eISSN: 2373-6372


Review Article Volume 15 Issue 4
Federal University of Minas Gerais, Postgraduate Program in Sciences Applied to Surgery and Ophthalmology, Brazil
Correspondence: Ana eloiza Verônica Machado, Federal University of Minas Gerais, Postgraduate Program in Sciences Applied to Surgery and Ophthalmology, Brazil
Received: August 25, 2024 | Published: September 3, 2024
Citation: Machado AV, Sander BQ, Aberti LR, et al. Weight loss and reduction in the risk of cardiovascular diseases in patients undergoing gastric end suture with the use of overstitch ® for a period of 12 months. Gastroenterol Hepatol Open Access. 2024;15(5):96‒119. DOI: 10.15406/ghoa.2024.15.00587
The objective of this study is to analyze weight loss and risk reduction of cardiovascular diseases in patients undergoing endoscopic gastroplasty over a 12-month period. The research methodology adopted was a retrospective study with patients from the center participating in the research to treat obesity and with clinical indication for the procedure, from January 2021 to January 2022, meeting the inclusion criteria: minimum age: 18 years old, Minimum BMI of 30 kg/m2 (grade I obesity) and also patients who have already undergone bariatric surgery in the past and gained weight again (gain of at least 10% of the minimum weight achieved after bariatric surgery). The results obtained demonstrate that in month 1, the average weight was 114.1 kg, while in month 12 it was 82.3 kg, a reduction of approximately 27.86% (P < 0.001), observing a trend of progressive reduction from 1.5 kg to each month There was an average reduction of 28.11% in BMI over the 12 months (P< 0.01). As for the average WHR index, it also demonstrated a reduction, which allows us to affirm an improvement in the cardiovascular risk of patients who participated in this study (P< 0.01). The percentage of non-obese patients increased significantly from 0% to 16.28%, while the percentage of patients with Grade 2 and Grade 3 obesity decreased from 44.83% to 6.98% and from 48.28% to 1.16 %, respectively. This suggests a significant change in the distribution of patients' BMI throughout the study. It was concluded that endoscopic gastroplasty proved to be safe as it did not present complications or complications and was efficient for weight loss and the risk of cardiovascular diseases in patients over a period of 12 months.
Keywords: Obesity, endoscopy, weight loss, cardiovascular diseases, endoscopic suture.
ANVISA, National Health Surveillance Agency; BIG, Intragastric Balloon; CC, Waist circumference; CREMESP, Regional Council of Medicine of São Paulo; ESG, Endo Gastric Suture; USA, United States of America; FMABC, ABC Faculty of Medicine; GREP, Primary Endoscopic Reduction Gastroplasty; GRES, Secondary Endoscopic Reduction Gastroplasty; HAS, Systemic arterial hypertension; BMI, Body Mass Index; MBE, Evidence-Based Medicine; MO, Operations Manual; NIH, National Institutes of Health; WHO, World Health Organization; PSI, Psychology; WHR, Waist-Hip Ratio; SBCBM, Brazilian Society of Bariatric and Metabolic Surgery; SUS, Unified Health System; UERJ, State University of Rio de Janeiro
Obesity is a chronic disease characterized by excessive accumulation of body fat and is determined by a Body Mass Index (BMI) above 30 kg/m2. Obesity is caused by an intake of calories that exceeds the body's daily expenditure and its treatment involves several approaches, including: nutritional, use of anti-obesity medications and physical exercise. The simplest form of treatment is the adoption of a healthier lifestyle, with lower calorie intake and increased physical activity, however, several patients do not respond to these types of treatment, requiring a different intervention.1
According to Ferreira et al.,2 obesity can be classified as the accumulation of fatty tissue located throughout the individual's body, which may be caused by genetic, endocrine-metabolic diseases or nutritional changes. Obesity can be classified as exogenous and endogenous. Exogenous obesity is due to excess food intake, early weaning, sedentary lifestyle, introduction of solid foods from a very early age, complications in family relationships, replacement of meals with snacks and difficulties in interpersonal relationships.
Ribeiro et al.3 explain that exogenous obesity occurs due to external and non-organic causes, such as advanced Tanner stage, height outside family standards, advanced bone age and cases of obese people in the family. The factors that cause exogenous obesity are also linked to the fact that parents are obese, which increases the possibility of children with the same problem, and individual factors such as increased appetite.
The World Health Organization (WHO) identifies obesity as one of the biggest public health problems in the world. In 2015, more than 1900 million adults, over the age of 18, were identified as overweight, of which more than 600 million were obese.4 Projections indicate that by 2025 there will be approximately 2.3 billion overweight adults, and more than 700 million with obesity. In Brazil the situation is no different.
The latest survey of data related to obesity, released by the Ministry of Health through the VIGITEL program, warns that excess weight already affects 52.5% of the country's adult population. It is important to highlight that the growth rate of excess weight increases every year, and in the last decade, the real increase was 23% in the period.4-6
Non-surgical methods to help reduce weight in the short term are diet, medication, exercise, in addition to the use of endoscopic devices such as the intragastric balloon (BIG).7 It should be noted that in recent years the use of BIG has stood out as the main current endoscopic alternative due to being a non-invasive method, with low risks for weight loss and which meets the recommendations of the National Institutes of Health (NIH) in that weight losses of 5 to 10% of initial body weight produce health benefits, preventing an increase in the number of morbidly obese people and reducing mortality.8,9
ESG has been a reality in the world and in Brazil, although it is still relatively recent. Regarding this, Brunaldi (2018) describes it as a method also adopted with the purpose of reducing the diameter of the gastrojejunal anastomosis 1in patients with post-bypass weight regain. It is a technique performed by applying stitches around the gastrojejunal anastomosis with the help of a suture device that is placed next to a gastroscope.
The ESG is a technique that emerged in Brazil in 2017, as an innovation for reducing overweight and treating obesity, known as endoscopic gastroplasty. Worldwide, more than 10,000 people have already undergone the procedure with good results and low rates of complications. This technique is relatively simple, as it is non-surgical, with discharge on the same day, quick recovery (2 to 3 days) and an average execution time of approximately 40 minutes.10,11
According to Magalhães et al.,12 OverStitch ® in Brazil is a device that has already been approved by the National Health Surveillance Agency (ANVISA) for use, as well as receiving official recognition by the Regional Council of Medicine of São Paulo (CREMESP). In 2016, after approval by the Research Ethics Committee at the Faculdade de Medicina do ABC (FMABC) in Santo André, Professors from the aforementioned faculty carried out studies and research with the aim of evaluating the results that ESG presented in Brazilian patients.
According to Sander,13 ESG is characterized as a safe method which uses a device called Overstitch © which, when placed next to the endoscopy device, has the capacity to perform the endoscopic stomach suture procedure, achieving an estimated reduction of more than 60 % of its distensibility and diameter. This fact, in turn, results in a decrease in its volume. Figure 1 illustrates the U-shaped suture in the ESG procedure using Overstitch © .
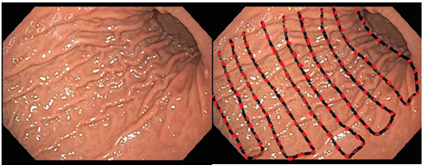
Figure 1 Photo of the stomach (left) and schematic representation of the U-shaped suture in the ESG procedure using Overstitch© (right).
Source: Sander (2022)
It is also possible to observe, through Figure 2 proposed by Sander,13 the Overstitch© on the endoscopy device handle, the needle at the tip of the equipment and the complete set.

Figure 2 Overstitch© on the endoscopy device handle (left) the needle mounting system on the tip (middle) and the assembled equipment (right).
Source: Sander (2022)
In general, Magalhães et al.12 explain that weight reduction through ESG using OverStitch ® occurs by reducing the gastric chamber, without necessarily needing to perform a surgical procedure or any type of external incision. However, it is necessary to observe the patient's evolution in the first six months after the procedure, as this is a period in which possible cardiovascular risks may arise, such as hypertension, congenital heart disease, acute myocardial infarction, cardiac arrhythmias.
Based on the contextualization presented, this study seeks to answer the following research problem: What is the weight percentage and risks of hypertension, congenital heart disease, acute myocardial infarction, cardiac arrhythmias that patients undergoing endoscopic suturing (overstitch ®) face? Can you lose in a 12 month period?
Justification
Carrying out a study on the topic in question is of significant importance to the academic and civil community, given that the proposal to reduce weight through ESG It is still a relatively new alternative in Brazil and little known. Added to this, there is a real need to combat obesity, as it is an anomaly responsible for around 300,000 deaths per year in the country and, when analyzed from the perspective of the added burden of diseases associated with obesity, the increase in mortality is even greater.14
As a consequence, it becomes important to highlight the economic impact on public health, the annual global costs of its treatment exceed thirty-two billion dollars.4 In Brazil, a study developed by the State University of Rio de Janeiro (UERJ) analyzed the direct costs associated with outpatients and hospitalized patients with diseases related to overweight and obesity. The annual cost was R$3.57 billion in 2010, with R$1.15 billion for outpatient care and R$2.38 billion for hospital care.15
It is possible to see that obesity is a problem that, according to Batista, Mondini and Jaime,14 affects a large number of people worldwide and has been considered one of the main Public Health problems in Brazil and the world, causing negative impacts on 1 in every 5 individuals in the United States, for example. For Klobukoski and Hofelmann,16 the prognosis of obesity has still been somewhat unclear, as, in some cases, it has been observed that obese children can become obese adults. While there are obese adults who were of ideal weight for their age and height in childhood and youth. However, it can also be noted that the younger the age of the child in which obesity manifests itself and the greater the intensity, the greater the possibility of becoming an obese adult.
As mentioned, the prevalence of obesity is continually increasing in Brazil and around the world, which can trigger several comorbidities in obese individuals, in addition to negatively impacting their quality of life. And, in this context, in addition to the options already existing in the fight against obesity (medicines, bariatric surgery, etc.), an innovative option is on the market, ESG, which, already in use in countries like the United States, has proven itself safe and effective in its proposed objective, which is weight reduction in obese patients.
Endoscopic suturing using OverStitch ® aims to reduce stomach capacity through endoscopy (Primary Endoscopic Reduction Gastroplasty - GREP), review and correction of previous bariatric surgeries (Secondary Endoscopic Reduction Gastroplasty - GRES) and treatment of bariatric surgery complications: early (fistulas) and late (widening of the anastomosis performed with weight regain),17 a fact that justifies the choice of the topic “analysis of weight loss and risk of cardiovascular diseases in patients undergoing endoscopic suture using overstitch ® over a period of 12 months”.
Based on the above, carrying out this work is also justified due to the high prevalence of obese people in everyday life, whose quality of life is impaired and need to undergo treatment. It also has social relevance in the sense of seeking to demonstrate the importance of treating obesity in an attempt to raise awareness among the entire population about the need and relevance of combating this problem with the use of ESG with overstitch ®.
Objective
Analyze weight loss and risk of cardiovascular diseases in patients undergoing Endo Gastric Suture using overstitch ® over a period of 12 months.
1 An important part of the operation not only because it is related to the fistula, considered the main and most serious complication of the surgery, but also because of its possible relationship with weight loss.
Obesity
Among the problems that present a high mortality rate in Brazil, there is obesity, responsible for approximately 300,000 deaths per year, and this number can increase when associated and analyzed from the point of view of diseases resulting from this anomaly, such as heart disease.4 Furthermore, it must be added to the fact that public health suffers constant impacts in relation to costs.
Brazilian data, for example, indicate that people with obesity represent high expenditure on health services. Therefore, associating obesity with cardiovascular diseases allows for a more complete estimate of the economic impact on the Unified Health System (SUS). With the introduction of the costs of obesity in the public health service as a risk factor for comorbidities such as diabetes and hypertension, for example, obesity can be attributed to total costs of R$669 million in hospitalizations and outpatient costs and R$722 million in spending on medicines, therefore totaling R$1.39 billion in 2018 alone.18
According to Batista, Mondini and Jaime,14 it is estimated that worldwide, more than 250 million people are obese with progressive increases in its prevalence, obesity is considered one of the main public health problems and is a disease that has affected one in five children in the United States.
The definition given by the World Health Organization (WHO) for obesity is as excess body fat that a person has in an amount that causes health problems. Normally, a person with a Body Mass Index (BMI) equal to or greater than 30 kg/m2 is considered obese, with a normal weight range considered between 18.5 and 24.9 kg/m 2.19
According to Ghoorah et al.,20 in 1998, a meeting was held in the United States of America (USA) by the National Institutes of Health (NIH – Instituto Nacional de Saúde in free Portuguese) to discuss obesity and its related problems. With the aim of creating guidelines aimed at health professionals regarding the risks associated with being overweight as well as possible treatments based on Evidence-Based Medicine (EBM). Among the recommendations that emerged in this debate, there is the fact that health professionals explain to obese patients the need and importance of reducing weight by at least 10% of total body weight through non-surgical alternatives in up to six months and, only then, recommend invasive measures.
The reason why this weight reduction of at least 10% of body weight was included in the guidelines, according to Van et al.21 is justified to ensure that there is a significant reduction in the risks of the emergence of diseases associated with obesity. Furthermore, it is also a way of inducing the patient to adopt a healthier lifestyle, starting with dietary re-education and, consequently, their total weight. For Van et al.,21 such factors jointly contribute to increasing the probability of successful weight reduction in the long term.
As illustrated by the Brazilian Society of Bariatric and Metabolic Surgery (SBCBM),22 Brazil is the country with one of the highest rates of obese individuals in the world. In 2022 alone, the number of obese people reached 863,083. Through Figure 3 it is possible to highlight obesity in Brazil.
Van et al.21 also explain that the guidelines created by the NIH were well accepted even by clinics and hospitals that, before carrying out bariatric surgeries, ask the patient to lose weight by at least 10% of the initial weight or 25% of the excess weight. Although it is public knowledge that obesity is a growing, recurrent and epidemic public health problem, what is notable is that its treatment appears to remain a clinical problem of high complexity, difficult and of great importance, as it is a multifactorial disease.
According to WHO,4 obesity is commonly a problem that is traditionally treated based on physical exercise, functional training, diets, behavioral guidance, psychological guidance and the administration of drugs to reduce appetite. However, these are approaches that, while still able to reduce the individual's weight, are not capable of maintaining long-term results.
There are a variety of alternatives that exist to treat excess weight and obesity, which are generally not isolated, but rather a combination of two, three or more of these alternatives. Regardless of the professional's indication or the patient's preference, all treatments have advantages and disadvantages that must be considered when choosing, as each type of treatment will depend on a variety of factors based on clinical parameters.4
Regardless of the treatment chosen, the diet is considered an inexorable part and is recommended for all patients, both to reduce total calorie intake and to practice healthy eating habits. For Garner and Wooley,23 it is necessary to point out that in addition to diet, the recommendation to practice physical activities has also been common, always taking into account the capacity and physical reality of each patient. However, for patients who wish to lose weight without invasive procedures, it is important to understand that diets and physical activity, whether isolated or combined, have high failure rates, which can vary from 90 to 98%.
The numerous failed attempts to reduce weight along with the problems of obesity may be due to the delay in obtaining results and patients remaining overweight, exposed to the risks associated with obesity. Therefore, the individual who decides, by their own decision, not to lose weight is already exposing themselves to risks.24
Regarding drug administration, Omran24 explains that pharmacotherapy is capable of providing the individual with rapid weight loss, depending on the case, however, there may be a greater risk of side effects. Not just side effects, there are also medications that are contraindicated for certain patients, such as hypertensive patients, for example. However, in relation to surgery, the selection of patients to undergo bariatic surgery requires at least five years of obesity evolution, together with the history of failure of conventional treatment.
Considering that obesity is a serious public health problem, Abeso25 describes that according to WHO data, it is estimated that by the year 2025 there will be approximately 2.3 billion overweight adults worldwide and, of these, 700 million are obese, that is, with a BMI greater than 30. In Brazil alone, there was an increase of 20.3% from 2006 to 2019.
According to Ferreira et al.,2 obesity as a health problem can be classified as the accumulation of fatty tissue present throughout the individual's body, capable of presenting as causes, nutritional changes, genetic anomalies, tiredness and endocrine-metabolic problems. Obesity is considered a chronic disease accompanied by several complications.
Obesity is also a problem that can cause a variety of complications for the affected person. According to Macedo et al.,26 there are three factors to be taken into consideration in body composition related to the emergence of chronic degenerative diseases. Such factors are the total amount of fat, excess fat in the trunk or abdominal region and excess visceral fat.
For Reis and Biagiotto,27 people, in general, from an early age, are from a psychological, socioeconomic and cultural point of view, very vulnerable, as they are influenced by the lifestyle habits of their family, the eating customs of the community where they live. They are inserted, with greater ease with food, and their attitude is a reflection of the environment in which they live. When unfavorable, the environment may provide conditions that lead to the development of eating disorders leading to obesity, which may persist if changes are not made in this context.
Sartori-Cintra, Aikawa and Cintra28 point out that for cases of obesity, there are some forms of treatment, including diet, physical activity, natural remedies and drugs, and, in some cases, when obesity is considered severe, bariatric surgery is recommended to reduce the stomach or the old bariatric surgery by endoscopy, currently known as endoscopic suture, described for the first time in 2013.
Treatment alternatives against obesity
Regarding treatment alternatives against obesity, Ravelli et al.29 state that it is necessary to initially observe the individual's general health conditions, as well as their motivation to lose weight. Among the types of treatment against obesity, one can count, among others, a combination of diet, physical activity, behavior change, natural remedies and weight loss drugs and, in certain situations, when obesity is considered severe, it is recommended bariatric surgery to reduce the stomach.
Schakarowski et al.30 state that there are several types of treatment in addition to those mentioned above, but care and the choice of the most appropriate option for treating obesity need to be established as soon as the diagnosis of obesity is made. Regarding conventional treatment, Schakarowski et al.30 observe that it is based on a decrease in caloric intake, an increase in energy expenditure, changing behavior and family involvement in the change process. This treatment is long-term.
Regarding dietary treatment, Carvalho and Rosa31 explain that it is necessary to focus on adapting caloric intake and providing nutritional needs for each age. It is important that the caloric proportion of macronutrients correctly follows the recommendations of national and international healthy eating guidelines.
Regarding the practice of physical activity for the treatment of obesity, Moreira et al.32 explain that there is no precise proof of exactly what the most correct prescription would be for this case. Whether for adults, children or teenagers, what we actually have is a big debate about what would be the appropriate intensity, duration and frequency for exercise.
Carvalho and Rosa31 point out that behavioral change is highlighted in many weight loss programs not only for adults, but also for children and adolescents. The purpose of behavioral treatment is to help recognize and modify incorrect habits to maintain a healthy weight.
Bariatric surgery
According to Godoy et al.,33 individuals with grade III obesity have an association with worsening quality of life, in addition to a high frequency of comorbidities, decreased life expectancy and the high possibility of failing less invasive treatments against obesity.
For Younes, Rizzotto and Araujo,34 the treatment of severe obesity through bariatric surgery has been adopted for almost 50 years, beginning in the 1950s with operations that caused malabsorption, forgotten at the end of the 1950s. 1970 because of the serious and frequent undesirable results it caused in the patient, such as, for example, vomiting, diarrhea, dehydration, liver problems, abdominal pain and cirrhosis.
Still according to the same authors mentioned above, among the surgical techniques for the treatment of obesity that has possibly been the most adopted throughout the world is Fobi-Capella. It is a mixed, restrictive and malabsorptive procedure, in which the patient's stomach is separated into two compartments using staplers. In this case, the remaining stomach will have a volume of 30ml to 50ml, being connected to a part of the small intestine and the largest portion of the stomach remains outside the food transit.
However, Steyer et al.35 emphasize that surgical treatment against obesity should only be indicated in cases where there is a risk of the individual remaining obese, exceeding the short and long-term risks of bariatric surgery.
Regarding the criteria for choosing the patient, Younes, Rizzotto and Araujo34 state that they involve a body mass index (BMI) equal to or greater than 40kg /m² or above 35kg/m² related to comorbidity, capable of decreasing with the loss of weight; the various attempts that the patient has already made to lose weight and have not achieved any results and; the psychological conditions to comply with dietary guidance in the postoperative period.
Moreira et al.32 state that the end of surgery does not mean the end of obesity treatment. In fact, it is the beginning of a change and adaptation regarding eating behavior and physical activities, and must be regularly monitored by a multidisciplinary team of health professionals.
For Moreira et al.,32 when bariatric surgery is performed using the Fobi Capella technique 2, the patient can experience a total loss of up to 75% of excess weight during one year. However, it is very important to perform surgery to treat morbid obesity, as it allows weight reduction and even completely eliminates the main comorbidities associated with excess weight, introducing improvements in the patient's quality of life.
The option to perform bariatric surgery, according to Steyer et al.,35 it has been one of the most effective alternatives for the treatment of morbid obesity, as it presents quick and lasting results compared to other existing therapies. Agreeing with the authors above, Moreira et al.32 indicate that bariatric surgery has effectively been the most viable and effective option for treating morbid obesity. However, for it to present the desired results, it is important that an adequate pre-surgical psychiatric evaluation is carried out for diagnosis. Early correct treatment of a previous eating disorder must also be carried out.
Bariatric surgery techniques
According to Mariano, Monteiro and Paula,36 there are different surgical techniques for treating obesity, which are called bariatric surgery. This surgery is basically based on four types of techniques, which are restrictive, malabsorptive, mixed and pacemaker.
Restrictive techniques
Regarding restrictive techniques, Ribeiro et al.3 emphasize that this is an alternative that aims to reduce the volume capacity of the patient's stomach, causing a feeling of satisfaction with ingesting just a small amount of food. For the authors, among the restrictive techniques, the most adopted are the non-surgical intragastric balloon, vertical sleeve gastroplasty and the laparoscopic adjustable gastric band.
About the Sleeve, it is a bariatric technique that presents better results when it comes to patients with morbid obesity and comorbidities, especially in relation to brown skin and a reduction in health problems that are associated with obesity. This technique consists of removing part of the stomata, the left part, causing a reduction in its capacity to store food.
According to Manegoto et al.,37 the application of the intragastric balloon precedes of surgical intervention. It is made with silicone and has a volume of 500 to 800 ml of aqueous material, occupying proportional space, bringing early satiety to the patient. After being placed inside the stomach, the balloon is inflated using the endoscopic method and remains in place for up to 12 months.
As for the laparoscopic adjustable gastric band, the authors state that it is a technique that consists of an inflatable silicone band that is applied laparoscopically to the upper part of the individual's stomach. Subsequently, the narrowing is done to generate a small proximal gastric chamber that connects with the distal portion of the rest of the stomach through a passage opening adjustable by the inflation level of the band. The best known are the Mason technique and the gastric band.
The Mason Technique, according to Ribeiro et al.,3 is seen as a milestone in obesity surgery. The gastric band, according to Manegoto et al.,37 it is in the form of a ring made of silicone, which is used to wrap around the upper part of the individual's stomach. It is inflated through a small needle, using a reservoir that is positioned under the skin.
Malabsorptive technique
According to Steyer et al.,35 the malabsorptive technique proposes leaving the stomach to provide a large intestinal diversion. With this technique, the patient continues to eat normally, in the same quantity, however, there is reduced absorption of food.
According to the authors, the malabsorptive technique has as its main representative the jejuno-ileal diversion and includes the exclusion of practically the entire patient's small intestine, maintaining only 35 cm of the proximal jejunum and 10 cm of the distal ileum in the food passage.
Mixed technique
Mixed technique is a modality that, according to Schakarowski et al.,30 combines the two previous principles (restrictive and malabsorptive) promoting a reduction in the patient's stomach and a small intestinal diversion, causing a decrease in food intake associated with a slight reduction in their absorption.
This mixed technique has been considered to be the most balanced and appropriate standard for bariatric surgeries, and according to Pedrosa et al.,36 the Capela technique and the Fobi-Capela technique. Still for these authors, the Fobi-Capella surgery it is the technique of vertical gastroplasty with gastric bypass that is normally the most used. This technique consists of separating the remainder of the stomach, the proximal gastric chamber coupled to the cardia with a capacity of 20 to 30 ml. In this way, the largest part of the stomach is out of food transit, meaning there is a reduced malabsorptive component.
Gastric pacemaker
Regarding the technique known as gastric pacemaker, Carvalho and Rosa31 emphasize that it involves the implantation of an electrical stimulator in the external wall of the patient's stomach that sends the sensation of early satiety to the brain. However, the authors note that this technique does not yet accurately determine the appropriate position for implanting the pacemaker, nor the profile that would benefit most from this technique. Furthermore, the results achieved are still not completely satisfactory, leaving something to be desired in most cases.
Possible complications of bariatric surgery
Bariatric surgery is known as a very invasive procedure, as, in most cases, a “piece” of the patient's stomach is removed in order to reduce the amount of calories absorbed by the body and lead to weight loss. Furthermore, Mariano, Monteiro and Paula36 state that it is a surgery that can present some complications, the most common of which are leaking seams, fistulas and pulmonary embolism.
Regarding pulmonary embolism, the authors point out that it is a complication that can be avoided through the administration of anticoagulants, the use of elastic stockings and mechanical compressors of the lower limbs. As for seam leaks, if they occur, they usually require surgical reintervention, which can be performed through conventional open surgery, laparoscopy or endoscopy, depending on each specific case.
Among other complications of bariatric surgery, Younes, Rizzotto and Araujo,34 point out intestinal obstruction, intra-abdominal digestive bleeding, vomiting, diarrhea, bleeding at the site of the operation, fistulas (pockets formed in the internal points of the operated site) and feces with blood, complications generally arise throughout the patient's hospital stay and, therefore, can be resolved promptly by the healthcare team. However, Younes, Rizzotto and Araujo34 explain that, depending on the severity of the symptoms and complications, there may be a need to perform a new surgical intervention to correct the problem.
It is also important to emphasize that complications from bariatric surgery can also be nutritional in nature, causing problems for the patient, such as anemia, malnutrition, calcium, folic acid and vitamin B12 deficiency. Thus, in order to carry out an intervention against obesity in a less invasive way, endoscopic gastroplasty (ESG) is used. It is interesting to note that in Brazil, the general complication rate is 0%.
Endoscopic gastroplasty
First described in 2013, endoscopic gastroplasty, according to Nava et al.,39 has been identified as an effective and safe alternative to bariatric surgery, proving over the years to be a viable and minimally invasive procedure against obesity.
According to Brunaldi et al.,40 although endoscopic gastroplasty was only popularly described in 2013, it is a procedure that was initially called the “Apollo method” that employed a full-thickness endoscopic suture device (Apollo OverStitch) to create apposition of the anterior, greater curvature and posterior wall of the gastric body. The endoscopist changes the shape of the stomach from a bean-like shape to a tubular one.
The creation of Apollo OverStitch, as explained by Brunaldi et al.,40 dates back to the 1990s, when a meeting was organized by the Olympus Corporation on Kiawah Island (USA) with the convening of several experts committed to developing new devices to treat reflux disease, large neoplastic lesions and refine transluminal suturing. The first result of animal research was published in 2005 describing the eagle claw, an endoscopic suturing device initially used for major arterial bleeding. Afterwards, new studies were carried out and, this time, with humans, starting in 2010 with the improved Apollo OverStitch, resulting in publications mainly related to the treatment of the disease weight recovery from Y-shaped gastric bypass. It was an important achievement, as, accumulated evidence that suggested that endoscopic gastric tubulation was promising for weight loss.
Gala et al.41 point out that in 2013 the Apollo OverStitch device was improved and considered second generation. However, the technique still underwent several studies to improve it as clinical use expanded throughout the world. The first described Apollo OverStitch device had several interrupted points, while the current technique uses several running points along the gastric body. For each running point, the endoscopist takes 6 to 12 bites in a square format. Some experts add reinforcing sutures between the first suture lines. Over time, suturing the gastric fundus was considered laborious and time-consuming. Furthermore, most of the serious complications of endoscopic gastroplasty were arising adjacent to the gastric fundus. Eventually, most endoscopists abandoned suturing this part of the stomach, resulting in a remaining fundal pouch. Later evidence revealed that this pouch plays an important role in the physiology of weight loss as it delays emptying. Other refinements of the early modern endoscopic gastroplasty technique include the use of the propeller and not just moving the endoscope toward the gastric wall, to grasp tissue and CO 2 insufflation per protocol.
Figure 4 proposed by Brunaldi et al.40 illustrates the current stitching method that is widely applied around the world. This method illustrates the sequence of stitches, starting with the antrum stitch, followed by the application of the second stitch, the beginning of the application of stitches with a second thread, the sequence of application of subsequent stitches on the area not yet sutured and, finally, the ESG with U-shaped suture pattern.
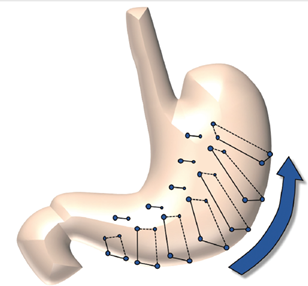
Figure 4 Schematics for the current “U” seam pattern with reinforcement stitches
Source: Brunaldi et al. (2022)
Currently, endoscopic gastroplasty has been widely promoted as a safe and effective alternative to combat obesity and, therefore, Magalhães et al.12 point to the need for constant studies on endoscopic procedures, as they are a minimally invasive alternative, of low complexity and have greater coverage in terms of the number of patients. Furthermore, endoscopic procedures are also indicated for patients who have certain physical and clinical conditions that are not eligible for bariatric or bypass surgery.
Primary endoscopic reduction gastroplasty (GREP) is known as follows in Brazil:
In Brazil, ESG is also called primary endoscopic reduction gastroplasty (GREP), gastric endosuture, endoscopic stomach reduction or endoscopic sleeve (name derived from the term ESG – endoscopic sleeve gastroplasty). Endoscopic suturing with Overstitch© can be used for any medical purpose in which it is desired to approximate tissues, endoscopically, without the need for laparoscopic or open surgery.13
Magalhães et al.12 explain that to perform the endoscopic gastroplasty procedure, the candidate must have mild obesity (grade I or II), morbid obesity or not present clinical conditions to undergo surgery, with this type of procedure having a low probability of complications, There is less dietary restriction in the postoperative period and it is still possible to reverse or redo it.
Regarding contraindications for performing endoscopic gastroplasty, according to Magalhães et al.,12 patients who have esophageal varices, active ulcers, gastric polyposis, gastric fornix, congestive gastropathy, gastric varices, psychiatric disorders, whether untreated or decompensated.
The endoscopic gastroplasty procedure can be seen in Figure 5 above , considering that image A shows the normal stomach before starting the procedure; image B is the first point of the stomach volume reduction procedure (ESG); image C refers to the application of the second point of the procedure; image D is the beginning of the application of stitches with a second thread; images E – F – G – H show the sequence of application of subsequent stitches on the area not yet sutured; images I – J – K – L are the sequence of the final appearance of the stomach after ESG with a U-shaped suture pattern, going from the gastric fundus to the antrum (proximal to distal direction).
As verified in the researched literature, the procedure known as endoscopic gastroplasty, although relatively recent, in addition to being minimally invasive, does not require cuts, as it uses a suture device that is placed in the throat so that it reaches the stomach, suturing the stomach with the aim of making it smaller.42
Endoscopic gastroplasty is an option for people who are significantly overweight and whose diet and exercise do not produce satisfactory results. With this technique, there is significant weight loss, limiting the amount that the patient can ingest. And because it is minimally invasive, the procedure reduces the risk of complications and allows a quick return to daily activities.
Like other weight loss procedures, Hedjoudje et al.42 explain that endoscopic gastroplasty requires the active participation of the patient to provide a healthier lifestyle through permanent healthy dietary changes and regular exercise to help ensure the long-term success of the procedure.
During the procedure, endoscopic gastroplasty uses the OverStitch ® endoscopic suture system with the aim of reducing the gastric lumen through tubulization, mimicking sleeve gastrectomy and gastric plication.43
Endoscopic suture system using the OverStitch®
Overstitch is a term that derives from English, with the meaning of a "seam over", a name given to the device that, after being connected to the endoscopy equipment, performs the endoscopic suture. Thus, the name Overstitch © is given as endoscopic suture. This is a device that can be adopted for any medical purpose that requires tissue approximation through endoscopy without the need for surgery. In Brazil, this device is also called endoscopic reduction gastroplasty, gastric endosuture, endoscopic stomach reduction or endoscopic sleeve.13
As Sander13 quotes:
Overstitch © aims both to reduce stomach volume (ESG), and to review and correct previously performed bariatric surgeries (secondary endoscopic reduction gastroplasty - GRES) and treatment of bariatric surgery complications: early (fistulas) and late (widening of the gastrojejunal anastomosis).13
Figure 6 shows the curved needle and 2-0 polypropolene thread with an approximate depth of 15 mm. Galvão-Neto et al.44 explain that OverStich® is an endoscopic suture system used for the purpose of making total stitches using this needle.
As explained in Figure 7, the endoscopic suture system is then connected to the endoscope handle, and at this point, the needle system is assembled at the distal tip of the device. This needle consists of thread seized by a system that has the purpose of disguising a needle holder used to carry, place and remove the thread from the suture system. It is possible to make the stitches separately or continuously after grasping the tissue with tweezers. This forceps pulls the tissue into the system and, from there, allows full stitch suturing, as can be seen in Figure 7.
To better explain Figures 6 and 7, the authors mention:
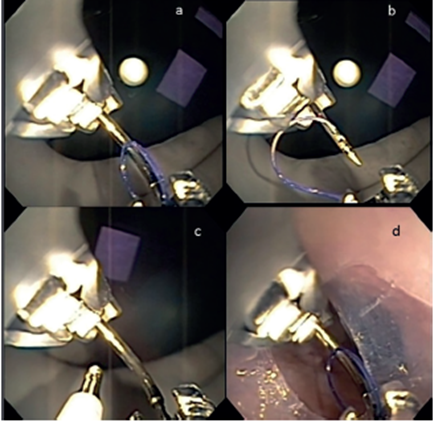
Figure 7 a) Assembly of the needle and suture thread; b) needle retraction (preparation for suture); c) tweezers; d) passage through the overtube.
Source Galvão-Neto et al. (2016).
OverStich ® is an endoscopic suturing system that, coupled to a double - channel endoscope, allows the creation of total stitches using a curved needle and 2-0 polypropolene thread, with a depth of 15 mm (Figure 6). The drive system is attached to the endoscope handle while the needle system is mounted on the distal tip of the device. The needle with the thread is captured by a system that mimics a needle holder, where it is possible to take, place and remove the thread from the suture system. The stitches can be made continuously or separated after grasping the tissue with the Helix® clamp, which aims to pull the tissue into the system, allowing full stitch suturing (Figure 7).44
According to Galvão-Neto et al.,44 at the end of each suture, a cutting and thread knot closure system is passed through the device's working channel, completing the procedure, as shown in Figure 8.
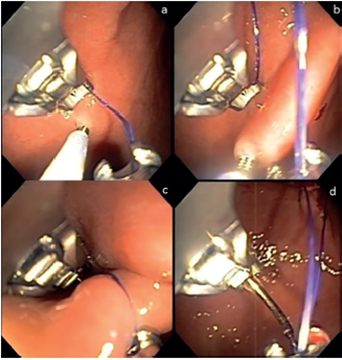
Figure 8 a) Grasping tissue with forceps; b) traction of the tissue into the device; c) crossing the point; d) preparation for the new suture.
Source: Galvão-Neto et al. (2016).
As a complement to the explanation given above by Galvão-Neto et al.,44 there is a quote from Sander, who states:
Overstitch © allows the creation of total stitches (complete transfixation of the gastric wall), using a curved needle and 2-0 polypropolene thread, with a depth of 15 mm. The drive system is coupled to the endoscope handle, while the needle system is mounted on the distal tip of the device. The needle with the thread is captured by a system that mimics a needle holder, where it is possible to take, place and remove the thread from the suture system. The stitches can be made continuously or separated after grasping the tissue with the corkscrew-shaped forceps called a helix.13
Basically, it can be seen that the overstitch method aims to reduce the food reserve capacity of the stomach through endoscopy, review and correction of previous bariatric surgeries and treatment of complications from early bariatric surgeries (fistulas) and late (widening of the anastomosis performed with weight regain).
International studies have shown that the overstitch method is safe and effective for weight reduction. Galvão-Neto et al.44 described the first vertical endoscopic gastroplasty after approval by the National Health Surveillance Agency (ANVISA) for use of the device in Brazil. According to the authors, the method was applied to a patient with a BMI of 35.17 kg/m2, with four plications performed, and the total procedure time was 50 min. The patient evolved without bleeding or other complications.
In 2017, Nava et al.45 developed a single-center prospective study on 154 patients. There were no adverse events during, after or even during follow-up. After 24 months of follow-up, they observed a significant reduction in BMI, from 38.3 to 30.8 kg/m2, with 85.7% of patients achieving the goal of excess weight loss of >25%. EWL.
Nava et al.44 state that the Overstitch © method performs endoscopic sutures, eliminating the need for more invasive surgeries, using only a curved needle to make stitches that completely cross the patient's gastric wall to a depth of 15mm.
Risk of cardiovascular diseases in patients undergoing gastroplasty endoscopic
According to Silva et al.,46 due to the loss of weight and visceral fat provided by the endoscopic suture procedure, in the short term, the results have been positive in terms of both the control and resolution of comorbidities linked to obesity. Therefore, it can be highlighted that the patient is exposed to risks with diabetes mellitus, dyslipidemia, systemic arterial hypertension (SAH), liver disease, sleep apnea and cardiovascular diseases (hypertension, congenital heart disease, acute myocardial infarction, arrhythmias cardiac, etc.).
As pointed out by Silva et al.,46 the risks of cardiovascular diseases in patients undergoing endoscopic suturing are minimal, this being a positive impact that remains with the patient in the long term, showing that there is little or no possibility of cardiovascular events and mortality. With this, it can also be highlighted that bariatric surgery should be an indicated treatment for severely obese patients who have tried different ways to lose weight, without success.
The authors explain that the possible impacts caused by endo gastric suture (ESG) in reducing body weight in relation to cardiovascular risks should be observed in the first six months to three years after surgery, as this is a period considered clinically important.
Study by Silva et al.,46 which aimed to make a comparative analysis on the frequency of cardiovascular risk factors in obese patients indicated for gastroplasty, used an observational study that allowed to verify the cardiovascular risk for this population is low for hypertension, LDL cholesterol, diabetes and syndrome metabolic. Furthermore, patients with cardiovascular risk, after the procedure, reduced their risk factors and, therefore, the positive impact provided by endoscopic suturing on weight loss is evident, since the individual, by reducing their BMI and abdominal circumference, you will have reduced cardiovascular risk.
Risk of cardiovascular diseases and its reduction based on BMI and the CC
According to Carlucci et al.,47 cardiovascular diseases are those responsible for causing disorders in the heart and blood vessels in the individual, and among the factors that present the greatest risk is obesity. Because of this, prevention and early diagnosis are essential to reduce morbidity and promote improvements in health. Obesity must be treated, as it is the main factor for cardiovascular diseases, as it has a harmful effect on health in isolation and is directly associated with the development of heart disease.
Cardiovascular diseases, in the teachings of Cunha,48 are capable of affecting four main areas, which are peripheral arterial disease, coronary heart disease, cerebrovascular disease and aortic therosclerosis with aneurysms. Conditions, such as obesity, for example, are directly associated with the onset of cardiovascular diseases, called “risk factors”.
As regards prevalence of risk factors, Cunha48 points out that this may still vary according to genetic and environmental characteristics, especially regarding lifestyle habits resulting from diet, physical activity, and others. Carrying out an anthropometric assessment as well as the identification of risk factors done individually or in combination are useful in relation to the individual's planning to seek treatment, in order to treat obesity and reduce the risks of cardiovascular diseases.
For Barroso, et al.,49 obese people have a greater accumulation of fat in the abdominal region which, in turn, as a result of their obesity situation, is directly associated with diseases such as diabetes mellitus, systemic arterial hypertension and dyslipidemia, which becomes worrying, as they are associated with the risk of developing cardiovascular diseases.
In this sense, it becomes relevant to consider the BMI and the WC of the obese individual, as they are anthropometric measurements, used to verify overweight and obesity. Both BMI and WC are simple to use measurements, in addition to being highly accurate when it comes to analyzing nutritional status.
2Mixed technique that promotes a marked reduction in the stomach and a small intestinal deviation.
As a complementary way of collecting data to analyze weight loss and risk of cardiovascular diseases in patients undergoing ESG (overstitch ®) over a 12-month period, face-to-face consultations were held. For better analysis and understanding of the data collected, categories were created, namely: epidemiological and clinical profile of patients; correlate the epidemiological profile with the effectiveness of the treatment (weight loss); analysis of weight loss over time; and analysis of the factors that impact weight loss over time and correlate those that most impact the effectiveness of the treatment in general. To this end, the statistical data presented in this chapter aims to present the results of the analysis of the research carried out using the statistical software IBM SPSS, version 27, Microsoft Excel and R-STUDIO (version 3.5.0).
Type of study
The type of research adopted to develop this study was analytical in nature, transversal in nature. To this end, patients undergoing the endo gastric procedure were selected, followed up through anthropometric assessment of the patient's month-to-month evolution and calculation of excess weight lost, percentage of excess weight lost and waist-to-hip ratio (WHR) linked to risks of cardiovascular diseases.
Population and sample
Initially, with the purpose of characterizing the sample, an analysis was carried out on 87 patients who underwent endoscopic gastroplasty and had nutritional monitoring for 12 consecutive months. During the assessments, weight, circumference, waist and hips and risk of cardiovascular disease were measured. In addition to these measures, the consultations also recorded whether the patients underwent any psychological counseling or had any difficulties with the diet and the amount of calories in the diet.
The population of this study consisted of all patients who entered the center participating in the research with the primary objective of treating obesity and with clinical indication for the procedure, from January 2021 to January 2022. These patients were invited to participate of the research, as long as they met the inclusion criteria: minimum age of 18 years, minimum BMI of 30 (grade I obesity), and patients who had already undergone bariatric surgery in the past and gained weight again (gaining at least 10% of weight minimum achieved after bariatric surgery). To characterize the sample, the epidemiological and clinical profile of the participants was surveyed for better analysis and understanding of the data collected.
Using as a model for sample calculation the results obtained by the work in Morales et. al.50– “ Modified endoscopic gastroplasty for the treatment of obesity - Surgical Endoscopy (2018) 32:3936 –3942 ” the following results were obtained. To evaluate the effectiveness of the technique, based on the percentage of excess weight lost in twelve months of follow-up, and adopting the statistical prerogatives of alpha and beta (0.05 – 0.80):
To evaluate the effectiveness of the technique, based on the percentage of excess weight lost in twelve months of follow-up, and adopting the statistical prerogatives of alpha and beta (0.05 – 0.90):
To evaluate the effectiveness of the technique, based on the percentage of waist-to-hip ratio (WHR) in twelve months of follow-up, and adopting the statistical prerogatives of alpha and beta (0.05– 0.80):
However, for each entry of 20 patients into the study, sample power and effect size tests were carried out to adjust the results in the chosen population, since the data for the sample calculation were taken from a different population.
Data collection instruments
The data collection instrument was carried out through a face-to-face consultation, in which an anthropometric assessment was carried out using the following materials: anthropometric tape/measure; balance; stadiometer and nutrition software (ditbox)
The procedure protocol was made as follows:
All patients returned for follow-up shown in Table 1.
|
Post-procedure period |
Doctor |
Nutritionist |
|
1st Semester |
Monthly |
Monthly |
|
2nd Semester |
Bimonthly |
Monthly |
|
3rd and 4th Semesters |
Quarterly |
Monthly |
Table 1 Returns for follow-up
Source: Prepared by the author (2023)
online database designed specifically for this purpose. All data was viewed only by the project coordinator and the supervisor. Backups were carried out periodically for partial data analysis, allowing data corrections as soon as possible, as well as partial reports for monitoring by researchers and the advisor.
In addition to the above, the waist-hip risk table was adopted as an auxiliary instrument for data collection, as illustrated in Figure 12:
Using this table, the percentage of excess lost and waist-to-hip ratio (WHR) was linked to the risks of cardiovascular diseases. To this end, the WHR was calculated based on the waist and hip measurements of the participating patients in order to verify their risk of developing cardiovascular disease. This verification was possible because the greater the concentration of abdominal fat, the greater the risk of problems such as high blood pressure, high cholesterol and diabetes.
Data analysis
For data analysis, all data were tested based on the normality distribution of the data. Specific tests for analysis between groups, before and after the procedure, were carried out according to the outcomes studied. A priori, all data were considered significant at p<0.05. Sample power and effect size tests were performed. The statistical package for data analysis was Stata (STATA corp. Version 13.0).
This monitoring for data analysis was carried out using the Operations Manual (MO), developed specifically for this research. Through this, an audit was carried out at the center, with no scheduled date for analyzing the procedures carried out. Every two months, a report was prepared for the supervisor to check the progress of the research, based on the MO and partial data.
The statistical data presented aims to demonstrate the results of the research analyzes carried out using the statistical software IBM SPSS, version 27, Microsoft Excel and R-STUDIO (version 3.5.0).
Ethical aspects
In compliance with CNS resolution 466/12, with a view to ensuring compliance with the guidelines and regulatory standards for research involving human beings, this research will follow four phases:
Consent form refers specifically to the procedure, corresponding to the center where it was carried out. (This is not attached to comply with the rules of this notice, where the author of the project cannot be identified in any way).
The research was carried out in a private care center for overweight and obese patients in the city of Belo Horizonte – MG. This clinic is certified to operate in all government bodies and bodies to carry out such procedures. The team involved in the project, namely the endoscopist, anesthesiologist, assistant and other collaborators are all certified by their respective professional training bodies.
The COEP approval number for the research is: 50131620.9.0000.5149
Epidemiological and clinical profile of the sample (patients)
Based on the data collected, it can be seen in Table 2 that the existing sample is 87 patients, an effect size of 0.125 and a significance level of 5%, the power of the test was approximately 99.82% (Weight), 99.8% (BMI) and 99.9% (Cardiovascular Risk). Considering this result, it can be stated that there is a very high probability of detecting a statistically significant effect, with this existing sample. High statistical power indicates that the sample is robust to detect moderate to large sized differences or effects. To calculate the sample size necessary to achieve a test power of 80%, considering an effect of 0.125 and ICC of approximately 0.88, there is a minimum sample size of 23 individuals, 3.78 times larger. For a test power of 0.90, the required sample size would be approximately 39 individuals.
|
|
|
ICC |
PW |
Sample Required |
Sample Taken |
||
|
|
(n = 87; EF = 0.125) |
PW = 80%; |
PW = 90%; |
Treatment Start (Month 0) |
End of Treatment (Month 12) |
||
|
|
ES = 0.125 |
ES = 0.125 |
|||||
|
Peso |
|
0,8879752 |
99,8 |
23 |
39 |
212 |
87 |
|
IMC |
|
0,8443617 |
99,8 |
||||
|
RCQ |
|
0,8738281 |
99,9 |
||||
Table 2 Sampling
Source: Research data (2023) Caption: ICC, Intraclass Correlation Coefficient; ES, Effect Size; PW, Test Power; n, Number of Individuals; WHR,Waist/Hip Ratio; BMI, Body Mass Index
When analyzing the results, it can be observed that the sample distribution of the 87 participating individuals, in terms of gender, is made up of 57 women (65.52%) and 30 men (34.48%). Regarding age group, the majority of participants were between 31 and 40 years old (47.13%), followed by 41 to 50 years old (21.84%), up to 30 years old (20.69%), and over 51 years old (10.34%). Regarding the BMI observed at the beginning of the study, the majority of participants had Grade 3 obesity (48.28%), followed by Grade 2 obesity (44.83%), Grade 1 obesity (5.75%) and only 1 participant was overweight (1.15%).
Table 3 provides an overview of the profile of patients who participated in this study, highlighting important information about gender, age group, initial BMI, psychological support and level of physical activity.
|
n |
% |
|
|
Sex (n = 87) |
||
|
Feminine |
57 |
65.52% |
|
Masculine |
30 |
34.48% |
|
Age Range (n = 87) |
||
|
Up to 30 years |
18 |
20.69% |
|
From 31 to 40 years old |
41 |
47.13% |
|
From 41 to 50 years old |
19 |
21.84% |
|
Over 51 years old |
9 |
10.34% |
|
Initial BMI (n = 87) |
||
|
Overweight |
1 |
1.15% |
|
Obesity Grade 1 |
5 |
5.75% |
|
Obesity Grade 2 |
39 |
44.83% |
|
Obesity Grade 3 |
42 |
48.28% |
|
Initial Psychologist Follow-up (n = 87) |
||
|
No |
23 |
26.44% |
|
Yes |
64 |
73.56% |
|
Initial Physical Activity Level (n=87) |
||
|
No activity |
22 |
25.29% |
|
Light |
65 |
74.71% |
Table 3 Patient profile
Source: Survey data (2023)
BMI, Body Mass Index
Regarding the question asked about initial psychological monitoring, a total of 73.56% of participants stated that yes, they were being monitored in the first month of the study, while 26.44% stated that they were not being monitored. Regarding the initial level of physical activity, the majority of participants reported having a light level of activity (74.71%), while 25.29% reported having no physical activity. Observe Table 3.
Table 4 presents descriptive statistics for patients at baseline. It is observed that the average weight was 114.10 kg, with an average body mass index of 39.45. Waist and hip circumferences presented averages of 105.1 cm and 121.71 cm, respectively. These numbers suggest that patients were in a state of significant obesity at the start of follow-up, as we previously noted where the majority of patients were classified as Grade 2 obesity (44.83%) and Grade 3 obesity (48.28%).
|
Variable |
Average |
Median |
Std. Dev |
Min |
Max |
|
Weight |
114.1 |
115 |
15.8 |
77 |
148 |
|
BMI |
39.45 |
39 |
3.4 |
29 |
47 |
|
Hip |
121.7 |
119 |
13.2 |
100 |
162 |
|
Waist |
105.1 |
103 |
16 |
77 |
152 |
|
Calories |
1526.9 |
1500 |
674.2 |
900 |
9000 |
|
WHR |
0.9 |
0.9 |
0.1 |
0.7 |
1 |
Table 4 Descriptive statistics of patients - Start of the study (month 1)
Source: Survey data (2023)
Caption: WHR, Waist/hip ratio; BMI, Body Mass Index
The average number of calories consumed per day was 1,526.88, indicating a dietary pattern that likely contributed to excess weight. Furthermore, the WHR, an indicator of cardiovascular risk, had an average of 0.9, highlighting a moderate risk profile for cardiovascular diseases, as shown in Table 4.
If these parameters are analyzed over a 12-month study period, the results observed will be of great importance in order to be able to evaluate the effectiveness of these interventions in reducing weight and the risks associated with obesity.
Correlation between the epidemiological profile and treatment efficacy (weight loss): an analysis over a period of 12 months
When considering the results obtained during the monitoring of these patients, it was possible to verify the results presented in Table 5, where the analysis of the patients' measurements over time is highlighted, considering the epidemiological profile.
|
Month 1 |
Month 2 |
Month 3 |
Month 4 |
Month 5 |
Month 6 |
Month 7 |
Month 8 |
Month 9 |
Month 10 |
Month 11 |
Month 12 |
P value |
|
|
Weight |
114.2 |
104.63 |
98.92 |
95,21 |
92,82 |
90,69 |
89,02 |
87,60 |
86,02 |
84,62 |
83,53 |
82,31 |
<0,001 |
|
IMC |
39,45 |
36,21 |
34,23 |
32,99 |
32,10 |
31,36 |
30,77 |
30,24 |
29,69 |
29,21 |
28,79 |
28,37 |
<0,001 |
|
RCQ |
0,90 |
0,89 |
0,88 |
0,87 |
0,87 |
0,86 |
0,86 |
0.85 |
0.85 |
0.84 |
0.84 |
0.84 |
<0.001 |
Table 5 Analysis of patient measurements over time
Source: Survey data (2023)
Caption: WHR, Waist/hip ratio; BMI, Body Mass Index
When this study began, it was observed that the average weight of the patients was 114.15 kg, with an average BMI of 39.45 and an average WHR of 0.90. However, when observing the changes over 12 months, it was noted that there was a gradual reduction in these values, which allows evidence of a progressive improvement in the patients' health. Furthermore, when comparing the average weight at the beginning (month 1) and at the end (month 12), a reduction of approximately 27.86% was noted. Another index that also showed a significant reduction was the average BMI, showing an approximate decrease of 28.11% over the 12 months studied and observed. As for the average WHR index, it also demonstrated a reduction, which allows us to affirm an improvement in the cardiovascular risk of the patients who participated in this study.
These are results that show that endoscopic gastroplasty and nutritional monitoring are effective for weight loss and cardiovascular risk in patients over the 12 months of follow-up.
Continuing, with the purpose of analyzing the relationship between BMI classifications, physical activity level and psychological monitoring at the beginning and end of the study follow-up, the Chi-square Test was adopted. The p-value obtained for each variable was compared with the 0.05 significance level to determine whether there is a statistically significant relationship between the categories at the beginning and end of the study. Using Table 6, it is possible to check the results of the comparative analysis of patients at the beginning and end of this study.
|
Start |
End |
P-Value (Chi-Square) |
|||
|
N |
% |
n |
% |
||
|
BMI classification |
|||||
|
Normal Weight |
0 |
0.00% |
14 |
16.28% |
0 |
|
Overweight |
1 |
1.15% |
45 |
52.33% |
|
|
Obesity Grade 1 |
5 |
5.75% |
20 |
23.26% |
|
|
Obesity Grade 2 |
39 |
44.83% |
6 |
6.98% |
|
|
Obesity Grade 3 |
42 |
48.28% |
1 |
1.16% |
|
|
Physical Activity Level |
|||||
|
No activity |
22 |
25.30% |
22 |
25.90% |
0 |
|
Light |
65 |
74.70% |
31 |
36.50% |
|
|
Moderate |
0 |
0.00% |
32 |
37.60% |
|
|
Psychologist |
|||||
|
No |
23 |
26.40% |
29 |
33.30% |
0.32 |
|
Yes |
64 |
73.60% |
58 |
66.70% |
|
Table 6 Comparative analysis of patients at the beginning and end of the study
Source Survey data (2023)
BMI, Body Mass Index
When analyzing the results, it was noted that in relation to the BMI classification, there was a statistically significant difference in the BMI categories at the beginning and end of the study (p <0.05). The percentage of patients with normal weight increased significantly from 0% to 16.28%, while the percentage of patients with Grade 2 and Grade 3 obesity decreased from 44.83% to 6.98% and from 48.28% to 1. 16%, respectively. This suggests a significant change in the distribution of patients' BMI throughout the study.
When analyzing the results regarding the Level of Physical Activity, a statistically significant difference was found in the levels of physical activity at the beginning and end of the study (p < 0.05). The percentage of patients with mild physical activity decreased from 74.7% to 36.5%, while the percentage of patients with moderate physical activity increased from 0% to 37.6%.
When analyzing the results of Psychological Monitoring, it was noted that there was no statistically significant difference in the frequency of psychological monitoring at the beginning and end of the study (p > 0.05). The percentage of patients who received psychological support was similar at the beginning (73.6%) and at the end (66.7%) of the study.
Analysis of weight loss over 12 months
Considering the data collected and the function of the Kruskal-Wallis Test, it was found that there was no significant difference in absolute weight loss between groups with different levels of physical activity (no activity, light and moderate), with a value of p = 0.364. However, when analyzing the percentage of weight loss, a trend towards greater weight loss was observed in groups with higher levels of physical activity, although this difference is not statistically significant, with a p value = 0.119.
Regarding BMI variation, there is also a tendency for a greater reduction in groups with higher levels of physical activity, but again, this difference is not statistically significant, with a value of p = 0.065. On the other hand, the variation in WHR shows a statistically significant difference between the groups, with a value of p = 0.035. This suggests that the level of physical activity may influence the reduction in WHR, with higher levels of physical activity associated with a greater reduction in this index of cardiovascular risk. Such results can be seen in Table 7.
|
Physical Activity Level |
||||
|
No Activity |
Light |
Moderate |
Kruskal Wallis Test |
|
|
Ultimate Weight Loss |
-17.27 |
-36.13 |
-38.44 |
0.364 |
|
% Final Weight Loss |
-15.21 |
-31.4 |
-33.54 |
0.119 |
|
% BMI Loss |
-15.07 |
-31.43 |
-33.97 |
0.065 |
|
% WHR Loss |
-3.04 |
-7.02 |
-9.92 |
0.035 |
Table 7 Analysis of average weight loss according to the level of physical activity at the end of the study
Source: Survey data (2023)
Caption: WHR, Waist/hip ratio; BMI, Body Mass Index
Next, as can be seen in Table 8, the influence of sex and physical activity on weight loss was analyzed, segmented by women and men, using the Kruskal-Wallis test to compare the means between the groups with different levels of physical activity.
|
|
|
Physical Activity Level |
Kruskal Wallis Test |
||
|
No Activity |
Light |
Moderate |
|||
|
Women |
Ultimate Weight Loss |
-13.36 |
-34.46 |
-37.86 |
0.169 |
|
|
% Final Weight Loss |
-13.27 |
-31.51 |
-34.94 |
0.019 |
|
|
% BMI Loss |
-12.96 |
-31.49 |
-35.34 |
0.013 |
|
|
% WHR Loss |
-3.00 |
-7.13 |
-10.75 |
0.018 |
|
Men |
Ultimate Weight Loss |
-21.18 |
-41.86 |
-39.70 |
0.434 |
|
|
% Final Weight Loss |
-17.15 |
-31.05 |
-30.45 |
0.626 |
|
|
% BMI Loss |
-17.17 |
-31.25 |
-30.94 |
0.733 |
|
|
% WHR Loss |
-3.08 |
-6.62 |
-8.11 |
0.696 |
Table 8 Analysis of the Influence of Sex and Physical Activity on Weight Loss in 12 months
Source: Survey data (2023)
Caption: WHR, Waist/hip ratio; BMI, Body Mass Index
As for females, no statistically significant difference was found in absolute weight loss between different levels of physical activity, with a value of p = 0.169. However, when analyzing the percentage of final weight loss, a statistically significant difference was observed, with a value of p = 0.019, indicating that women who practiced moderate physical activity had a greater percentage of weight loss compared to those who practiced moderate physical activity. Do not practice or have practiced light physical activity. Women who practiced moderate physical activity had a 34.94% reduction in weight compared to their initial weight. Regarding the variation in BMI and WHR, statistically significant differences were also found between groups with different levels of physical activity, with values of p = 0.013 and p = 0.018, respectively.
As for men, no statistically significant differences were found in absolute weight loss, percentage of weight loss, BMI variation or WHR variation between different levels of physical activity. Observe Table 8.
Regarding the analysis of the influence of age and physical activity on weight loss, this was segmented by age groups. For participants aged 31 to 40, no statistically significant differences were found in weight loss, BMI variation or WHR variation between different levels of physical activity. However, a statistically significant difference was found in the percentage of weight loss, with a p-value = 0.045, indicating that participants in this age group who practiced moderate physical activity had a greater percentage of weight loss compared to those who did not or practiced light physical activity.
For participants up to 30 years old and 41 to 50 years old, no statistically significant differences were found in weight loss, percentage of weight loss, BMI variation or WHR variation between different levels of physical activity, as shown in Table 9.
|
|
|
Physical Activity Level |
Kruskal Wallis Test |
||
|
No Activity |
Light |
Moderate |
|||
|
Up to 30 years |
Ultimate Weight Loss |
-17.00 |
-36.75 |
-37.50 |
0.903 |
|
|
% Final Weight Loss |
-15.04 |
-32.90 |
-32.79 |
0.808 |
|
|
% BMI Loss |
-14.65 |
-32.47 |
-32.96 |
1,000 |
|
|
% RCQ Loss |
-3.28 |
-5.66 |
-8.37 |
0.225 |
|
From 31 to 40 years |
Final Weight Loss |
-15.25 |
-35.73 |
-38.08 |
0.509 |
|
|
% Final Weight Loss |
-14.32 |
-31.71 |
-35.57 |
0.045 |
|
|
% BMI Loss |
-14.12 |
-31.83 |
-36.29 |
0.028 |
|
|
% WHR Loss |
-3.29 |
-6.09 |
-12.18 |
0.007 |
|
From 41 to 50 years old |
Ultimate Weight Loss |
-19.00 |
-38.25 |
-40.38 |
0.599 |
|
|
% Final Weight Loss |
-16.68 |
-30.88 |
-31.61 |
0.916 |
|
|
% BMI Loss |
-16.81 |
-31.18 |
-32.00 |
1,000 |
|
|
% WHR Loss |
-3.32 |
-8.62 |
-8.88 |
0.834 |
|
Over 51 years old |
Ultimate Weight Loss |
-21.20 |
-32.75 |
|
|
|
|
% Final Weight Loss |
-16.52 |
-29.82 |
|
|
|
|
% BMI Loss |
-16.46 |
-29.41 |
|
|
|
|
% WHR Loss |
-2.17 |
-8.62 |
|
|
Table 9 Analysis of the Influence of Age and Physical Activity on Weight Loss, over 12 months
Source: Survey data (2023)
Caption: WHR, Waist/hip ratio; BMI, Body Mass Index
Analysis of the factors that impact weight loss over time and that most impact the effectiveness of treatment in general: influence of time on weight variation
Regarding weight analysis over the months, the standard deviation remained relatively stable at around 11-15, showing consistency in the dispersion of data in relation to the average, as can be seen in Figure 13.
Based on the results obtained with the analysis between the different times of weight measurement, it was possible to conclude that there was a statistically significant evolution in the patients' weight over the 12 months of follow-up, which suggests that, on average, the patients' weight varied significantly during the observation period. It was also concluded that comparisons between all pairs of measurement times show statistically significant differences in weight. This indicates that the pattern of change in weight is not linear and varies over time. Furthermore, the significant differences between measurement times suggest that certain periods may be associated with more significant changes in weight than others. Such data can be better viewed in Table 10.
|
Time |
Beta |
I.C. - 95% |
Valor-p |
|
1 / 2 |
9,52 |
[9,01; 10,03] |
0,000 |
|
1 / 3 |
15,23 |
[14,28; 16,18] |
0,000 |
|
1 / 4 |
18,94 |
[17,63; 20,26] |
0,000 |
|
1 / 5 |
21,33 |
[19,78; 22,89] |
0,000 |
|
1 / 6 |
23,46 |
[21,8; 25,12] |
0,000 |
|
1 / 7 |
25,13 |
[23,32; 26,94] |
0,000 |
|
1 / 8 |
26,55 |
[24,62; 28,48] |
0,000 |
|
1 / 9 |
28,13 |
[26,04; 30,21] |
0,000 |
|
1 / 10 |
29,53 |
[27,32; 31,74] |
0,000 |
|
1 / 11 |
30,62 |
[28,28; 32,96] |
0,000 |
|
1 / 12 |
34,93 |
[31,36; 38,51] |
0,000 |
|
2 / 3 |
5,71 |
[5,21; 6,21] |
0,000 |
|
2 / 4 |
9,43 |
[8,51; 10,34] |
0,000 |
|
2 / 5 |
11,82 |
[10,62; 13,02] |
0,000 |
|
2 / 6 |
13,94 |
[12,6; 15,28] |
0,000 |
|
2 / 7 |
15,61 |
[14,09; 17,13] |
0,000 |
|
2 / 8 |
17,03 |
[15,36; 18,71] |
0,000 |
|
2 / 9 |
18,61 |
[16,76; 20,46] |
0,000 |
|
2 / 10 |
20,01 |
[18,02; 22,01] |
0,000 |
|
2 / 11 |
21,1 |
[18,96; 23,25] |
0,000 |
|
2 / 12 |
25,41 |
[22,13; 28,7] |
0,000 |
|
3 / 4 |
3,71 |
[3,18; 4,25] |
0,000 |
|
3 / 5 |
6,1 |
[5,24; 6,97] |
0,000 |
|
3 / 6 |
8,23 |
[7,19; 9,27] |
0,000 |
|
3 / 7 |
9,9 |
[8,64; 11,15] |
0,000 |
|
3 / 8 |
11,32 |
[9,88; 12,76] |
0,000 |
|
3 / 9 |
12,9 |
[11,27; 14,53] |
0,000 |
|
3 / 10 |
14,3 |
[12,51; 16,08] |
0,000 |
|
3 / 11 |
15,39 |
[13,44; 17,35] |
0,000 |
|
3 / 12 |
19,7 |
[16,63; 22,77] |
0,000 |
|
4 / 5 |
2,39 |
[1,95; 2,83] |
0,000 |
|
4 / 6 |
4,52 |
[3,88; 5,15] |
0,000 |
|
4 / 7 |
6,18 |
[5,28; 7,09] |
0,000 |
|
4 / 8 |
7,61 |
[6,49; 8,73] |
0,000 |
|
4 / 9 |
9,18 |
[7,87; 10,5] |
0,000 |
|
4 / 10 |
10,59 |
[9,11; 12,06] |
0,000 |
|
4 / 11 |
11,68 |
[10,01; 13,35] |
0,000 |
|
4 / 12 |
15,99 |
[13,08; 18,9] |
0,000 |
|
5 / 6 |
2,13 |
[1,8; 2,45] |
0,000 |
|
5 / 7 |
3,79 |
[3,2; 4,39] |
0,000 |
|
5 / 8 |
5,22 |
[4,4; 6,03] |
0,000 |
|
5 / 9 |
6,79 |
[5,79; 7,8] |
0,000 |
|
5 / 10 |
8,2 |
[7,02; 9,37] |
0,000 |
|
5 / 11 |
9,29 |
[7,91; 10,66] |
0,000 |
|
5 / 12 |
13,6 |
[10,76; 16,44] |
0,000 |
|
6 / 7 |
1,67 |
[1,3; 2,04] |
0,000 |
|
6 / 8 |
3,09 |
[2,48; 3,71] |
0,000 |
|
6 / 9 |
4,67 |
[3,87; 5,47] |
0,000 |
|
6 / 10 |
6,07 |
[5,1; 7,04] |
0,000 |
|
6 / 11 |
7,16 |
[5,99; 8,33] |
0,000 |
|
6 / 12 |
11,47 |
[8,65; 14,3] |
0,000 |
|
7 / 8 |
1,43 |
[1,05; 1,8] |
0,000 |
|
7 / 9 |
3 |
[2,45; 3,55] |
0,000 |
|
7 / 10 |
4,4 |
[3,67; 5,13] |
0,000 |
|
7 / 11 |
5,49 |
[4,57; 6,42] |
0,000 |
|
7 / 12 |
9,8 |
[7,01; 12,6] |
0,000 |
|
8 / 9 |
1,57 |
[1,25; 1,9] |
0,000 |
|
8 / 10 |
2,98 |
[2,47; 3,48] |
0,000 |
|
8 / 11 |
4,07 |
[3,38; 4,76] |
0,000 |
|
8 / 12 |
8.38 |
[5.57; 11.19] |
0.000 |
|
9 / 10 |
1.4 |
[1.09; 1.71] |
0.000 |
|
9/11 |
2.49 |
[ 2 ; 2.99] |
0.000 |
|
9/12 |
6.8 |
[3.94; 9.67] |
0.000 |
|
10 / 11 |
1.09 |
[0.77; 1.41] |
0.000 |
|
10 / 12 |
5.4 |
[2.5; 8.31] |
0.000 |
|
11 / 12 |
4.31 |
[1.36; 7.26] |
0.004 |
Table 10 Influence of time on weight
Source: Survey data (2023)
Regarding the influence of time on BMI, based on descriptive statistics of BMI over the months, the average values were higher in the first months, with an average of 39.4 for m1 and 36.2 for m2, while the final months presented lower average values, with an average of 29.2 for m10, 28.8 for m11 and 28.4 for m12. The median BMI followed a similar trend, with higher values in the first months and lower in the last.
As for the standard deviation, variability in values was observed over the months, indicating the dispersion of data around the average. These analyzes suggest possible changes in the nutritional status of individuals over time, with potential influences of factors such as diet, physical activity and other variables that can affect BMI, as seen in Figure 14.
Analysis of the BMI results shows that as the months progress, the differences between consecutive months appear to increase, indicating a reduction in BMI over time. Furthermore, it also proves that some comparisons show greater differences than others. For example, comparisons between consecutive months tend to have smaller differences compared to those between more distant months. These observations suggest that patients' BMI tends to reduce over time, with significant differences between months, especially between the first and last months of the study period, as shown in Table 11.
|
Time |
Beta |
IC - 95% |
p-value |
|
1 / 2 |
3.24 |
[3.08; 3,4] |
0.000 |
|
1 / 3 |
5.22 |
[4.95; 5.49] |
0.000 |
|
1 / 4 |
6.46 |
[6.09; 6.83] |
0.000 |
|
1 / 5 |
7.34 |
[6.88; 7.81] |
0.000 |
|
1 / 6 |
8.09 |
[7.61; 8.58] |
0.000 |
|
1 / 7 |
8.68 |
[8,11; 9.25] |
0.000 |
|
1 / 8 |
9,21 |
[8,58; 9,84] |
0,000 |
|
1 / 9 |
9,76 |
[9,07; 10,44] |
0,000 |
|
1 / 10 |
10,24 |
[9,5; 10,98] |
0,000 |
|
1 / 11 |
10,66 |
[9,87; 11,44] |
0,000 |
|
1 / 12 |
11,81 |
[10,71; 12,92] |
0,000 |
|
2 / 3 |
1,98 |
[1,8; 2,16] |
0,000 |
|
2 / 4 |
3,22 |
[2,93; 3,51] |
0,000 |
|
2 / 5 |
4,1 |
[3,72; 4,49] |
0,000 |
|
2 / 6 |
4,85 |
[4,43; 5,27] |
0,000 |
|
2 / 7 |
5,44 |
[4,92; 5,96] |
0,000 |
|
2 / 8 |
5,97 |
[5,38; 6,55] |
0,000 |
|
2 / 9 |
6,52 |
[5,88; 7,16] |
0,000 |
|
2 / 10 |
7 |
[6,29; 7,71] |
0,000 |
|
2 / 11 |
7,41 |
[6,66; 8,17] |
0,000 |
|
2 / 12 |
8,57 |
[7,52; 9,62] |
0,000 |
|
3 / 4 |
1,24 |
[1,04; 1,44] |
0,000 |
|
3 / 5 |
2,13 |
[1,84; 2,41] |
0,000 |
|
3 / 6 |
2,87 |
[2,54; 3,2] |
0,000 |
|
3 / 7 |
3,46 |
[3,03; 3,89] |
0,000 |
|
3 / 8 |
3,99 |
[3,49; 4,49] |
0,000 |
|
3 / 9 |
4,54 |
[3,97; 5,11] |
0,000 |
|
3 / 10 |
5,02 |
[4,39; 5,65] |
0,000 |
|
3 / 11 |
5,44 |
[4,76; 6,12] |
0,000 |
|
3 / 12 |
6,59 |
[5,59; 7,6] |
0,000 |
|
4 / 5 |
0,89 |
[0,71; 1,06] |
0,000 |
|
4 / 6 |
1,63 |
[1,4; 1,86] |
0,000 |
|
4 / 7 |
2,22 |
[1,88; 2,56] |
0,000 |
|
4 / 8 |
2,75 |
[2,34; 3,16] |
0,000 |
|
4 / 9 |
3,3 |
[2,82; 3,78] |
0,000 |
|
4 / 10 |
3,78 |
[3,24; 4,33] |
0,000 |
|
4 / 11 |
4,2 |
[3,59; 4,8] |
0,000 |
|
4 / 12 |
5,35 |
[4,37; 6,34] |
0,000 |
|
5 / 6 |
0,75 |
[0,61; 0,88] |
0,000 |
|
5 / 7 |
1,33 |
[1,1; 1,56] |
0,000 |
|
5 / 8 |
1,86 |
[1,55; 2,17] |
0,000 |
|
5 / 9 |
2,41 |
[2,04; 2,79] |
0,000 |
|
5 / 10 |
2,9 |
[2,45; 3,34] |
0,000 |
|
5 / 11 |
3,31 |
[2,8; 3,82] |
0,000 |
|
5 / 12 |
4,47 |
[3,5; 5,43] |
0,000 |
|
6 / 7 |
0,59 |
[0,42; 0,75] |
0,000 |
|
6 / 8 |
1,11 |
[0,87; 1,36] |
0,000 |
|
6 / 9 |
1,67 |
[1,36; 1,98] |
0,000 |
|
6 / 10 |
2,15 |
[1,77; 2,53] |
0,000 |
|
6 / 11 |
2,56 |
[2,13; 3] |
0,000 |
|
6 / 12 |
3,72 |
[2,76; 4,68] |
0,000 |
|
7 / 8 |
0,53 |
[0,37; 0,68] |
0,000 |
|
7 / 9 |
1,08 |
[0,87; 1,29] |
0,000 |
|
7 / 10 |
1,56 |
[1,28; 1,84] |
0,000 |
|
7 / 11 |
1,98 |
[1,64; 2,31] |
0,000 |
|
7 / 12 |
3,13 |
[2,19; 4,08] |
0,000 |
|
8 / 9 |
0,55 |
[0,41; 0,69] |
0,000 |
|
8 / 10 |
1,03 |
[0,83; 1,24] |
0,000 |
|
8 / 11 |
1,45 |
[1,2; 1,69] |
0,000 |
|
8 / 12 |
2,61 |
[1,66; 3,55] |
0,000 |
|
9 / 10 |
0,48 |
[0,34; 0,62] |
0,000 |
|
9 / 11 |
0,9 |
[0,72; 1,07] |
0,000 |
|
9 / 12 |
2,05 |
[1,08; 3,02] |
0,000 |
|
10 / 11 |
0,41 |
[0,28; 0,54] |
0,000 |
|
10 / 12 |
1,57 |
[0,59; 2,55] |
0,002 |
|
11 / 12 |
1,16 |
[0,16; 2,15] |
0.022 |
Table 11 Influence of time on BMI
Source: Survey data (2023)
BMI, Body Mass Index
Regarding the influence of time on the WHR, the analysis carried out using descriptive statistics reveals that over the months, the mean and median remained constant at approximately 0.9, indicating stability or little variation in this patient measurement. The minimum value fluctuated between 0.7 and 0.8, while the maximum value varied from 1.0 to 0.7 over the months, as shown in Figure 15. This suggests that, in general, participants maintained a waist-to-hip ratio with low variation.
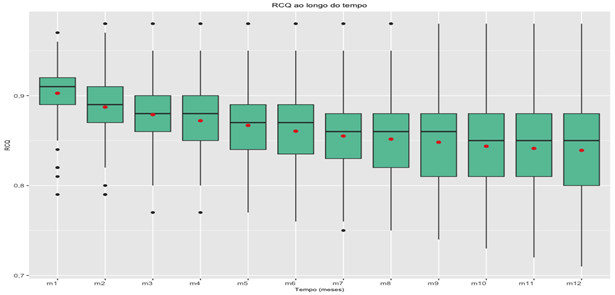
Figure 15 Box-Plot of BMI over the months.
Source: Survey data (2023).
Caption: BMI, Body Mass Index
The analysis of the RCQ results shows that, based on the analysis of RCQ residues over the months, it is not possible to state that time is a factor that directly impacts the reduction in RCQ. The RCQ residuals, originated by the statistical model (Table 12) are indicators of the difference between the observed values and the values predicted by the statistical model. An increase in WHR residuals may suggest a variation in the quality of measurements or discrepancies between actual values and values predicted by the model.
|
Time |
Beta |
IC - 95% |
p-value |
|
1 / 2 |
0.02 |
[0.01; 0.02] |
0.000 |
|
1 / 3 |
|
[0,02; 0,03] |
0,000 |
|
1 / 4 |
0,03 |
[0,02; 0,04] |
0,000 |
|
1 / 5 |
0,04 |
[0,03; 0,04] |
0,000 |
|
1 / 6 |
|
[0,03; 0,05] |
0,000 |
|
1 / 7 |
0,05 |
[0,04; 0,06] |
0,000 |
|
1 / 8 |
|
[0,04; 0,06] |
0,000 |
|
1 / 9 |
|
[0,05; 0,06] |
0,000 |
|
1 / 10 |
0,06 |
[0,05; 0,07] |
0,000 |
|
1 / 11 |
|
[0,05; 0,07] |
0,000 |
|
1 / 12 |
0,07 |
[0,06; 0,09] |
0,000 |
|
2 / 3 |
0,01 |
[0,01; 0,01] |
0,000 |
|
2 / 4 |
0,02 |
[0,01; 0,02] |
0,000 |
|
2 / 5 |
|
[0,02; 0,03] |
0,000 |
|
2 / 6 |
0,03 |
[0,02; 0,03] |
0,000 |
|
2 / 7 |
|
[0,03; 0,04] |
0,000 |
|
2 / 8 |
0,04 |
[0,03; 0,04] |
0,000 |
|
2 / 9 |
|
[0,03; 0,05] |
0,000 |
|
2 / 10 |
|
[0,04; 0,05] |
0,000 |
|
2 / 11 |
0,05 |
[0,04; 0,05] |
0,000 |
|
2 / 12 |
0,06 |
[0,05; 0,07] |
0,000 |
|
3 / 4 |
0,01 |
[0; 0,01] |
0,000 |
|
3 / 5 |
|
[0,01; 0,02] |
0,000 |
|
3 / 6 |
0,02 |
[0,01; 0,02] |
0,000 |
|
3 / 7 |
|
[0,02; 0,03] |
0,000 |
|
3 / 8 |
0,03 |
[0,02; 0,03] |
0,000 |
|
3 / 9 |
|
[0,02; 0,04] |
0,000 |
|
3 / 10 |
0,04 |
[0,03; 0,04] |
0,000 |
|
3 / 11 |
|
[0,03; 0,04] |
0,000 |
|
3 / 12 |
0,05 |
[0,04; 0,06] |
0,000 |
|
4 / 5 |
0,01 |
[0; 0,01] |
0,000 |
|
4 / 6 |
|
[0,01; 0,01] |
0,000 |
|
4 / 7 |
0,02 |
[0,01; 0,02] |
0,000 |
|
4 / 8 |
|
[0,02; 0,02] |
0,000 |
|
4 / 9 |
|
[0,02; 0,03] |
0,000 |
|
4 / 10 |
0,03 |
[0,02; 0,03] |
0,000 |
|
4 / 11 |
|
[0,02; 0,04] |
0,000 |
|
4 / 12 |
0,04 |
[0,03; 0,05] |
0,000 |
|
5 / 6 |
0,01 |
[0; 0,01] |
0,000 |
|
5 / 7 |
|
[0,01; 0,01] |
0,000 |
|
5 / 8 |
0,02 |
[0,01; 0,02] |
0,000 |
|
5 / 9 |
|
[0,01; 0,02] |
0,000 |
|
5 / 10 |
|
[0,02; 0,03] |
0,000 |
|
5 / 11 |
0,03 |
[0,02; 0,03] |
0,000 |
|
5 / 12 |
0,04 |
[0,03; 0,05] |
0,000 |
|
6 / 7 |
0,01 |
[0; 0,01] |
0,000 |
|
6 / 8 |
|
[0,01; 0,01] |
0,000 |
|
6 / 9 |
|
[0,01; 0,02] |
0,000 |
|
6 / 10 |
0,02 |
[0,01; 0,02] |
0,000 |
|
6 / 11 |
|
[0,01; 0,02] |
0,000 |
|
6 / 12 |
0,03 |
[0,02; 0,04] |
0,000 |
|
7 / 8 |
0 |
[0; 0] |
0,000 |
|
7 / 9 |
0,01 |
[0; 0,01] |
0,000 |
|
7 / 10 |
|
[0,01; 0,01] |
0,000 |
|
7 / 11 |
|
[0,01; 0,02] |
0,000 |
|
7 / 12 |
0,03 |
[0,01; 0,04] |
0,000 |
|
8 / 9 |
0 |
[0; 0] |
0,000 |
|
8 / 10 |
0,01 |
[0,01; 0,01] |
0,000 |
|
8 / 11 |
|
[0,01; 0,01] |
0,000 |
|
8 / 12 |
0,02 |
[0,01; 0,03] |
0,000 |
|
9 / 10 |
0 |
[0; 0,01] |
0,000 |
|
9 / 11 |
0,01 |
[0; 0,01] |
0,000 |
|
9 / 12 |
0,02 |
[0,01; 0,03] |
0,001 |
|
10 / 11 |
0 |
[0; 0] |
0,036 |
|
10 / 12 |
0,01 |
[0; 0,03] |
0,014 |
|
11 / 12 |
|
[ 0 ; 0.02] |
0.046 |
Table 12 Influence of time on the Waist-Hip Risk Table
Source: Survey data (2023)
Multivariate model
With the aim of analyzing which factors most influence the effectiveness of the treatment, considering the weight reduction criteria, BMI and WHR, three regression models were proposed for each of the variables, which are the Weight Loss Model, BMI Model and WHR Model.
Weight loss model
The Weight Loss Model is the first multivariate model constructed, taking into account which variables contribute to a reduction in patient weight. The results indicate that the patient's gender and psychological support are factors that significantly impact patients' weight loss. The coefficient for male is 5.44349 and p-value is 0.00575, which indicates that gender is statistically significant in explaining patients' final weight loss. Male patients tend to have a greater final weight loss compared to female patients.
The coefficient for months of Psychology (PSI) is 1.65403 (p-value < 0.001), which indicates that the number of months with psychological support are highly significant in explaining the patients' final weight loss. For every one month increase in psychologist, an increase of approximately 1.65 units in final weight loss is expected.
Although the practice of moderate physical activity has a positive beta, indicating a relationship with weight loss, we cannot say that it has a direct relationship with weight measurement in absolute value. The intercept is the expected value of the response variable when all explanatory variables are zero. This means that when all other variables are zero, the final weight loss is expected to be approximately 13.81 kilograms in patients.
The coefficient of determination (R-squared) is 0.5975, which means that approximately 59.75% of the variability in patients' final weight loss is explained by the variables included in the model. Such results can be better visualized in Table 13.
|
Final weight loss |
||||
|
Predictors |
Estimates |
std. Error |
CI |
p |
|
(Intercept) |
13.81 |
4.48 |
4.90 – 22.72 |
0.003 |
|
AGE |
0.03 |
0.11 |
-0.19 – 0.26 |
0.756 |
|
Sex [M] |
5.44 |
1.92 |
1.63 – 9.26 |
0.006 |
|
PSI Months |
1.65 |
0.19 |
1.28 – 2.03 |
<0.001 |
|
Moderate ATV months |
0.27 |
0.21 |
-0.14 – 0.68 |
0.192 |
|
Observations |
87 |
|||
|
R2 / R2 adjusted |
0.598 / 0.578 |
|||
Table 13 Final weight loss
BMI Model
The BMI Model is the multivariate model that considers the response variable as the percentage of variation/reduction in BMI from the beginning to the end of treatment. Based on the data collected, it can be concluded that the significant variables to explain the percentage of variation/reduction in BMI are the months of psychological monitoring and the months of moderate activity. Age and sex did not show statistical significance.
The coefficient for months of moderate exercise activity is 0.32570 (p-value 0.0377), which indicates that months of moderate exercise activity are statistically significant in explaining the percentage of BMI loss. For every one month increase in moderate activity, an increase of approximately 0.33% in the percentage of BMI loss is expected.
As for the number of months with psychological support, it is 1.27876, which indicates that the months of PSI are highly significant in explaining the percentage of BMI loss. For every one-month increase in PSI, an increase of approximately 1.28% in the percentage of BMI loss is expected.
The significant intercept indicates that, when all other variables are zero, the percentage of BMI loss is expected to be approximately 15.56% throughout the patients' follow-up. The R-squared coefficient is 0.6555, which means that approximately 65.55% of the variability in the percentage of BMI loss is explained by the variables included in the model. Observe the results in Table 14.
|
Percentual_BMI_final |
||||
|
Predictors |
Estimates |
std. Error |
CI |
p |
|
(Intercept) |
15.56 |
3.34 |
8.92 – 22.20 |
<0.001 |
|
Age |
0.01 |
0.08 |
-0.15 – 0.18 |
0.874 |
|
Sex [m] |
-0.38 |
1.43 |
-3.22 – 2.47 |
0.792 |
|
PSI months |
1.28 |
0.14 |
1.00 – 1.56 |
<0.001 |
|
Moderate ATV months |
0.33 |
0.15 |
0.02 – 0.63 |
0.038 |
|
Observations |
87 |
|||
|
R2 / R2 adjusted |
0.655 / 0.639 |
|||
Table 14 Final BMI percentage
Source: Survey data (2023)
WHR Model
The WHR Model is the multivariate model that considers the response variable as the percentage of patients' WHR loss after 12 months of treatment. Moderate exercise activity is the habit that has the most influence on reducing patients' WHR. The coefficient for months of moderate activity is - 0.46089 (p-value 0.000722), which indicates that months of moderate activity are highly significant in explaining the percentage of WHR loss. For every one month increase in moderate activity, an approximately 0.46% decrease in the percentage of WHR loss is expected.
The intercept is -1.21658. This shows that the average WHR loss percentage is approximately -1.22%. Table 15 shows the results.
|
Percentual_RCQ |
||||
|
Predictors |
Estimates |
std. Error |
CI |
p |
|
(Intercept) |
-1.22 |
2.84 |
-6.87 – 4.44 |
0.670 |
|
Age |
-0.09 |
0.07 |
-0.23 – 0.05 |
0.211 |
|
Sex [m] |
1.76 |
1.22 |
-0.66 – 4.19 |
0.151 |
|
PSI months |
-0.14 |
0.12 |
-0.38 – 0.10 |
0.241 |
|
Moderate ATV months |
-0.46 |
0.13 |
-0.72 – -0.20 |
0.001 |
|
Observations |
87 |
|||
|
R2 / R2 adjusted |
0.250 / 0.214 |
|||
Table 15 WHR Percentage
Source: Survey data (2023)
Considering the results achieved, the efficiency of the weight loss procedure is notable, allowing us to see that the patient undergoing this ESG procedure will have a reduced likelihood of cardiovascular diseases, as one of the factors that most cause these diseases is obesity. And, as it is a minimally invasive procedure that has shown effectiveness in treating obesity.
This work was developed to investigate weight loss in patients undergoing ESG, which allowed us to initially verify that obesity is a public health problem that affects people of all ages and genders around the world. Considering that obesity is a serious public health problem, it is possible to observe the importance of seeking methods that are less invasive, more effective and that have few complications, especially cardiovascular ones.
Considering the objective proposed in this research, it can be stated that the sample analyzed, taking into account the characteristics, reflects the general situation of the participating patients, who sought help to lose weight. To this end, a cross-sectional study was carried out, which was necessary to analyze weight loss and risk of cardiovascular diseases in patients undergoing ESG because it allowed the cause associated with the effect of the analyzed phenomenon to be exposed. According to Hochman et al.,51 cross-sectional research helps the researcher to collect data from the meanings of real life, in order to identify and obtain evidence about the objectives that are intended to be achieved.
The objective is to determine the necessary sample size and test power for a study with repeated measures over 12 months, considering the Intraclass Correlation Coefficients for the variables of WEIGHT, BMI and WHR, an effect size and a level of 5% significance.
When analyzing, initially, the sample profile was characterized by the majority of women (65.52%), aged between 31 and 40 years (47.13%) and BMI at the beginning of the study in Grade 3 (48. 28%), the majority (73.56%) stated that they had psychological support and reported having a light level of physical activity (74.71%). In the context of obesity, it is important to point out that, according to Ferreira et al.,2 it is a public health problem, as obese individuals are at high risk of developing various diseases related to the problem of fat accumulation, such as diabetes, GOUT, high blood pressure, cholecystitis, joint problems, among others. It can be said that among the main factors causing obesity is the imbalance between food intake and energy expenditure, which results in high caloric consumption and little physical activity. Currently, obesity has been a concern, as people increasingly tend to reduce energy expenditure due to having a sedentary lifestyle.
What drew attention in this study was the dietary pattern of the sample, which may have been one of the main and most aggravating factors for excess weight and WHR with an average of 0.9. These data suggest that patients, at the beginning of this study, had an obesity profile with cardiovascular risk, highlighting the importance of intervention and nutritional monitoring to improve their health and quality of life. Regarding the RCQ, Tinoco et al.52 explain that it refers to a calculation carried out based on the individual's waist and hip measurements with the purpose of checking the possibility, that is, the risk of developing a cardiovascular disease. This fact is permitted because the greater the concentration of abdominal fat in the person, consequently, the higher the risk of developing problems, such as, for example, high blood pressure, high cholesterol, diabetes, among others.
The analysis over time, over a period of 12 months, through the analysis of the measurements of patients monitored after undergoing the endoscopic gastroplasty procedure and nutritional monitoring, revealed a significant reduction in weight, BMI and WHR. At this point, it is necessary to return to the literature and explain that BMI and WHR are indicators used as more precise indirect measures of obesity, shown to present good performance in terms of health risk predictors.53
The results collected above suggest that endoscopic gastroplasty and nutritional monitoring were effective in reducing the weight and cardiovascular risk of patients over the 12 months of follow-up. Hedjoudje et al.42 explain that this weight loss procedure consists of reducing the stomach using an endoscopic suture, characterized as minimally invasive, without the need for hospitalization of the patient and is quick to perform. Endoscopic gastroplasty helps to treat and control mild/moderate obesity, being an alternative for those who wish to lose weight and have not yet undergone surgical treatment or Bypass, which in turn allows the problem to be resolved early.
The relationship between BMI classifications, physical activity level and psychological monitoring at the beginning and end of the study follow-up was adopted using the Chi-square test. This test, according to Contador and Senne,54 is adopted with the objective of evaluating fit, homogeneity and independence, considered a quality test that determines a distribution of observed frequencies. From this, it was found that the BMI classification showed a statistically significant difference at the beginning and end of the study (p <0.05). The percentage of patients with Grade 2 and Grade 3 obesity decreased from 44.83% to 6.98% and from 48.28% to 1.16%.
Regarding the level of physical activity, the difference at the beginning and end of the study (p < 0.05) decreased from 74.7% to 36.5%, and the percentage of patients with moderate physical activity increased from 0% to 37.6%.
Psychological support did not show a significant difference at the beginning and end of the study (p > 0.05), with patients who received psychological support being similar at the beginning (73.6%) and at the end (66.7%). However, the literature states that, according to Fagundes, Caregnato and Silveira,55 it is in the post-operative period that the individual needs to receive greater attention in all aspects, both physical and emotional, as, after surgery, they become more weakened because it is a renewal in his life, a new phase where he will begin to eat differently, making him vulnerable to social and psychological changes, which require adaptations. Based on the above, Almeida and Nespoli56 emphasize that the beginning of the postoperative period generally impacts the person who, if they do not receive due support from their family and psychological support, may not be able to deal easily with their new phase of life and, Therefore, the work and support of a Psychologist in this initial process is essential so that they can know how to deal with the changes that will occur in their lives and, thus, reduce the possibilities of being negatively affected psychologically in the long term. However, according to the results obtained in the field, it cannot be said that psychological support showed a significant difference at the beginning and end of the study.
In addition to the above, the study also showed that, based on the results, it is clear that the patient's gender and psychological support are factors that significantly impact the patients' weight loss. Male patients tended to have a greater final weight loss compared to female patients. Considering this result, it is suggested that men tend to lose more weight compared to women so as not to develop cardiovascular diseases such as hypertension, congenital heart disease, acute myocardial infarction, cardiac arrhythmias, and others.
The analysis of weight loss over time was carried out according to the patient's level of physical activity at the end of the study using the Kruskal-Wallis Test as a tool to compare measurements between groups. This test, according to Almeida et al.57 is a non-parametric statistical test used for the purpose of comparing three or more populations. It is adopted with the aim of testing the null hypothesis that all populations present, as well as equal distribution functions against an alternative hypothesis of different distribution presented by two of the populations studied. If the result obtained is a p-value ≤ 0.05, the hypothesis can therefore be considered null and thus rejected.
It was found that, for women, practicing moderate physical activity helps with weight loss, showing variation in BMI and WHR, unlike men, where physical activity seems to be less relevant. This suggests that the muscle mass of men and women, as they are different, present different results when it comes to practicing physical activities to reduce weight and fat.
The study showed that the influence of age and physical activity on weight loss, participants between 31 and 40 years old showed differences, but, on the other hand, a difference was noted in the percentage of weight loss, with a value of p = 0.045, showing that practicing moderate physical activity contributes to weight loss compared to those who do not practice or practice light physical activity.
When analyzing weight over the months, a progressive reduction trend can be seen, indicating an average reduction of approximately 1.5 kg each month, demonstrating the effectiveness of ESG. This result corroborates a study by Sander13 carried out on this procedure with 189 patients who underwent endoscopic gastroplasty and found that it is a method that is 87.5% effective for sustained weight loss in up to five years.
The analysis of the BMI results shows that as the months progress, the differences between consecutive months seem to increase, indicating a reduction in BMI over time and proves that some comparisons present greater differences in relation to others. Thus, it was noted that patients' BMI tends to decrease over time, with significant differences between months.
The study showed that the influence of time on WHR remained constant at approximately 0.9, that is, stability or little variation in this measurement for patients. However, it is important to point out that the minimum value fluctuated between 0.7 and 0.8 and the maximum varied between 1.0 and 0.7 over the months.
Notably, the results obtained over 12 months on weight loss and risk of cardiovascular diseases in patients undergoing endoscopic suturing were positive, as the patients who participated in this study showed a tendency to reduce their average weight during the period analyzed. Furthermore, it was observed that the patient's gender and psychological support are factors that significantly impact weight loss, with male patients showing a greater tendency towards greater final weight loss compared to women. But, on the other hand, the practice of physical activity showed more significant effectiveness in females. These results corroborate a study by Sander (2022) when analyzing 189 patients with obesity, concluding that ESG was safe, effective and with good durability in the corresponding period between 12 and 48 months, together with nutritional and psychological monitoring, presenting a positive effect on weight loss.
The results achieved are corroborated by the study by Nava et al.45 who analyzed a treatment group against obesity consisting of 154 patients to be evaluated for 24 months, with a mean age of 44.9±9.5 (23-69) and pre-procedure BMI of 383.3 +5.5 (30-47). After two years, they concluded that endoscopic suturing was an effective and safe technique for treating patients with obesity, without the emergence of cardiovascular risks.
It was also observed the influence that changing eating habits, physical activities and psychological support have on the nutritional profile of obese people who wish to lose weight, considering that they are predictors for remaining obese due to having several risk factors, generally, sedentary lifestyle, inadequate diet and others. Given this context, considering existing alternatives to treat and combat obesity is a way to contribute significantly to the treatment and prevention of obesity.
Regarding the existing treatment alternatives against obesity, there are, among others, physical activities, psychological support to control weight and compulsion to eat, diet, behavior change, drugs and, considering the patient's reality, in cases where obesity is severe, bariatric surgery for stomach reduction is recommended. However, for those who have already gone through several attempts and failed to achieve the desired result, ESG has proven to be a promising method, still relatively new in Brazil.
It was found that ESG consists of a complete suture made on the gastric wall using endoscopy, with no need for cuts or hospitalization of the patient, making it possible to perform endoscopic gastroplasty. It also provides the patient with a quick recovery and low risk of complications, in addition to presenting, in the end, satisfactory weight loss.
Last but not least, it is necessary to explain that this study had some limitations. The first was the fact that national literature is still scarce in relation to the number of publications on ESG, which is relatively recent in Brazil. The second limitation was the difficulty in maintaining the same number of patients since the beginning, which was 212. However, throughout the study, many patients did not return for consultation and as a result, the number of participating patients fell to 87 and, therefore, it was necessary to work with this final number.
ESG using overstitch ® demonstrated, in this study, to be a safe and effective procedure for weight loss and reducing the risk of cardiovascular diseases, over a 12-month follow-up period.

©2024 Machado, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.