eISSN: 2373-6372


Research Article Volume 12 Issue 2
Department of Pediatric Gastroenterology & Nutrition, Bangabandhu Sheikh Mujib Medical University, Bangladesh
Correspondence: Rafia Rashid, Postal address: C6, 85 Bashiruddin Road, Kalabagan, Dhaka 1205, Bangladesh, Tel +8801819420570
Received: March 15, 2021 | Published: April 15, 2021
Citation: Rashid R, Karim BASM, Rukunuzzaman, et al. Serum phosphate level as a predictor of outcome in children with acute liver failure. Gastroenterol Hepatol Open Access. 2021;12(2):37-40. DOI: 10.15406/ghoa.2021.12.00454
Objectives: Clinical and laboratory predictors of recovery in children with acute liver failure (ALF) are limited. Recent studies reported hypophosphatemia as a laboratory indicator of recovering liver function. Hence, this study aimed to record serum phosphate levels and to identify its predictive relationship with clinical outcome.
Methods: This cross-sectional descriptive study was conducted at the Department of Paediatric Gastroenterology & Nutrition, Bangabandhu Sheikh Mujib Medical University, Bangladesh, from 2017 to 2019. Twenty-one patients were selected purposively. Parents gave informed consent during recruitment. Demographic data, vaccination history, and other information regarding etiology and complications were recorded. Serum bilirubin, albumin, creatinine, electrolytes, prothrombine time, were carried out as required during the hospital stay. Serum phosphate levels were measured at admission and two days apart whenever possible. Fisher's exact test determined the association between hypophosphatemia and clinical outcome. Logistic regression was performed to analyze the predictive relationship between serum phosphate level and recovery.
Results: More than half (52.4%) of the studied patients died. Among the studied patients, Hepatitis A virus infection was the most frequent cause. Clinical outcome was significantly associated with hypophosphatemia (p = 0.009). Hypophosphatemia was usually found in patients who died. Logistic regression showed significant (p = 0.017) predictive relationship between serum phosphate level and recovery. This result indicates that with one mg/dL increase in serum phosphate level, the odds of recovering are higher by a factor of 3.605.
Conclusions: This study concludes that serum phosphate levels may be a good predictor of clinical outcome in children with ALF.
Keywords: paediatric hepatology, liver function test, hypophosphatemia, serum bilirubin, albumin, creatinine, electrolytes
ALF, acute liver failure; SD, standard deviation; INR, international normalised ratio
Acute liver failure (ALF) is a fatal disorder in previously healthy children, despite improvements in intensive care management and the development of other therapeutic modalities. Clinical and laboratory recovery predictors for children with ALF are limited. Identification of the predictors of outcome is an issue of central importance in the management of ALF. Encephalopathy, metabolic acidosis, increasing serum levels of bilirubin, and ammonia have all been associated with lower survival rates in these patients. Recent studies reported hypophosphatemia as a laboratory indicator of recovering liver function in children with ALF.
Serum phosphate level, along with other prognostic factors such as total serum bilirubin, serum albumin, serum creatinine, the grade of encephalopathy, can help to predict the clinical outcome of children with ALF as well as guide decisions regarding further management. The serum phosphate level was chosen due to inexpensive and easy to perform laboratory procedures.
No study regarding the predictors of outcome of ALF has been conducted in Bangladesh. Therefore, this study aimed to determine the frequency of hypophosphatemia in children with ALF in the study place; and analyze the relationship between serum phosphate level and clinical outcome in those patients.
Study procedure
This cross-sectional descriptive study was conducted at the Department of Paediatric Gastroenterology & Nutrition, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh during the period 1st May 2017 to 30th April 2019. Twenty-one samples were selected according to the inclusion and exclusion criteria. During recruitment, study objectives were explained to the parents, and written consent was taken. Demographic data, vaccination history, and other related information regarding etiology and complications were recorded in a standard datasheet. Serum bilirubin, albumin, creatinine, electrolytes, prothombine time, international normalised ratio (INR) were carried out as required from admission until the patient spontaneously recovered or died or referred for orthotopic liver transplantation. Serum phosphate level (mg/dL) was measured on admission as well as two other follow-ups. The first follow up was within 3 to 5days after admission, and the second follow up was within 5 to 7 days after admission. For all computation and analysis, the lowest value of serum phosphate level among these values was analyzed. Hypophosphatemia or low serum phosphate level was determined at a phosphate level that is at least 2 standard deviation (SD) below the mean for the age of the child. Table 1 below summarizes the mean serum phosphate level for different age ranges.
Statistical analysis
Collected data were checked manually and analyzed by computer-based program IBM SPSS Statistics (version 24.0). The association between hypophosphatemia and clinical outcome (recovered or died) was determined using Fisher’s exact test. Here, the dependent variable (clinical outcome) is binary (died or recovered), and the independent variable (serum phosphate) is continuous. Therefore, logistic regression was performed to analyze the predictive relationship between serum phosphate level (mg/dL) and recovery.
Ethical issue
Every ethical concern was discussed with the parents. Parents were informed about the nature and purpose of this study, procedures, associated risks, and benefits from this study in the understandable local language. They were also informed about the right to participate or withdraw from the study at any time. Then a written consent was obtained from the parents of each child to be included in the study. Every precaution was taken so that the study will not cause any harm or delay in the treatment.
Twenty-one patients were enrolled in this study. The majority (62%) of the studied patients belonged to the 5-10 year age group. The mean age was 9±3.4years, with ages ranged from 4-16years. More than half (62%) of these patients were male, and the remaining 38% were female. Among these studied patients, more than half (52.4%) of the patients died (Table 2). The etiology of ALF of these patients varies; Wilson Disease and infection with Hepatitis A virus were the most common causes (Table 2). About 57.1% of patients had a history of taking street food or unsafe water. Only 6 (28.6%) patients had a history of ingestion of herbal medicine. None of the patients had any history of vaccination against Hepatitis A. Only 19% of studied patients had a family history of liver disease.
|
Age range |
Mean±SD of serum phosphate level |
|
0 to <2years |
5.6±0.7mg/dL |
|
2 to <5years |
5.2±0.8mg/dL |
|
5 to <12years |
4.6±0.8mg/dL |
|
12 to <16years |
3.8±0.6mg/dL |
Table 1 Mean serum phosphate level with age5
|
Age(years) |
9±3.4 |
|
Gender |
|
|
Male |
13(62%) |
|
Female |
8(38%) |
|
History |
|
|
History of taking street food or unsafe water |
12(57.1%) |
|
History of ingestion of herbal medicine |
6(28.6%) |
|
History of vaccination against Hepatitis A |
0(0%) |
|
Family history of liver disease |
4(19%) |
|
History of vaccination against Hepatitis B |
16(76.2%) |
|
Outcome |
|
|
Recovered |
10(48%) |
|
Died |
11(52%) |
|
Etiology |
|
|
Hepatitis A virus |
8(38%) |
|
Wilson Disease |
7(33.3%) |
|
Coinfection with multiple hepatotropic viruses |
4(19%) |
|
Indeterminate |
2(9.5%) |
Table 2 Cross-tabulation of age, gender, history, outcome, and etiology of studied patients(n=21)
Only 4 (19%) patients had moderate level of anaemia. Physical examination revealed jaundice in all the patients. The liver was palpable in 71.4% patients, and 33.3% of patients had palpable spleen. Only 2 (9.5%) patients had tense ascites. Clinical features of coagulopathy (bleeding from any site) were present in 81% of patients. Encephalopathy was absent in 28.6% of patients. The majority (57%) had grade I & II encephalopathy, and only 1 (4.8%) patient had grade IV encephalopathy. Among the haematological parameters, INR more than 2.3 was found in 71.4% of patients. Hb and platelet count were within the normal range for the majority of the studied patients.
Among the biochemical parameters studied, serum ALT was raised in 91% of patients, and serum bilirubin was high (> 3mg/dL) in 86% of patients. Serum creatinine and electrolytes were within normal limits, as observed in 10 patients.
Association of hypophosphatemia with clinical outcome
Eleven patients (52.4%) out of the total of 21 studied patients demonstrated hypophosphatemia.
The association of hypophosphatemia with clinical outcome was significant as the p-value from Fisher’s exact test was 0.009, and hypophosphatemia was found more common in patients who died (Table 3). This is also a strong association since the value of Cramer’s V was 0.618 for 1 degree of freedom.
|
Variable |
Clinical outcome |
p value |
|
|
|
Died(n=11) |
Recovered(n=10) |
|
|
Hypophosphatemia |
|
|
0.009 |
|
Present |
9(81.8%) |
2(20%) |
|
|
Absent |
2(18.2%) |
8(80%) |
|
Table 3 Association of hypophosphatemia with clinical outcome for studied patients (n=21)
The predictive relationship between serum phosphate level and recovery
The beginning block of logistic regression for this distribution showed that the regression model is 52.4% accurate if it always predicts outcome as died. After applying serum phosphate data as an independent variable in the logistic regression, classification accuracy was increased from 52.4% to 76.2%, and statistically significant (p = 0.017) result was found. This result also states that with one unit (i.e., 1mg/dL) increase in serum phosphate level, the odds of recovering is higher by a factor of 3.605.
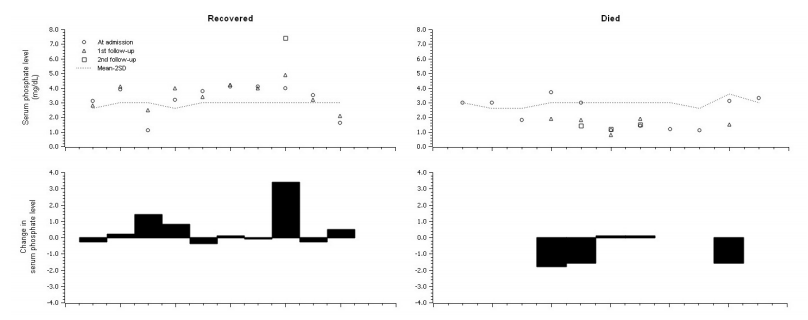
Figure 1 Serum phosphate level and change in serum phosphate level of studied patients [Top-Left: serum phosphate level (mg/dL) of recovered patients. TopRight: serum phosphate level (mg/dL) of died patients. Bottom-Right: change in serum phosphate level of died patients. Bottom-Left: change in serum phosphate level of recovered patients.]
Association of other parameters with clinical outcome
The association of clinical outcome with other essential parameters were calculated using the Chi-Square test of independence. The association between INR and clinical outcome was statistically significant (p = 0.004), and the effect size was large (Cramer’s V value was 0.663). The association of clinical outcome with other parameters like encephalopathy, coagulopathy, Serum ALT, Serum Bilirubin was not statistically significant.
The current study stated that Hepatitis A virus infection was the most commonly found underlying cause in ALF children aged 5 to 10 years. This finding was similar to the previous studies who found that viral hepatitis was the most common identified cause both in Bangladesh and in the Indian subcontinent.1,2 These school-going children are more vulnerable to taking unhygienic street foods and unsafe water. Also, Hepatitis A vaccination is not included in the government provided vaccination schedule in Bangladesh.
According to Squires, children are increasingly exposed to a variety of over-the-counter, prescription, and herbal medications as well as environmental toxins and recreational drugs.3 The present study also found that 28.6% of patients had a history of ingestion of herbal medicine. In this study among the patients with poor outcomes, Wilson Disease was the most common cause; and among the patients who recovered, hepatitis A virus infection was the most common cause. This finding is similar to an earlier study by Mazumder et al.1
In terms of outcome after hospital admission, many ALF patients had complications such as infections and multiple organ failures, which causes high mortality and required high cost for management. Identification of patients who have poor survival outcomes is essential for prompt referral and consideration for emergency liver transplantation. Previous studies showed that encephalopathy, extrahepatic organ failure (especially renal failure), and coagulopathy were poor prognostic factors for mortality.1 In this present study, both encephalopathy and coagulopathy were present in 95.2% of patients who died.
Nanji and Anderson first reported hypophosphatemia in the case of ALF.4 After that, various studies reported hypophosphatemia in adult and pediatric patients with ALF and hepatic resection. The latter studies suggested that hypophosphatemia may be the consequence of liver regeneration.5 In this present study, it was found that all the patients had significantly lower serum phosphate levels than the mean of their respective age groups.
According to Quirós-Tejeira et al.,6 a total of 39 children who spontaneously recovered experienced profound hypophosphatemia that resolved as the synthetic function of the liver improved.6 Serum phosphate levels improved to the normal range immediately after the full recovery of synthetic hepatic function. Similar patterns were seen in the 29 identified children who recovered after liver transplantation.6 Phosphate levels improved towards normal levels immediately after liver transplantation. In the current study as well, 60% of patients among those who spontaneously recovered showed an increase in serum phosphate levels towards the average value of their age group. Rest 40% of patients had no significant change in Serum phosphate level during their hospital stay. This finding also resonates with the findings of Dawson et al.7 According to them, low phosphate concentrations returned to the average level spontaneously in recovered cases.7
Baquerizo et al.8 hypothesized that the maximal rate of ATP synthesis in the liver might be impaired in patients with low serum phosphorus, and that administration of supplemental phosphate may prevent the decrease in ATP synthesis, facilitating the regeneration of liver cells and improving the outcome of patients with ALF.8 According to Schmidt and Dalhoff, patients with acute liver failure often required phosphate supplements.9 It has been suggested that uncorrected hypophosphatemia may contribute to the manifestations of liver failure or may even be a cause of acute liver failure.9 In the study of Dawson et al., supplements of phosphate were given intravenously to two patients whose plasma concentration was low.7 Baquerizo et al.8 hypothesized that acute hypophosphatemia as a result of an abrupt shift of phosphorus into the liver might result in clinically significant manifestations because free phosphate becomes unavailable for the generation of intracellular ATP.8 Aggressive early phosphorus administration after major hepatic resections has been shown to decrease postoperative hypophosphatemia and the incidence of significant complications.8 George and Shiu showed that phosphorus replacement on the first day after major hepatic resections had a significant protective effect, increasing serum inorganic phosphorus and decreasing the number of significant complications.10 Studies in right-lobe living-related orthotopic liver transplantation donor showed that repletion with parenteral phosphorus at 60mmol per day, twice the recommended daily allowance (30mmol/day), reduced the incidence of hypophosphatemia and morbidity.11
In the present study, phosphorus supplementation was not administered to any patient. Hence those patients with very low serum phosphate levels may fail to recover spontaneously. This finding is aligned with the studies mentioned above.
The main limitation of this study was that it was a single-center study with limited intensive care facilities. It would be more interesting if daily levels of serum phosphate can be monitored.
The predictive relationship between serum phosphate level and recovery was significant. Hence, this study concludes that serum phosphate levels may be a good predictor of clinical outcome in children with acute liver failure. This study also recommends future prospective multi centered studies to investigate further the role of phosphorus as a predictor of outcome in ALF and to determine whether or not aggressive early phosphorus repletion can improve outcomes.
We want to thank all the faculties, fellowship students, residents, and staff of the Department of Pediatrics Gastroenterology & Nutrition of BSMMU, Dhaka, Bangladesh, for their technical and administrative assistance. We also want to thank all the parents of our patients who were very cooperative throughout the study period.
The authors did not receive any grant for this research study.
We, the authors declare that we have no conflicting interests.

©2021 Rashid, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.