eISSN: 2373-6372


Research Article Volume 14 Issue 4
Correspondence: Hany R Shabana, Assistant Professor of Hepatology and Gastroenterology, Internal Medicine Department, Specialized Medical Hospital, Faculty of Medicine, Mansoura University, Mansoura, Egypt, Tel +201060396985
Received: May 16, 2023 | Published: August 16, 2023
Citation: Mohammed Saad MAE, EL-Moniem SMA, Ibrahim DA et al. The validity of I-Scan in diagnosis of gastroesophageal reflux disease. Gastroenterol Hepatol Open Access. 2023;14(4):118-125. DOI: 10.15406/ghoa.2023.14.00556
Background: The evaluation of patients with suspected gastroesophageal reflux disease (GERD) frequently represents a diagnostic dilemma. Confirmation of the presence of the esophogeal mucosal injury is one of the roles of endoscopy in GERD diagnosis. In this context, there are limitations of white light endoscopy (WLE) because of the inadequate visualization of the minute mucosal changes and the uncertainty in describing the severity of mucosal injury. I-SCAN technology helps in revealing fine details of the GI mucosa.
Aim: to evaluate the diagnostic efficacy of I-SCAN technology as compared to white light endoscopy (WLE) in Egyptian patients suffering from GERD symptoms.
Patients and methods: This study included adult patients with GERD questionnaire (Q) score ≥ 8 points. The distal esophagus was examined by WLE followed by I-SCAN 2 to evaluate the presence of mucosal injuries and to classify GERD severity according to the Los Angles (LA) classification & its Japanese modification, respectively. Biopsies were taken from the lower esophageal mucosa as well as from the visible mucosal breaks and subjected to histopathologic examination.
Results: Sixty patients were enrolled; 32 (53.3%) were females & 28 (46.7%) were males. WLE showed erosive reflux disease (ERD) in 41 patients (68.3%); while 19 patients (31.7%) showed no mucosal breaks. As regard LA classification; 18 of the cases were classified as grade A (30%); 15 as grade B (25%); 7 as grade C (11.7%) and 1 as grade D (1.7%). Re-examination of distal esophagus by I-SCAN 2 showed minimal change esophagitis (MCE) (grade M) & ERD in 57 patients (95%); while only 3 patients (5%) showed no mucosal changes (grade N). As regard the modified LA classification; 16 cases were classified as grade M (26.6%); 12 as grade A (20%); 21 as grade B (35%); 7 as grade C (11.7%) and 1 as grade D (1.7%). There was perfect agreement of WLE with I-SCAN 2 in LA grades B, C & D. There was poor agreement of WLE with I-SCAN 2 in cases who had no mucosal breaks & LA grade A cases on WLE (weighted Kappa was 0.11); as 16 cases were reclassified as grade M on I-SCAN 2 (had no mucosal breaks on WLE) and 6 cases were reclassified as class B on I-SCAN 2(were classified as grade A on WLE). As regard the histological proven reflux esophagitis (HPRE), it was present in 41 (68.3%) of the studied cases with statistically significant higher proportion of male gender. It was present in 28 (68.3%) of the patients who had ERD on WLE; 13(68.4%) of the patients who had no mucosal breaks on WLE; 38 (66.6%) of the cases who had grade M or ERD on I-SCAN 2 & the three patients who had grade N on I-SCAN 2.GERD Q score ranged from 10 to 12 points with median of 11 points. It was significantly higher in patients with HPRE (11.4±1.8 points) than those without (10.3±1.3 points) (p= 0.026). GERD Q score strongly correlated with both the modified LA grade by I-SCAN 2 (p=0.03) and the histological severity score (p=0,016). On univariate & multivariate analysis, male gender and GERD Q score > 11points were significant predictors of HPRE (p < .001). ROC analysis curve showed that GERD Q score at a cut-off > 11points was a significant predictor of HPRE with a sensitivity of 47%, specificity of 85%, AUC of 66.7% and p = 0.015.
Conclusion: I-SCAN technology may improve the diagnosis of the esophogeal mucosal injury in GERD patients. There was poor agreement of WLE with I-SCAN 2 in patients who had no mucosal breaks & those with LA grade A on WLE. However, there was perfect agreement of WLE with I-SCAN 2 in patients with LA grades B, C& D. GERD Q score had positive correlation with both the modified LA grade on I-SCAN 2 and the histological severity score. Male gender and GERD Q score > 11points were significant predictors of histological proven reflux esophagitis.
Keywords: GERD, GERD questionnaire, I-scan, white light endoscopy, histological proven reflux esophagitis, modified LA classification, erosive reflux disease & Egypt
AI, artificial intelligence; AUC, area under the curve; BE, barrett's esophagus; COR, crude odds ratio; CI, confidence interval; CE, contrast enhancement; CSS, combined severity score; EoE, eosinophilic esophagitis; ERD, erosive reflux disease; FH, functional heartburn; GEFV, gastroesophageal flap valve; GERD, gastroesophageal reflux disease; GERD Q, gastroesophageal reflux dis4,ease questionnaire; GI, gastrointestinal; H&E, hematoxylin and eosin; HPRE, histological proven reflux esophagitis; IQR, interquartile range; I-SCAN OE, I-SCAN optical enhancement; LA classification, Los Angeles Classification; MCE, Minimal Change Esophagitis; OR, odds ratio; PPI, proton pump inhibitors; r1; reference category; RE, reflux esophagitis; SE, surface enhancement; SD, standard deviation; SE, the standard error; TE, tone enhancement;VC, virtual chromoendoscopy; WLE, white light endoscopy
According to the Montreal consensus; gastroesophageal reflux disease (GERD) is a chronic condition that develops when the reflux of the gastric contents into the esophagus causes troublesome recurrent symptoms and or complications.1 The evaluation of patients with suspected GERD is difficult and complex. Diagnostic tests are neither sensitive nor specific for definitive diagnosis.2 The role of upper gastrointestinal (GI) endoscopy in GERD is to confirm the diagnosis, evaluate for GERD complications (Barrett’s esophagus or peptic strictures) and to detect a potential alternative diagnosis.3 However, there are major limitations of white light endoscopy (WLE) in GERD diagnosis. In non erosive reflux disease (NERD), minute mucosal changes are not adequately visualized by WLE.4 In addition, the uncertainty in describing the severity of mucosal injury can lead to a poor inter-observer agreement.5 Currently, imaging technologies have been applied in endoscopy to improve detection and differentiation of subtle mucosal changes within the GI tract using digital contrast methods that provide the capability of filtering specific wavelengths of light; such as I-SCAN (Pentax).6 I-SCAN technology is a dynamic image enhancement technology that can enhance the endoscopic view regarding both the texture and architecture of the mucosal surface and vascular network.7 There are three I-SCAN settings which include I-SCAN 1 mode, using only surface enhancement (SE) to refine imaging of minute surface abnormalities without altering the brightness of the endoscopic picture for detection of lesions, I-SCAN 2 mode, using an algorithm that combines both SE and tone enhancement (TE) to show enhanced fine mucosal changes and vascular structures for characterization of lesions and I-SCAN 3 mode which digitally adds blue color to darker edges within the image of the examined field and adds contrast enhancement (CE) to the obtained image (with both SE and TE) for demarcation of lesions.8 So, I-SCAN can provide higher resolution and image modulation which can improve the diagnosis of erosive reflux disease (ERD). It may increase the detection of minute esophageal mucosal changes in patients who showed no mucosal breaks on WLE.9
Aim of the work: To evaluate the diagnostic efficacy of I-SCAN technology as compared to white light endoscopy (WLE) in Egyptian patients suffering from GERD symptoms.
This was a hospital based study that was conducted at Endoscopy Unit, Internal Medicine Department, Specialized Medical Hospital, Mansoura University; from January 2020 till October 2021. Adult patients with symptoms suggestive of GERD including heartburn, regurgitation, disturbed sleeping because of heartburn and/or regurgitation & chronic unexplained dry cough who were able to provide an informed consent were included in the study. Exclusion criteria included inability to stop acid suppressive therapy before endoscopy, evidence of cancer or mass lesion in the esophagus, presence of active upper gastrointestinal (UGI) bleeding, severe uncontrolled coagulopathy, prior history of esophageal or gastric surgery, decompensated cirrhosis, portal hypertension, pregnancy, endoscopic evidence of biliary reflux, chronic pancreatitis and uncooperative or excessively apprehensive patient. Complete history and thorough GERD symptoms review using GERD Q score were done (Table 1). All patients were asked to recall their symptoms and the frequency of their occurrence over the past 7 days. The questionnaire is composed of 6 items; heartburn, regurgitation, disorders related to sleep, use of over-the-counter medications (positive predictors), nausea and epigastric pain (negative predictors). Patient answered each question using a scale from 0 to 3 for positive predictors and from 3 to 0 for negative predictors. The sum of the points for the mentioned symptoms served as a subject’s GERD Q scores. The maximum score that can be obtained was 18 and a score equal to or more than 8 was considered positive for GERD.10 Five hundred patients attending the endoscopy unit were evaluated for eligibility. Fifteen patients were excluded due to inability to stop acid suppressive therapy before endoscopy,111 patients were excluded because of low GERD Q score (< 8), 32 patients were excluded due to presence of active upper gastrointestinal bleeding,106 patients were excluded due to decompensated cirrhosis, 10 patients were excluded due to past history of esophogeal and or gastric surgery, 7 patients were excluded due to severe coagulopathy,121 patients were excluded due to presence of portal hypertension,6 patients were excluded due to pregnancy, 9 patients were excluded due to biliary reflux,7 patients were excluded due to esophogeal cancer history & 16 patients were uncooperative. Sixty patients were enrolled and signed an informed consent prior to participation in the study (Figure 1). Basic laboratory investigations were done including complete blood count, coagulation profile & virology screen. Endoscopic examination was done using a Pentax Gastroscope with EPKi 5000 processor under conscious sedation with intravenous midazolam. A full WLE was performed first and a detailed examination of the squamo-columnar, gastroesophageal junction & lower esophogeal mucosa was done followed by activation of I-SCAN 2 mode by pressing the appropriate button at the endoscope control unit to re- evaluate the examined areas. All images were captured in a high resolution mode and stored for later evaluation by another endoscopist who was blinded to the reports of the first endoscopist. Patients with mucosal breaks identified by WLE were classified as erosive reflux esophagitis (ERD) and graded according to the LA classification (grade A, one or more mucosal breaks no longer than 5 mm, not bridging the tops of mucosal folds; grade B, one or more mucosal breaks longer than 5 mm not bridging the tops of mucosal folds; grade C, one or more mucosal breaks bridging the tops of mucosal folds involving <75% of the circumference and grade D, one or more mucosal breaks bridging the tops of mucosal folds involving >75% of the circumference).11 Patients with no visible mucosal break on WLE were recorded. Mucosal breaks & subtle distal esophageal mucosal changes were carefully evaluated with I-SCAN 2 and graded according to the LA classification system with Japanese modification.12 The modified LA classification added grades N and M. Grade N represents absence of the findings of esophagitis, while grade M represents minimal change esophagitis (MCE) (blurring or irregular Z-line, erythema, whitish turbidty and minute mucosal breaks). At the end of the procedures, biopsy specimens were obtained from lower esophageal mucosa as well as from the visible mucosal breaks and were sent for histopathologic examination. Microscopic changes of the distal esophageal mucosa were noted including basal cell hyperplasia, papillary elongation, dilated intercellular space and intraepithelial inflammatory cells according to the histological severity scores established by the Esohisto project in 2010 for the diagnosis of histologically proven reflux esophogitis (HPRE).13 The degrees of these microscopic changes were semi-quantitatively scored as normal (scores 0-0.25), mild oesophagitis (scores 0.5-0.75), severe esophagitis (scores ≥1). Histopathologic evaluation was performed by one experienced pathologist.
|
Question |
Points for symptom |
|||
|
|
Day |
|||
|
|
0 |
1 |
2-3 |
4-7 |
|
Positive predictors |
||||
|
How often did you have a retrosternal burning feeling? |
0 |
1 |
2 |
3 |
|
How often did you have regurgitations? |
0 |
1 |
2 |
3 |
|
How often did you have disturbed sleeping because of your heartburn and/or regurgitation? |
0 |
1 |
2 |
3 |
|
How often did you use of over-the-counter medications? |
0 |
1 |
2 |
3 |
|
Negative predictors |
|
|
|
|
|
How often did you have epigastric pain? |
3 |
2 |
1 |
0 |
|
How often did you have nausea? |
3 |
2 |
1 |
0 |
Table 1 The GERD questionnaire (gastroesophageal reflux disease questionnaire) 10
Ethical approval
The study protocol was reviewed and approved by the ethical committee at Faculty of Medicine in Mansoura University; the approval code was MS.18.12.420. The study was conducted in accordance with the Declaration of Helsinki and the consolidated Good Clinical Practice guidelines. Written informed consents were obtained from the patients after assuring confidentiality. All authors had access to the study data, and they all reviewed and approved the final manuscript.
Statistical analysis
Data were entered and analyzed using IBM-SPSS software (IBM Corp. Released 2019. IBM SPSS Statistics for Windows, version 26.0. Armonk, NY: IBM Corp.). Quantitative data were initially tested for normality using Shapiro-Wilk’s test with data being normally distributed if p > 0.05. Quantitative data were expressed as mean±standard deviation (SD) if normally distributed or median and interquartile range (IQR) if not. Qualitative data were expressed as frequency (N) and percentage (%).Qualitative data were compared by Chi-Square test (for large sample size ≥ 5 per cell) or Fisher’s exact test (for small sample size; < 5 in at least one cell). Quantitative data in two groups were compared by Independent-Samples t-Test (for normally distributed data in both groups) or its non-parametric equivalent; Mann-Whitney U test if data were not normally distributed in one or both groups. Cochran-Armitage test of trend was used to assess the association between one independent ordinal variable with one dependent dichotomous variable. The Spearman's rank-order correlation was used to assess the strength and direction of the association/relationship between two continuous variables if not normally distributed or between one continuous variable and one ordinal variable. Cohen’s kappa was used to assess interobserver agreement between two observers on a dichotomous variable. Weighted kappa was used to assess agreement between WLE and I-SCAN 2 in grading of GERD according to LA classification & Japanese modification. The univariate analyses and multivariate logistic regression analyses were conducted to determine predictors of HPRE. ROC curve was used for estimation of cut off level of GERD Q score in prediction of HPRE. For any of the used tests, results were considered statistically significant if p value was ≤ 0.05.
A total of 60 patients were enrolled in the study. Their age ranged from 30 to 59 years with a median age of 40 years; 32 of them (53.3%) were females and 28 (46.7%) were males. Current smoking was present in 16 patients (26.6%). Diabetes Mellitus was present in 10 patients (16.7%). Hypertension was present in 11 patients (18.3%). Regarding the residence, 35 patients (58.3%) lived in rural areas and 25 patients (41.7%) lived in urban areas. As regard the occupation, employee represented 45 % of the cases, housewives represented 41.6 %, 8.3 % were retired and 5% were students (Table 2).
|
Categorical characteristic (N=60) |
N (%) |
|
Age in years, median (range) |
40 (30-59) |
|
Sex: Male/Female |
28 (46.7%) / 32 (53.3%) |
|
Current smoking |
16 (26.6%) |
|
Diabetes Mellitus |
10 (16.7%) |
|
Hypertension |
11 (18.3%) |
|
Residence |
|
|
Rural |
35 (58.3%) |
|
Urban |
25 (41.6%) |
|
Occupation |
|
|
Employee |
27 (45%) |
|
Housewife |
25(41.6%) |
|
Retired |
5 (8.3 %) |
|
Student |
3 (5%) |
Table 2 Demographic characteristics of the studied cases
As regard patients’ symptoms, GERD Q score ranged from 10 to 12 points with a median score of 11points. As regard symptoms reported on the last week prior to inclusion; heartburn was reported in all patients (100%), regurgitation in 58 patients (96.7%), epigastric pain in 46 (76.7%), nausea in 36 (60%) and sleep disturbance in 34 (56.7%).Forty patients (66.7%) reported the use of acid suppressive therapy (Table 3).
|
Categorical characteristic |
N (%) |
|
GERD Q score, median (range) |
11 (10 – 12) |
|
Heartburn |
60 (100%) |
|
Regurgitation |
58 (96.7%) |
|
Epigastric pain |
46 (76.7%) |
|
Nausea |
36 (60%) |
|
Sleep disturbance |
34 (56.7%) |
|
Use of Over-the-Counter medications |
40 (66.7%) |
Table 3 Symptoms of the studied GERD cases
GERD Q score, gastroesophageal reflux disease questionnaire
WLE examination showed evidence of ERD in 41 patients (68.3%); while 19 patients (31.7%) showed no mucosal breaks.As regard LA classification, 18 cases were classified as grade A (30%),15 as grade B (25%), 7 as grade C (11.7%) and 1 as grade D (1.7%). As regard gastroesophageal flap valve (GEFV), 41(68.3%) patients had incompetent valve (grades III/IV) (Table 4).
|
Categorical characteristic |
N (%) |
|
Erosive reflux esophagitis (ERD) |
41 (68.3%) |
|
No mucosal breaks |
19 (31.7%) |
|
|
|
|
GERD LA class |
|
|
No mucosal breaks |
19 (31.7%) |
|
Grade A |
18 (30%) |
|
Grade B |
15 (25%) |
|
Grade C |
7 (11.7%) |
|
Grade D |
1 (1.7%) |
|
Hill's type of GEFV |
|
|
Type 1 |
4 (6.7%) |
|
Type 2 |
15 (25%) |
|
Type 3 |
25 (41.7%) |
|
Type 4 |
16 (26.7%) |
|
Trachealization |
2 (3.3%) |
Table 4 Endoscopic findings of the studied cases by WLE
ERD, erosive reflux esophagitis; GERD, gastroesophageal reflux disease; WLE, white light endoscopy; GEFV, gastroesophageal flap valve
Re-examination of distal esophagus by I-SCAN 2 showed minimal change esophagitis (MCE) (grade M) & ERD in 57 patients (95%); while only 3 patients (5%) showed no mucosal changes (grade N). As regard the modified LA classification, 16 cases were classified as grade M (26.6%), 12 as grade A (20%), 21 as grade B (35%), 7 as grade C (11.7%) and 1 as grade D (1.7%) (Table 5). I-SCAN 2 was also able to detect minimal change esophagitis (MCE) such as minute mucosal breaks in 25 cases (41.7%), erythema in 44 (73.3%), whitish turbidity in 21 (35%), irregular Z-line in 42 (70%) , blurred Z-line in 10 (16.7%) and columnar islands in 5 cases (8.3%) (Table 5 Photo 1).
|
Categorical characteristic |
N (%) |
|
Reflux esophagitis(ERD) |
57 (95%) |
|
No mucosal changes (Grade N) |
3 (5%) |
|
The modified GERD LA class (I-SCAN 2) |
|
|
Grade N |
3 (5%) |
|
Grade M |
16 (26.6%) |
|
Grade A |
12 (20%) |
|
Grade B |
21 (35%) |
|
Grade C |
7 (11.7%) |
|
Grade D |
1 (1.7%) |
|
Minute mucosal breaks |
25 (41.7%) |
|
Erythema |
44 (73.3%) |
|
Whiti urbidity |
21 (35%) |
|
Smooth Z-line |
3 (5%) |
|
Irregular Z-line |
42 (70%) |
|
Blurred Z-line |
10 (16.7%) |
|
Columnar islands |
5 (8.3%) |
Table 5 Endoscopic findings of the studied cases by I-SCAN 2
ERD, erosive reflux esophagitis; GERD, gastroesophageal reflux disease; LA, los angeles classification
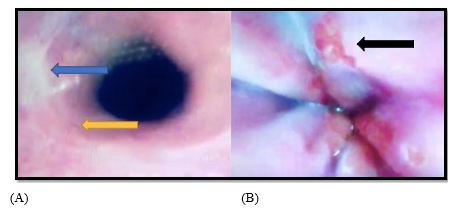
Photo 1 Minimal change esophagitis (MCE) observed through I-SCAN 2 (A) whitish turbidity (blue arrow) with blurring of Z-line (yellow arrow) (B) Columnar islands (black arrow).
There was perfect agreement of WLE with I-SCAN 2 in LA grades B, C& D. There was poor agreement of WLE with I-SCAN 2 in patients who had no mucosal breaks & LA grade A cases on WLE & weighted Kappa (WK) was 0.11. In 19 patients who had no mucosal breaks by WLE, 16 cases were reclassified as class M on I-SCAN 2 (Table 6, Photo 2). In 18 patients who were graded as LA class A by WLE, 6 cases were reclassified as class B on I-SCAN 2 (Table 6, Photo 3). However, the overall Agreement between WLE and I-SCAN 2 was good (WK = 0.66) (Table 7).
|
LA class (WLE) |
|
|||
|
No mucosal breaks |
Grade A |
Total |
||
|
The modified LA class (I-Scan 2) |
No mucosal changes (Grade N) |
3 |
0 |
3 |
|
Grade M |
16 |
0 |
16 |
|
|
Grade A |
0 |
12 |
12 |
|
|
Grade B |
0 |
6 |
6 |
|
|
Total |
19 |
18 |
37 |
|
|
Weighted Kappaa |
0.11713 |
|||
|
Standard error |
0.06349 |
|||
|
95% CI |
-0.00731 to 0.24159 |
|||
Table 6 Agreement of WLE with I-SCAN 2 in grading of GERD (LA classification & its Japanese modification)
WLE, White Light Endoscopy; GERD, Gastroesophageal Reflux Disease; LA, Los Angeles Classification
|
Modified LA grading by I-SCAN 2 |
LA grading by WLE |
Test of significance |
|||||||
|
No mucosal breaks |
A |
B |
C |
D |
Weighted k |
SE |
95% CI |
||
|
N |
3 |
0 |
0 |
0 |
0 |
0.66514 |
0.06115 |
0.545 - 0.785 |
|
|
M |
16 |
0 |
0 |
0 |
0 |
||||
|
A |
0 |
12 |
0 |
0 |
0 |
||||
|
B |
0 |
6 |
15 |
0 |
0 |
||||
|
C |
0 |
0 |
0 |
7 |
0 |
||||
|
D |
0 |
0 |
0 |
0 |
1 |
||||
Table 7 Agreement of WLE with I-SCAN 2 in grading of GERD (LA classification)
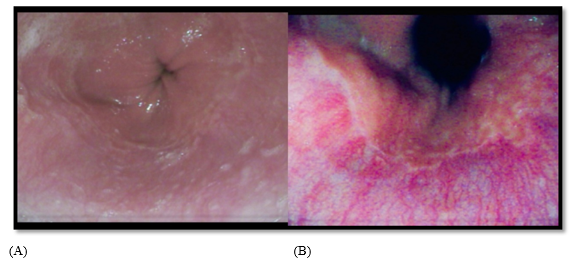
Photo 2 (A) No mucosal breaks by WLE (B) minimal change esophagitis (MCE) as seen by I-SCAN 2 of same patient (irregular Z-line, minute mucosal breaks, erythema & whitish turbidity), modified LA grade M.
WLE, white light endoscopy; LA, Los Angeles classification
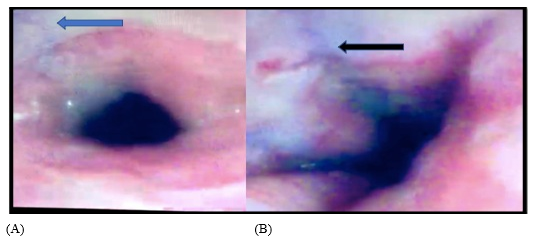
Photo 3 (A) LA class grade A by WLE (blue arrow), (B) Reclassified to grade B on switching to I-SCAN 2 (black arrow).
WLE, white light endoscopy; LA, Los Angeles classification
Histopathologic examination of distal esophageal biopsies was normal in 19 patients (31.6%), while mild reflux esophagitis was present in 32 patients (53.3%) and severe reflux esophagitis was present in 9 patients (15%) (Photo 4). Barrett’s esophagus (intestinal metaplasia) and eosinophilic esophagitis was noted in only 1 case (1.7%) for each (Table 8).
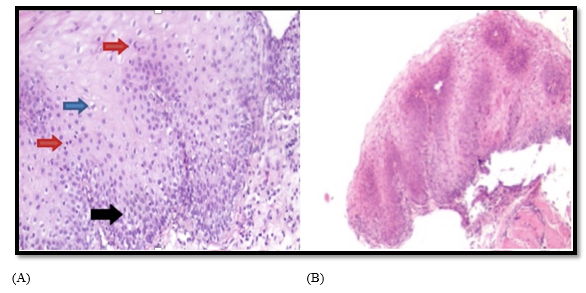
Photo 4 (A) Mild reflux esophagitis with mild basal cell hyperplasia (15-30 %) (black arrow), dilation of intracellular spaces (˂1 lymphocyte) (blue arrow) & intraepithelial mononuclear cells (10-30 cells) (red arrows) (H&E X 400), (B) Severe reflux esophagitis with basal cell hyperplasia (˃30%), papillary elongation (˃75%) & dilation of intracellular spaces (˃1 lymphocyte) (H&E X 100).
|
Categorical characteristic |
N (%) |
|
Histological severity score |
|
|
Normal |
19 (31.6%) |
|
Mild esophagitis |
32 (53.3%) |
|
Severe esophagitis |
9 (15%) |
|
Barrett’s esophagus (intestinal metaplasia) |
1 (1.7%) |
|
Eosinophilic oesophagitis (eosinophils ≥ 15/HPF) |
1 (1.7%) |
Table 8 Histopathologic findings of the studied cases
Overall, HPRE was present in forty one patients representing 68.3% of the studied cases .Forty one patients (68.3%) showed ERD on both WLE; 28 (68.3%) of them showed histological proven reflux esophagitis (HPRE) while 13 (31.7%) of them did not have HPRE. Nineteen patients had no mucosal breaks by WLE, 13(68.4%) of them showed HPRE, while 6 (31.6%) of them did not have HPRE. Fifty seven patients (95%) showed grade M & ERD on I-SCAN 2, 38 of them (66.6%) showed HPRE while 19 of them (33.3%) did not have HPRE. Three patients had no mucosal breaks by both WLE & I-SCAN 2(Grade N) and had HPRE (Table 9).
|
ERD by WLE (N=41) |
No mucosal breaks by WLE (N=19) |
|||
|
HPRE (Yes) |
HPRE (No) |
HPRE (Yes) |
HPRE (No) |
|
|
Grade M& ERD by I-SCAN 2 (N=57) |
28 |
13 |
10 |
6 |
|
No mucosal changes by I-SCAN 2 (Grade N) |
No |
No |
3 |
No |
Table 9 Distribution of HPRE in relation to different endoscopic modalities
WLE, White Light Endoscopy; ERD, Erosive reflux esophagitis; HPRE, Histological Proven Reflux Esophagitis
A statistically significant positive correlation was found between GERD Q score and both histological severity score (p=0.016) and modified LA classification by I-SCAN 2 (p=0.030), but there was no significant correlation between GERD Q score and LA class by WLE (p=0.204) (Table 10).
|
Grading system |
Correlation coefficient (r) |
P value |
|
Histological severity score |
0.311 |
0.016 |
|
GERD LA class (WLE) |
0.166 |
0.204 |
|
GERD modified LA class (I-SCAN 2) |
0.28 |
0.030 |
Table 10 Correlation between GERDQ score and both endoscopic and histological severity score
R, spearman’s correlation coefficient; WLE, white light endoscopy; GERD, gastroesophageal reflux disease; LA, Los Angeles classification
The Cochran-Armitage test of trend showed a statistically significant linear trend, with higher GERD modified LA class by I-SCAN 2 associated with a higher proportion of patients suffering from GERDQ≥10 (p=.033) (Table 11).
|
Dichotomous |
Ordinal |
|
|
LA class by WLE |
LA class by I-SCAN 2 |
|
|
GERD Q |
0.408 |
0.033 |
Table 11 Correlation between LA class (WLE & I-SCAN) and GERD Q scores
GERD Q score, gastroesophageal reflux disease questionnaire; WLE, white light endoscopy; GERD, gastroesophageal reflux disease; LA, Los Angeles classification
There was statistically significant higher proportion of males in patients with HPRE (p= 0.003). GERD Q score was significantly higher in patients with HPRE (11.4±1.8 points) than those without (10.3±1.3 points) (p= 0.026).There was no significant differences between those with and without HPRE regarding residence, smoking, GERD duration, presence of DM or hypertension (Table 12).
|
Characteristic |
HPRE (Yes) |
HPRE (No) |
P value |
|
Sex |
|||
|
Male |
25 (41.6%) |
3 (5%) |
0.003 |
|
Female |
16 (26.6%) |
16 (26.6%) |
|
|
Residence |
|||
|
Urban |
18 (45%) |
7 (35%) |
0.459 |
|
Rural |
22 (55%) |
13 (65%) |
|
|
Current smoking |
13 (32.5%) |
3 (15%) |
0.148 |
|
Disease duration (years) |
3 (1 – 5) |
3 (1.3 – 5) |
0.792 |
|
GERD Q score (points) (Mean ± SD) |
11.4 ± 1.8 |
10.3 ± 1.3 |
0.026 |
|
Diabetes mellitus |
4 (10%) |
6 (30%) |
0.07 |
|
Hypertension |
7 (17.5%) |
4 (20%) |
1 |
Table 12 Comparisons of the history including GERD Q score of those with and without HPRE
HPRE, histologically proven reflux esophagitis; GERD Q score, gastroesophageal reflux disease questionnaire; SD, standard deviation
Univariate analysis showed that male gender and GERD Q score > 11 were statistically significant predictors of HRPE, while modified LA class of GERD by I SCAN 2 was not (Table 13). On multivariate analysis, the model incorporating male gender and GERD Q score>11 was statistically significant (c2 [2] = 15.857, P <0.001). The model correctly classified 78.3% of cases, with sensitivity, and specificity of 82.5%, and 70%, respectively. Both variables were statistically significant independent predictors of HRPE. Male patients and GERD Q score>11 points have 6.8, and 6-times higher odds to exhibit HRPE, respectively (Table 14). GERD Q score at a cut-off>11 points was a statistically significant predictor of HPRE with a sensitivity of 47%, specificity of 85%, AUC of 66.7% and p = 0.015 (ROC curve, (Figure 2)).
|
P value |
COR |
95% CI |
P value |
OR |
95% CI |
|
|
Sex |
||||||
|
Female |
0.006 |
r(1) |
r(1) |
0.005 |
r(1) |
r(1) |
|
Male |
|
6 |
1.7-21.3 |
|
6.8 |
1.8-26 |
|
GERD Q score |
|
|
|
|
|
|
|
≤11 |
0.02 |
r(1) |
r(1) |
r(1) |
r(1) |
|
|
>11 |
|
|
|
0.017 |
6 |
1.4-26 |
|
Modified LA class (I-SCAN 2) |
0.228 |
1.5 |
0.76-3.1 |
- |
- |
- |
Table 13 Predictors of the likelihood of HPRE
COR, crude odds ratio; CI, confidence interval; OR, odds ratio; r (1), reference category; GERD Q score, gastroesophageal reflux disease questionnaire; LA, Los Angeles classification
|
Variable (I-SCAN 2) |
Kappa |
SE |
P value |
|
Minute mucosal breaks |
0.529 |
0.201 |
0.015 |
|
Erythema |
0.625 |
0.195 |
0.005 |
|
Whitish turbidity |
0.737 |
0.17 |
0.001 |
Table 14 Inter observer agreement for dichotomous variables

Figure 2 ROC curve for GERD Q score diagnostic performance in HPRE.
GERD Q score, gastroesophageal reflux disease questionnaire; HPRE, histologically proven reflux esophagitis; AUC, area under the curve
Statistically significant agreement was found between the two observers in diagnosing minute mucosal breaks, erythema & whitish turbidity by I-SCAN 2 (Table 14) and in grading reflux esophagitis by LA classification & its Japanese modification by both WLE & I-SCAN 2 respectively (Table 15).
|
Variable |
Weighted kappa |
SE |
95% CI |
|
LA classification by WLE |
0.834 |
0.062 |
0.713-0.955 |
|
Modified LA classification by I-SCAN 2 |
0.938 |
0.042 |
0.856-1.000 |
Table 15 Inter observer agreement for ordinal variables
LA, Los Angeles classification; WLE, White light endoscopy; SE, standard error; CI, confidence interval
The main benefit of the upper GI endoscopy in GERD diagnosis is direct visualization of the oesophageal mucosa which helps in detection of the complications such as esophagitis, strictures and Barrett’s esophagus.14 However, one of the limitations of conventional WLE is the inability to detect the minute mucosal changes in MCE.15 Endoscopic technologies have evolved tremendously with the emergence of image-enhancing technologies which aim at overcoming the limitation of WLE, specially the detection of minimal mucosal injury.7 I-SCAN technology is one of the advanced imaging technologies that have been applied in endoscopy to improve detection and differentiation of subtle mucosal changes. It consists of three modes of image enhancement which include surface enhancement (SE), contrast enhancement (CE), and tone enhancement (TE). It can provide higher resolution of the images with image modulation to improve the evaluation of GI mucosa.16 The present study included 60 GERD patients; 53.3% were females & 46.7% were males with male to female ratio of 1:1.1. However, there was statistically significant higher proportion of males in patients with HPRE. This may be explained by the fact that estrogen has a protective role through increasing the esophageal mucosal resistance by expression of tight junction proteins as mentioned by Kim et al.17 GERD Q score of the studied cases ranged from 10 to 12 points with a median score of 11 points. This was similar to those found in the validations and baseline estimates of GERD Q in different populations. For example, in the initial Diamond study by Dent et al, where the questionnaire was developed, a GERD Q score of ≥8 points had sensitivity and specificity of 64.6% and 71.4% respectively in GERD diagnosis.18 The present study showed that the most common presenting symptoms were heartburn & regurgitation. In a similar study conducted on 1,031 GERD patients aiming to asses the clinical presentation in GERD, heartburn and regurgitation were the most common presenting symptoms.19 As regard the WLE findings, erosive reflux disease was detected in 68.3% of the cases, while 31.7% showed no visible mucosal breaks. According to the LA classification, grade A was the most common followed by grade B, then grade C and lastly grade D. In concordance with our study, Hunter et al found that reflux esophagitis was present in 63.7% patients, most of them had grade A followed by grade B and 35.1% of the patients had normal esophagus.20 The present study showed that the mucosal breaks could be seen more easily and clearly with I-SCAN 2 than with a conventional WLE. This can be explained by the ability of I-SCAN 2 to improve the visualization of the squamo-columnar junction through enhancing the contrast between the oesophageal and gastric mucosa as noted by Kang et al.21. In the present study, mucosal injury was detected in 95% of the cases upon switching to I-SCAN 2 mode, while only 5% showed normally appearing mucosa. The most common grade according to the modified LA classification using I-SCAN 2 mode was grade B followed by grade M , then grade A and lastly grades C &D,. There was perfect agreement of WLE with I-SCAN 2 in LA grades B, C& D, while there was poor agreement of WLE with I-SCAN 2 in patients who had normal mucosa or LA grade A by WLE as evidenced by low weighted Kappa (WK) .In this study, 16 cases were reclassified as class M on I-SCAN 2 after initial absence of mucosal breaks by WLE & 6 cases were reclassified as class B on I-SCAN 2 after initial classification as grade A by WLE.This can be explained by the ability of I-SCAN 2 examination to detect minimal changes like erythema, whitish turbidity, Z-line changes (blurring &irregularity) and columnar islands. This ability is attributed to intensification of the contrast between inflamed erythematous mucosa and the normal squamous epithelium during I-SCAN examination as noted by Kim et al.22 In a cohort study done on dyspeptic patients by Netinatsunton et al., minimal changes that were observed through I-SCAN (erythema , blurring of z line and micro erosions) were significantly higher in GERD group than in non-GERD group.23 On the contrary, Kim et al reported that the prevalence of minimal changes was not significantly different between patients with GERD and patients without GERD.24 The lack of a standardized definition for minimal changes, lack of definite gold standard tool for GERD diagnosis, different populations recruited, different endoscopic image technologies and the low inter-observer agreement for minimal changes visualization may account for different results. In agreement with our study, Hoffman et al.25 found that I-SCAN improved the detection rate of mucosal breaks. Two patients were upgraded from LA grade A to grade B, and three patients were reclassified to LA grade A after initial absence of mucosal breaks by WLE .However, there was no differences in advanced LA grades.26 Kang et al also reported that the diagnostic yield of reflux esophagitis was significantly higher by I-SCAN than WLE. Also, the detection rate of minimal changes was significantly higher by I-SCAN than WLE. However, the detection rate of LA grades A, B and C didn’t show significant difference between both modalities.21 The difference between studies could be related to variable factors related to patients, examiners and endoscopy. In the present study, HPRE was present 68.3% of the studied cases. Similarly, El. alawy et al found that microscopic esophagitis was present in 52.5% of patients.27 In the current study, regarding the patients who showed mucosal injury on I-SCAN 2, HPRE was present in 66.6% of them. In agreement with our study, Medranda et al. found that 80% of patients who showed evidence of esophagitis at I-SCAN had HPRE and 20 % had normal epithelium.28 In the current study, 52% of the patients who had no mucosal breaks on WLE showed evidence of minimal change esophagitis by I-SCAN 2 and HPRE .Chu et al found that I-SCAN detected more minimal changes in NERD patients than functional heartburn (FH) and the control group and that pathologic changes related to acid reflux were found in NERD patients but not in patients with FH and control subjects.29 This denotes that I-SCAN can help in distinguishing NERD patients from those with FH without the need for further diagnostic tests. The present study showed that 5% of the patients had no mucosal injury on both WLE & I-SCAN 2 but showed HPRE. This finding is in agreement with that of Rey et al.who reported that very few numbers of patients had reflux related histological changes of the oesophageal mucosa despite absence of endoscopic evidence of esophagitis, even on I-SCAN.30
The present study showed that there was near perfect agreement between the two observers regarding LA classification by I-SCAN and WLE. This is consistent with Kang et al. study which showed a good inter-observer agreement for LA classification by I-SCAN but moderate agreement by WLE.21 As regard the inter-observer agreement for MCE detected by I-SCAN 2 in the present study, there was moderate agreement between the two observers in diagnosing minute mucosal breaks, erythema and whitish turbidity. Similarly, Sottisuporn et al. showed a good inter-observer agreement for minimal changes by I-SCAN in their study.25 In the present study, male gender & GERD Q score >11 were statistically significant predictors of HPRE. In the histo GERD trial, they validated the histological criteria as defined in the Esohisto project, demonstrating that histology is significantly associated with male sex and patient symptoms.31 Furthermore, we found a statistically significant positive correlation between GERD Q score and both Histological severity score and modified LA classification by I-SCAN.The main limitation of the current study was the relatively small sample size. So, further studies including larger number of GERD patients should be done to confirm these findings.
I-SCAN technology may improve the diagnosis of the oesophageal mucosal injuries in GERD patients. There was poor agreement of WLE with I-SCAN 2 in patients who had no mucosal breaks & LA grade A on WLE .There was perfect agreement of WLE with I-SCAN 2 in LA grades B, C& D. Significant positive correlation was found between GERD Q score and both histological severity score and the modified LA classification of GERD by I-SCAN 2. Male gender and GERD Q score > 11 were statistically significant predictors of histological proven reflux esophagitis.
None.
The authors declare no conflicts of interest

©2023 Mohammed, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.