eISSN: 2373-6372


Case Report Volume 13 Issue 3
Department of Surgery, Inspira Health Network, USA
Correspondence: David Kelter, Resident Physician, Department of Surgery, Inspira Health Network, 1505 West Sherman Avenue, Suite B,Vineland, NJ, 08360, Tel 856-641-8635, Fax 856-641-8636
Received: June 05, 2022 | Published: June 22, 2022
Citation: David K, Alexandria M, Hsu-Tsai C. Portal vein thrombosis and pylephlebitis following laparoscopic appendectomy in a patient with esophageal varices. Gastroenterol Hepatol Open Access. 2022;13(3):108-110. DOI: 10.15406/ghoa.2022.13.00507
Pylephlebitis is defined as infectious suppurative thrombosis of the portal vein. The etiologies of pylephlebitis are variable, however, nearly all cases represent a rare albeit serious complication of an intraabdominal infectious process due to the regional portal venous system drainage. Appendicitis is a well-documented cause of pylephlebitis. A 1995 review of 19 cases of reported pylephlebitis demonstrated appendicitis as the second most common pre-disposing etiology in the development of pylephlebitis, with Bacteroides and E. coli being the most commonly cultured organisms. The utility of therapeutic anticoagulation following diagnosis is presently undetermined.
We describe a case of pylephlebitis presenting 5 days status post laparoscopic appendectomy for uncomplicated acute appendicitis in a 62-year-old adult male with a history of cirrhosis and esophageal varices. Considering the patient’s history of cirrhosis and resultant esophageal varices, this uncertainty regarding the use of anticoagulation was particularly problematic. Given the lack evidence-based guidelines, a multidisciplinary approach weighing the risks and benefits of systemic anticoagulation was employed. Ultimately, the decision was made to proceed with therapeutic anticoagulation under close supervision with serial imaging to identify thrombus propagation and/or recanalization. While the patient did not demonstrate evidence of recanalization after 58 days of therapy, the throm-bus did indeed fail to propagate further. Clarification regarding the utility of anticoagulation in the setting of pylephlebitis in conjunction with risk stratification based on individual patient factors is certainly warranted to optimize future clinical outcomes.
Keywords: pylephlebitis, portal vein thrombosis, appendectomy, cirrhosis, esophageal varices
Pylephlebitis is defined as infectious suppurative thrombosis of the portal vein. The etiologies of pylephlebitis are variable, however, nearly all cases represent a rare albeit serious complication of an intra-abdominal infectious process due to regional portal venous system drainage. Appendicitis is a well-documented cause of pylephlebitis.1 A 1995 review of 19 cases of reported pylephlebitis demonstrated appendicitis as the second most common predisposing etiology in the development of pylephlebitis, with Bacteroides and E. coli as the most commonly cultures organisms.2 The utility of therapeutic anticoagulation following diagnosis is presently undetermined.3 We describe a case of pylephlebitis presenting 5 days status post laparoscopic appendectomy for uncomplicated acute appendicitis in a 62-year-old adult male with a history of cirrhosis and esophageal varices.
Patient is a 62-year-old male with a past medical history of hypertension, hepatitis C and hepatitis A, resultant cirrhosis, esophageal varices, and robotic left inguinal hernia repair in October 2020, who presented to the emergency department in April 2021 with a chief complaint of right lower quadrant abdominal pain associated with nausea and emesis for 36 hours. He was found to have significant leukocytosis of 24.2, in addition to CT findings demonstrating a dilated, fluid-filled appendix with a thickened wall, periappendiceal fat stranding, and trace fluid in the right lower quadrant. As such, the patient proceeded to the operating room the following morning for a laparoscopic appendectomy. Intraoperatively the patient was found to have a frankly necrotic distal appendix with a healthy base, in addition to a small amount of surrounding serosanguineous fluid. No evidence of perforation was noted, however, thrombosed periappendiceal vessels were visualized. The operation proceeded uneventfully, and the patient was discharged home the following day after demonstrating clinical stability, improved leukocytosis, and diet toleration. The pathology report resulted the second postoperative day with findings consistent with acute appendicitis. The serosal surface noted to be dark tan with exudative congestion. On postoperative day 5, the patient presented back to the emergency department with a chief complaint of intermittent fevers and right sided quadrant abdominal pain that abruptly began on postoperative day 3. In the emergency department patient was found to be febrile to 38.3 °C, normotensive, and tachycardic to 108 beats per minute. Labs demonstrated leukocytosis of 28.8, normal liver function tests, and slightly elevated creatinine at 1.2. A CT of the abdomen and pelvis with IV contrast was obtained which demonstrated mild phlegmonous changes and fat stranding present in the right lower quadrant. The scan was additionally significant for thrombosis of the right portal vein and its branches, which represented a new finding in comparison to the prior CT obtained preoperatively. Blood cultures were obtained, and the patient was subsequently admitted to the surgical acute care unit. He was immediately started on IV Ceftriaxone and Metronidazole, in addition therapeutic anticoagulation with a heparin infusion. Consults were placed to hematology, vascular surgery, gastroenterology, and infectious disease (Figure 1).
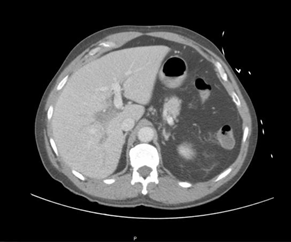
Figure 1 CT Abdomen and Pelvis with IV contrast demonstrating new-onset right portal venous thrombosis on postoperative day 5.
Given the patient's history of hepatitis C, resultant cirrhosis and esophageal variceal disease, a multidisciplinary discussion was held regarding the use of anticoagulation. After careful consideration the decision was made to continue anticoagulant therapy given the possible benefit of improved recanalization and portal venous pressures. The patient's general clinical picture of pylephlebitis/infectious burden, immobility, hospitalization and recent surgery, was felt to represent a high-risk scenario for propagation and non-recanalization of the thrombosis given the patient’s overall hypercoagulable state. An MRI was obtained on post-operative day 7 for further monitoring of the portal venous thrombosis and demonstrated a patent left portal, superior mesenteric, and splenic vein, without further propagation of the right portal venous thrombosis. Over the following 3 days, the patient remained intermittently febrile with steadily improving while continuing intravenous antibiotics and anticoagulation. His liver enzymes reached a peak on post-operative day 10, with an ALT 77 AST 130 and ALP 138, which rapidly improved to within normal limits thereafter. Blood cultures obtained on admission ultimately resulted positive for Bacteroides distasonis on post-operative day 11. The patient demonstrated marked clinical improvement and remained afebrile for 48 hours between post-operative days 10-12. On post-operative day 12, normalization of liver function tests and leukocytosis was noted. The decision was made at this point to discharge the patient home, with an additional 7-day prescription for levofloxacin 750 mg once daily and metronidazole 500 mg 3 times daily. The patient was additionally instructed to continue therapeutic anticoagulation in the form of apixaban 10 mg twice daily for 7 days, followed by 5 mg twice daily thereafter, with close outpatient follow-up with hematology to determine total anticoagulant therapy duration. The patient was additionally advised to follow up closely with his gastroenterologist for monitoring of his esophageal variceal disease while on anticoagulation. A repeat MRI was obtained 58 days after initial diagnosis which demonstrated persistence of the right portal thrombosis without propagation or recanalization. As such, it was determined the patient would benefit from 3-6 months of total anticoagulant therapy in addition to repeat imaging prior to discontinuation.
Pylephlebitis is defined as an infective suppurative thrombosis of the portal vein and carries a significant risk of morbidity and mortality without prompt diagnosis and treatment. The portal vein is formed by the union of the superior mesenteric and splenic veins, and drains blood from the gastrointestinal tract with the exception of the lower rectum. Pylephlebitis initially begins with thrombophlebitis within the smaller veins of the splanchnic venous system, eventually extending into larger veins including the portal veins.4 If left untreated pylephlebitis may extend into the larger mesenteric veins, potentially leading to bowel ischemia, infarction, and death. While the frequency and prognosis of pylephlebitis remain unknown, diverticulitis has been described as common underlying etiology. In addition, pancreatitis, appendicitis, cholangitis, inflammatory bowel disease, and other intra-abdominal inflammatory and infectious processes may rarely result in development of septic portal thrombosis.5
Early recognition of pylephlebitis and subsequent treatment has improved over the past several decades, in part due to more advanced imaging techniques.2 Although Computed Tomography (CT) has an unknown sensitivity and specificity in the diagnosis of pylephlebitis, its advent has augmented earlier diagnosis and provides the added bene-fit of potential identification of the primary infectious source.6 Additional diagnostic accuracy may be ascertained via color doppler ultrasound. MRI, the use of which was described in this case, is an additional tool to characterize the extent of portal venous thromboses.5
The role of anticoagulation in the treatment of pylephlebitis remains undefined. In a 2010 case series, 81 cases of acute pylephlebitis dating back to 1971 were examined with 19 mortalities identified. In this case series, a portal venous thrombosis was found extending to the superior mesenteric, splenic, and portal veins into 42%, 12%, and 39% of cases, respectively. Patients were administered antibiotics in all cases, and therapeutic anticoagulation in 35 cases. The patients who received anticoagulation had favorable outcomes compared to those who received antibiotics alone (complete recanalization 25.7% vs 14.8% (p >0.05), no recanalization 5.7% vs. 22.2% (p <0.05), and death 5.8% vs 22.2% (p <0.01)).7 In a more recent case series from 2020, the records and outcomes of 67 consecu-tive patients diagnosed with pylephlebitis were reviewed. Outcomes assessed in this study included survival, portal vein thrombosis resolution, development of chronic symptomatic portal hypertension, and major bleeding. Of these 67 patients, 47 received anticoagulation. Interestingly, while those patients who were anticoagulated demonstrated significantly better rates of portal venous thrombosis resolution [58% vs 21% (p <0.02)], lower rates of future chronic portal hypertension [11% vs 47% (p <0.004)], there was no significant difference in survival observe on multivariable analysis.4
The uncertainty regarding the use of anticoagulation in this case was particularly problematic given the patient’s history of cirrhosis and resultant esophageal varices. Given the lack of evidence-based guidelines, a multidisciplinary approach weighing the risks and benefits of systemic anticoagulation was utilized. Ultimately, the decision was made to proceed with therapeutic anticoagulation under close supervision with serial imaging to identify thrombus propagation and/or recanalization. The patient was additionally instructed to follow up frequently on an outpatient basis with hematology and gastroenterology for continued evaluation of the necessity of anticoagulation and monitoring of gastroenterological risk factors for variceal bleeding. While the patient did not demonstrate evidence of recanalization after 58 days of therapy, the thrombus did indeed fail to propagate further. Clarification regarding the utility of anticoagulation in the setting of pylephlebitis in conjunction with risk stratification based on individual patient factors is certainly warranted to optimize future clinical outcomes.
None.
The author declares no conflicts of interest.

©2022 David, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.