eISSN: 2373-6372


Case Report Volume 6 Issue 3
1Departments of Hepatology & Gastroenterology, Mansoura University, Egypt
2Department of Radiology, Mansoura University, Egypt
3Clinical pathology, Mansoura University, Egypt
Correspondence: Monir Bahgat, MD, Hepatology & Gastroenterology division, Specialized Medical Hospital, Faculty of Medicine, Mansoura University, Gomhuria street, Mansoura 35516, Egypt, Tel +2-111-1196919, Fax +2-50-2230287
Received: December 23, 2016 | Published: March 8, 2017
Citation: Bahgat M, AboZeid FA, El-Etreby S, Elrakhawi M, EL-Mashad N (2017) Klebsiella-Related Paraspinal Abscess: A Rare Cause of Sepsis- Associated Cholestasis. Gastroenterol Hepatol Open Access 6(3): 00199. DOI: 10.15406/ghoa.2017.06.00199
Vertebral osteomyelitis with or without paraspinal abscess is a rare clinical condition, accounting for only 1-7% of all bone infections. Its incidence is rising especially in the elderly population with chronic debilitating diseases such as diabetes mellitus (DM). It has been known for many years that patients with non-hepatic infections can develop cholestasis. Therefore, we present a case of cholestasis that was caused by klebsiella-related paraspinal abscess as a rare non-hepatic infection caused by an atypical organism causing an atypical presentation in uncontrolled diabetic female.
Keywords: Klebsiella pneumonia, paraspinal abscess, Cholestasis, metastatic bone lesion, uncontrolled diabetes mellitus
RBG, random blood glucose; INR, International normalized ratio; LDH, lactate dehydrogenase; ALP, alkaline phosphatase; IgG, immunoglobulin-G; CRP, C–reactive protein; ANA, antinuclear antibody; ASMA, anti-smooth muscle antibody; LKM, liver kidney microsomal; AMA, anti mitochondrial antibody; ANCA, anti-neutrophilic cytoplasmic antibody; CBC, complete blood count; WBCs, white blood cell; HB, hemoglobin; MCV, mean corpuscular volume; HPF, high power field; CCU, coronary care unit; RV, right ventricle; KP, Klebsiella pneumoniae; DM, diabetes mellitus; US, ultrasonography; CT, computerized tomography; MRI, magnetic resonance imaging
A 48years old housewife, presented with jaundice two days after removal of ingrowing left lateral toe nails, it was associated with fever, dark colored urine, and normal colored stool. The condition was not associated with itching, vomiting or diarrhea. She is known diabetic since the last 10years on oral hypoglycemic agents and shifted to insulin 1year ago. She had disc prolapse in the lumbosacral region 3years ago, that needed just follow up and physiotherapy.
On examination she was clinically free apart from; dyspnea 35 breath/min and fever of 38.5˚. Her laboratory data on admission was illustrated in Table 1. Arterial blood gas showed hypoxia with CO2 wash, her ECG: showed sinus tachycardia and right axis deviation, trans-thoracic echo gave picture suggestive of pulmonary embolism (right ventricle (RV) pressure overload, “McConnell sign” defined as right ventricle free wall hypokinesia in the presence of normal RV apical contractility). Streptokinase was given under close monitoring in CCU.
S. bilirubin (mg/dl) |
13.6 (direct 9.7) |
ESR |
110 |
AST (mg/dl) |
36 |
CRP |
48 ( N <6) |
ALT (mg/dl) |
94 |
Coombs (direct & indirect) |
Negative |
S. albumin (g/dl) |
2.7 |
Anti cardiolipin IgM |
Negative |
S. sodium (mEq/l) |
127 |
Anti cardiolipin IgG |
Negative |
S. potassium (mEq/l) |
4.1 |
Lupus anticoagulant |
Negative |
S. creatinine (mg/dl) |
1.7 |
ANA |
Negative |
RBG (mg/dl) |
372 |
Anti-LKM |
Negative |
HB A1C (%) |
10 |
ASMA |
Negative |
INR |
1.03 |
AMA |
Negative |
LDH (IU/L) |
339 (1.5 UNL) |
ANCA |
Negative |
ALP (IU/L) |
221 (1.3 UNL) |
||
IgG (IU/L) |
1430 (700-1600) |
||
CBC |
|
Urine Analysis |
|
WBCs (/cmm3) |
8 |
glucose |
+++ |
HB (gm/dl) |
9.9 |
pus cells |
6/HPF |
MCV (fl) |
79 |
casts |
NIL |
Platelets (/cmm3) |
170 |
protein |
NIL |
Table 1 Laboratory investigations at time of admission
RBG, random blood glucose; INR, International normalized ratio; LDH, lactate dehydrogenase; ALP, alkaline phosphatase; IgG, immunoglobulin-G; CRP, C–reactive protein; ANA, antinuclear antibody; ASMA, anti-smooth muscle antibody; LKM, liver kidney microsomal; AMA, anti mitochondrial antibody; ANCA, anti-neutrophilic cytoplasmic antibody; CBC, complete blood count; WBCs, white blood cell; HB, hemoglobin; MCV, mean corpuscular volume; HPF, high power field
Pelvi-abdominal ultrasonography (US) showed enlarged liver with diffuse fatty infiltration, thick-walled gall bladder, moderately enlarged spleen with dilated splenic veins and hilar collaterals. There was an accidentally discovered well-defined isoechoic lesion in the posterior wall of the uterus about 4x4cm (fibroid). No evidence of Budd-Chiari Syndrome. Post contrast computerized tomography (CT) chest (2 days after streptokinase) demonstrated the presence of mild bilateral pleural effusion more on the right side with patchy areas of consolidation scattered in both lungs more on the right side likely pneumonic to be followed up.
Patient was started empirically on intravenous levofloxacin (500mg bid), meropenem (500mg once daily) and metronidazole (500mg t.d.s.) under strict control of blood glucose and close monitoring of serum creatinine. One week later, her fever subsided with normalization of serum bilirubin and creatinine associated with improvement of CBC. Later on, blood culture result yielded Klebsiella pneumoniae (KP) organism with high sensitivity to levofloxacin, imipenem and amikacin.
As patient still having backache, Magnetic Resonance Imaging (MRI) lumbo-sacral region was done to evaluate any deterioration in the disc prolapse state. Paraspinal mass was illustrated in MRI assessment (Figure 1) suggestive of metastatic lesion. So, bone scan was ordered to evaluate the nature of the lesion, and the results revealed neoplastic lesion involving L4 (Figure 2).
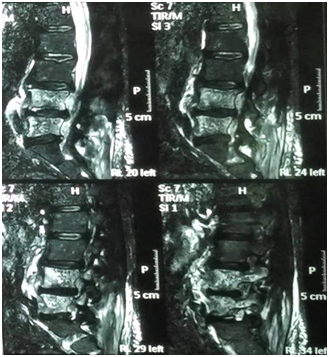

Figure 1 Non contrast MRI lumbosacral spine, bone marrow of L4 and L5 is seen replaced by abnormal SI in form of low SI on T1 and high SI on both T2 and STIR images?? Mostly metastatic lesion.

Figure 2 Bone scan, focal area of intense radioactive tracer uptake is seen the right pedicle of 4th lumbar spine?? Metastatic lesion otherwise the remained of scanned skeleton is free.
She was referred to a neurosurgeon, who decided to do an operation for this paraspinal mass that surprisingly was simply a bag of pus and fixation was done (Figure 3). After surgical drainage, cytopathological examination of the drained material was free of any malignant cells and culture of the drained pus confirmed the same organism and since then she was better.
Klebsiella pneumoniae which is a well-known frequent cause of lobular pneumonia rarely presents by vertebral osteomyelitis with or without paraspinal abscess.1 Meanwhile, only a few case reports with paraspinal abscesses caused by Klebsiella pneumoniae have been described in the literature.2–6
The pathogenic mechanisms of pyogenic spondylitis caused by KP have been unclear. However, DM is known to be the most common underlying condition among patients with pyogenic vertebral osteomyelitis7 and uncontrolled DM is considered as an important risk factor because of impaired phagocytosis of KP.8 This infection might spread locally to the myofascial tissues and epidural space or systemically leading to uncontrolled sepsis.9 In our case, the septicemia was noticed after surgical removal of ingrowing toe nails under a background of uncontrolled diabetic state.
Paraspinal abscess is most commonly caused by Staph. aureus (42–84% of cases)10 while KP , on the other hand, is rarely isolated. In our case, KP was isolated not only from the blood culture but also from culture of the drained paraspinal abscess and treatment with proper antibiotics continued for more than two weeks. It has been well-known that patients with a wide variety of non-hepatic infections can develop cholestasis which is not related to biliary obstruction but toxemia with an expected improvement of jaundice upon control of sepsis.11,12
This what exactly happened to our case with normalization of liver function tests by proper treatment of her sepsis. Imaging studies including plain x-ray and CT could be useful. However, MRI is the most sensitive, radioisotope is a helpful adjunct, and biopsy (either percutaneous needle or open surgical) is generally needed to confirm the clinical and/or radiographic suspicion. Samples should be sent for aerobic, anaerobic, mycobacterial and fungal culture and pathology.
In our case, MRI suggested metastatic bone lesion which was changed to a diagnosis of paraspinal abscess on surgery indicating the mandatory need for confirmation of the diagnosis through biopsy. Surgical drainage of the paraspinal abscess under coverage of systemic antibiotic was the treatment of choice in this case as reported in literature.13
Sepsis associated cholestasis is a common condition that might be caused by rare diseases. In this case, jaundice was caused by klebsiella-related paraspinal abscess. Another lesson from this case is that we should investigate every possible source of sepsis even if a clear diagnosis was previously established.
None.
The authors who have taken part in this study declared that they do not have anything to disclose regarding funding or conflict of interest with respect to this manuscript.
None.

©2017 Bahgat, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.