes in appetite or weight loss. She was on chronic iron therapy and stated that her stools were usually black in color. The patient’s outpatient medications included coumadin, hydralazine, cyanocobalamin (Vitamin B12), metroprolol, ferrous sulfate, famotidine, calcium acetate, folic acid, levothyroxine, prednisone, simvastatin and tramadol.
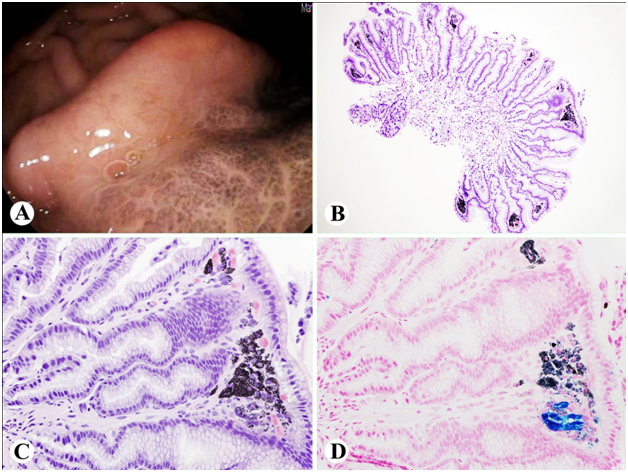
GI was consulted for marked anemia (Hemoglobin of 6.8 g/dL). Upper GI endoscopy was done to evaluate her marked iron deficiency anemia and showed a few localized small erosions in the gastric body. There was no stigma of recent bleeding. However, in the greater curvature of the gastric body there was a localized mucosal abnormality characterized by darkly pigmented discoloration that “did not wash off” (Figure 1A). Biopsies were taken with a cold forceps for histology. The duodenum appeared normal.
Histologically, the gastric biopsy revealed characteristic subepithelial pigment deposition. Aggregates of subepithelial macrophages with coarse brown-black pigment were seen within the lamina propria (Figure 1B-1C). This pigment had focal and patchy positive staining for iron (Figure 1D). These changes were consistent with pseduomelanosis.
Due to the benignity of gastric pseudomelanosis, this lesion was not further evaluated for. The syncopal episode was determined to be orthostatic which responded to IV fluids. The patient was also transfused 2 units of PRBCs and discharged with uneventful follow up.
Only 7 cases of gastric pseudomelanosis have been reported to our knowledge, including this current case. In the seven reported cases, all but one patient was female (The gender of one patient was not given in the literature). The ages ranged from 60 to 86 with an average age of 73.4 years. In the seven reported cases, all patients suffered from multiple medical problems (One case report did not discuss comorbidities). Of the cases with known comorbidities, common medical problems included chronic renal insufficiency, anemia and hypertension. All patients were taking ferrous sulfate and at least six of the seven patients were on an antihypertensive medication. In all cases the endoscopic findings showed dark pigmentation in the gastric mucosa corresponding to subepithelial pigmented macrophages histologically.1-6 No evidence of malignant transformation or worsening of any underlying medical conditions was reported (Table 1). Although gastric pseudomelanosis is a rare entity, physicians should be aware of it to facilitate a prompt diagnosis and avoid unnecessary testing.3
Case |
Age |
Sex |
Comorbidities |
Medications |
Clinical Presentation |
Endoscopic Findings |
Histologic Findings |
Follow Up |
Weinstock LB et al.1 |
74 |
Female |
Chronic renal insufficiency (Creatinine 4.6 mg/dL), anemia |
Ferrous sulfate |
Asymptomatic |
Dark pigmentation of the antral mucosa |
Presence of iron sulfide granules in the lamina propria, confirmed by Prussian blue stain |
Unknown |
Rustagi T et al.2 |
60 |
Female |
Chronic kidney disease, hypertension, iron deficiency anemia, coranary artery disease, type 2 diabetes mellitus, hypertension |
Ferrous sulfate, hydralazine, furosemide, carvedilol, clopidogrel, insulin |
Hypertensive urgency and intermittent nausea and vomiting for 2 days |
Patchy erythema in the antrum with thick mucosal folds and a diffuse peppered gray-black pattern in the stomach |
Aggregates of macrophages with coarse black-brown cytoplasmic pigment within the lamina propria |
No further episodes of vomiting and was discharged with uneventful follow-up |
Kibria R et al.3 |
79 |
Female |
Hypertension, congestive heart failure, iron deficiency anemia |
Ferrous sulfate, furosemide, carvedilol, bupropion, escitalopram |
Postprandial epigastric pain and early satiety for 2 months, along with 10 lb weight loss |
Dark pigmentation of the pylori antral mucosa; the remainder of the gastric mucosa appeared normal |
Prussian blue stain indicated hemosiderin deposition |
Unknown |
Alraies MC |
83 |
Female |
Diabetes mellitus, hypertension, coronary artery disease, hypothyroidism, chronic renal failure |
Ferrous sulfate, furesamide, hydralazine, Hydrochlorothiazide, isosorbide mononitrate, levothyhroxine, esomeprazole, atorvastatin, insulin, metoprolol, diltiazem and aspirin |
Epigastric pain for 1 day with black stool |
Speckled pattern of black pigmentation seen throughout the stomach and duodenum |
Pigment in stromal macrophages ; iron staining (Perl’s) was negative for the presence of iron sulfide granules in the lamina propria |
No recurrent bleeding and discharged with uneventful follow-up |
Ochoa Palominos A et al.5 |
60 |
Male |
Hypertension, ischemic heart disease, idiopathic retroperitoneal fibrosis, chronic kidney failure, iron deficiency anemia |
Ferrous sulfate, furosemide, doxazosin, atenolol, acenocoumarol |
Rule out esophageal-gastric varices |
Multiple millimeter coffee-colored lesions in the gastric body, duodenal bulb and second portion of duodenum |
Blackish-brown deposits within the lamina propria macrophages. |
Uneventful follow-up |
Antaki F |
73 |
Unknown |
Unknown |
Ferrous sulfate, hydralazine |
Dysphagia |
Dark pigmentation of the gastric mucosa inside a small hiatal hernia |
Pigment deposition at the level of the lamina propria |
Unknown
|
Quintana A |
86 |
Female |
Hypertension, chronic kidney disease, iron deficiency anemia, Afib, coronary artery disease |
Ferrous sulfate, hydralazine, famotidine, cyanocobalamin, metroprolol, folic acid, levothyroxine, prednisone, simvastatin and tramadol |
Severe anemia and syncope |
Gastric greater curvature with darkly pigmented discoloration that “did not wash off” |
Subepithelial coarse brown-black pigmentation deposition in macrophages; patchy positive for iron |
Discharged with uneventful follow-up |
Table 1 Clinical pathologic findings in the six reported cases and current case of gastric pseudomelanosis
The exact pathogenesis and etiology for pseudomelanosis is not clear, however it has been associated with hypertension, chronic kidney disease, anemia, diabetes mellitus and gastrointestinal bleeding.1,2,5 Many common medications including antihypertensive drugs such as hydralazine and furosemide, propranolol, methyldopa, thiazides and iron sulfate have been implicated in pseudomelanosis. Although no definite etiology or mechanism has been identified, it is thought that the large size of the particles that cause pigmentation are difficult to absorb and subsequently cause pigmentation deposition.5 Hydralazine, furosemide and hydrocholorthiazide contain sulfur, which has been postulated to promote deposition of pigment in the duodenum.2
The classic endoscopic findings of pseudomelanosis of the gastrointestinal tract are discrete, flat, black or brown speckled pigmentation of the gastric, duodenal, and jejunal mucosa. In the present case, only the stomach was involved. Histologic examination is necessary for diagnostic confirmation and to exclude other conditions associated with deposition of pigment seen endoscopically such as post-hemorrhagic deposition of hemosiderin, hemosiderosis/hemochromatosis, metastatic melanoma and substance ingestion such as charcoal or barium sulfate.2 Microscopically, the pigment is located subepithelially in mucosal macrophage lysosomes, but can also be found in extracellular space or in epithelial cells. Various ancillary histochemical stains can be utilized to help characterize the pigment, including Masson-Fontana stain and Perls’ Prussian blue stain. Iron stains are typically negative or only focally positive. In the current case, Prussian stain is focally positive for iron deposition.
The pigment in hemosiderosis/hemochromatosis is finely granular, brown to black particles in epithelial cells which stain diffusely positive for iron. In advanced iron overload disorders, iron is deposited in parenchymal cells throughout the body, including the parietal cells in the stomach. Studies have shown that the pigment of pseudomelanosis is composed of a mixture of ferrous sulfide, ferrum sulfate, lipomelanin, hemosiderin, ceroid, pseudomelanin, lipofuscin and lipofuscin-like pigment. The deposited pigment can also contain aluminum, calcium, magnesium, potassium, sulfur, silica, and silver.1,2 As mentioned previously, histochemical stains can be utilized to help characterize the pigment, including Masson-Fontana stain and Perls’ Prussian blue stain. Because the pigment is made up of a mixture of pigments, iron stains are typically negative or only focally positive. It is important to note that Prussian blue stain can give a false-negative reaction if ferrous oxide is present instead of ferrous sulfide.
None.
The author declares no conflict of interest.

©2015 Jin-Ping, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.