eISSN: 2373-6372


Mini Review Volume 6 Issue 3
Memorial Atasehir Hospital, Department of Gastroenterology, Turkey
Correspondence: Irfan Koruk, Department of Gastroenterology, Kucukbakkalkoy mh, Vedat Gunyol cd, No: 2834758 Atasehir, Istanbul, Turkey, Tel +90 216 5706666, Fax +90 216 570 66 20
Received: December 11, 2016 | Published: February 27, 2017
Citation: Koruk I (2017) How to Manage Difficult Cannulation in ERCP. Gastroenterol Hepatol Open Access 6(3): 00194. DOI: 10.15406/ghoa.2017.06.00194
Endoscopic retrograde cholangio pancreatography (ERCP) is still the gold standard for the diagnosis and management of biliary system diseases. The first major step of ERCP is the cannulation of the biliary and/or pancreatic duct. Success rate of ERCP is directly proportional with cannulation. In this review, the techniques for facilitating biliary/pancreatic cannulation in ERCP will be discussed. Of course there is a debate about “difficult” cannulation. Which one is “difficult?” and “difficult” to whom? The answers to these questions are subjective and differ from one to another. “Easy” cannulation for one endoscopist may be “difficult” for another. Morever, “difficult” and “easy” terminology can spur a discussion on relativity, such as “this was more difficult than the previous” or “this is the most difficult one I’ve ever seen!
There are different acceptations about “difficult” cannulation in the literature.1,2 Time or attempt number to reach cannulation may be the criterion. In one study cannulation was considered to be “difficult” if it failed after five or ten minutes.3 Attempt number independent of time or need for alternative cannulation methods are accepted as “difficult”. So we still don’t have a standard parameter for difficulty. In the literature approximately 11% of ERCPs are considered to be difficult cannulation.4
We can sort these factors as follows:
Factors depend on the patient, the endoscopist, as well as the availability of educated staff and adequate equipment. These are shown in Table 1.
Factors depends on patient |
Anatomic variations |
Altered anatomy |
Papillary anatomy |
Factors depend on endoscopist |
Case volume |
Experience |
Known maneuver/method alternativity |
Capability of thinking different alternatives |
Imagining duodenal anatomy in 3D |
Scope and instrument knowlegde |
Factors depend on staff and equipment |
Variation of equipments |
Experience of the staff |
Table 1 Factors for “difficult cannulation” in ERCP
The factors depend on the patient
Factors depend on the endoscopist
Factors depend on the staff and equipment
Other than standard cannulation techniques, the endoscopist may use advanced techniques in difficult cases. The advanced cannulation techniques can be divided in two categories: The first and second line alternative cannulation techniques. Endoscopists with limited experience can try the first line techniques. However, second line methods must only be used by experienced endoscopists. The decision about applying these second line methods depends on the indication, emergency situation, and the endoscopists experience. These methods are listed in Table 2.
First step methods |
Guide-wire cannulation |
Double (pancreatic) guide-wire cannulation |
“S” maneuver |
Double catheter cannulation |
Second step methods |
Precut over pancreatic stent |
Transpancreatik sphincterotomy |
Precut with needle knife sphincterotom |
Fistulotomy |
“Tip to top” precut |
Table 2 The alternative methods/techniques for failed standard cannulation
Guide-wire cannulation
In standard manner ERCP catheter or sphincterotomes may be used for cannulation. In this method tip of the catheter is placed at the orifice followed by two alternative methods for introduction. First one is injecting contrast medium slowly in order to see the biliary and pancreatic duct anatomy and then introducing the catheter deeply. The second way is after placing the tip of the catheter to the orifice, introducing the loaded guide-wire to the biliary duct. The angle and the direction of the wire will guide you to decide if you are in the bile duct or pancreatic duct. The post-ERCP pancreatitis is more common in the first method (contrast medium) than the second (guide-wire cannulation).5,6 Forcing the guide-wire roughly may cause pancreatitis, false-root or perforation and this must be kept in mind.
Pancreatic guide-wire cannulation
Sometimes in repeated attempts the guide-wire always goes into the pancreatic duct. In these situations you can use the double guide-wire technique.3,7 In this technique the wire is introduced to the body in the pancreatic duct, left, and then a secondary guide-wire loaded catheter is used to cannulate the bile duct. The wire in the pancreas will cause more stiffness in the papilla and facilitate access to the bile system.
Cannulation with “S” maneuver
Sometimes the bile duct follows an “S” type shape in the papilla. In this situation the wire or the catheter cannot be introduced deeply. In the standard position of the scope and the catheter, the wire always touches the upper wall of the duct. Thus, a different maneuver is needed. It is called as an “S maneuver” because of the shape of the bile duct. The most important thing in this maneuver is to imagine the papilla and duct in 3D. We use a wire-loaded sphincterotom. In the first step we place the tip of the sphincterotom at the orifice by flexing the cutting wire. In second step while slowly unflexing the cutting wire, we pull the duodenoscope back gently. In this way the “S” shape of the duct will be straightened. In the third step we unflex the cutting wire or the sphincterotom and pull the duodenoscope a little more and then introduce the guide-wire deeply.
Double catheter cannulation
This technique is suitable in the juxta-diverticular or hidden papilla. The working channel diameter of the therapeutic duodenoscope is 4.2mm. The ERCP catheter is 5 or 7F in diameter (1.9-2.1mm). If we want to use a double catheter, then we have to choose the 5F catheters. This technique can be summarized as follows (Figure 1). We use the first catheter in order to visualize the papilla which is hidden under the pili or towards the diverticulum. This catheter acts as a finger in order to make the orifice facing to the scope. Then we use the second wire-loaded catheter for cannulation in the standard manner.
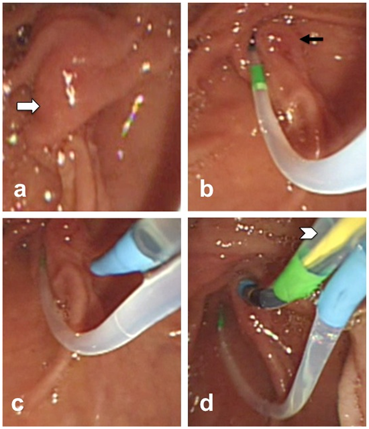
Figure 1 Double catheter method: a) Papilla hidden under the duodenal pili (white arrow), b) getting orifice an-face with the first catheter (black arrow), c) cannulation attempt with the second catheter, d) cannulation is achieved with the guide-wire in the second catheter (arrow head).
Precut over the pancreatic stent
In case of repeating pancreatic cannulation, placing a pancreatic stent to the pancreatic duct, and then applying a precut using a needle knife sphincterotom in order to access biliary tract will reduce the post-ERCP pancreatitis risk.8 The stent in the pancreas duct may stay after the procedure is completed in order to decrease pancreatitis risk.
Transpancreatic sphincterotomy
In cases with repeated pancreatic cannulation the guide-wire is placed in the pancreatic duct. A standard sphincterotom is then introduced towards the pancreatic duct. We apply a short cut through the medial side of the pancreatic duct. This axis will be parallel with the bile duct. This way the bile duct may be visible and this simplifies the biliary cannulation.9 The use of this technique depends on the experience of the endoscopist.
Precut with needle knife sphincterotom (NKS)
If standard techniques and maneuvers fail than NKS precut is thought to be another option for cannulation.10 The complication rate of this method is high and it must be used by experts. The definition of the method is for informational purposes only rather than encouraging readers. Use of the NKS precut technique without enough experience is not advised.11 NKS can be used in two different ways. First one is called as “fistulotomy”.12 We apply a puncture at the roof of the bulging papilla. This is especially suitable for the impacted stones and bulged papilla. By using “fistulotomy” it is easy to access the duct rather than cannulating from the orifice in the bulged papilla. Use of fistulotomy is not limited to this indication; it can be used in unsuccessful attempts of cannulation also.
The second way of NKS is the “tip to top” technique. This is shown in Figure 2. We start to cut from the tip of the orifice to the top. The needle is taken 2mm out, so as to make a mucosal incision. When we see the fibers of the sphincter (Figure 2c; white arrows) then we puncture it and cannulate the bile duct. An important factor in applying this precut is similarly imagining the papilla in 3D. This type of precut is like cutting butter with a hot knife. Sometimes a little oozing hemorrhage occurs and the incision site becomes invisible. In this situation never continue cutting or puncturing without a clear view. When biliary cannulation is achieved then change the NKS technique with a standard one over the guide-wire and continue in a standard way.
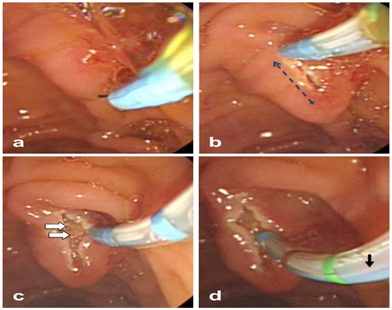
Figure 2 “Tip to top” precut with needle knife sphincterotom: a) the naïve form of the papilla, (note that the needle is not fully out), b) mucosal dissection from tip to top (dashed arrow); c) the visible fibres of the sphincter after dissection (white arrows); d) puncturing over the sphincter and cannulation (black arrow).
Both fistulotomy and papillotomy (tip to top technique) has similar success rates.13
Advanced alternative methods
Endoscopic papillectomy for biliary access is thought to be an alternative invasive method. Papillectomy is applying “polypectomy” to the papilla. By this way both biliary and pancreatic orifices become visible separately.14 This is an uncommon and advanced method, and can be tried possibly just for cases of ampullary tumor and adenomas. It should be noted that this technique is not a standard method and must be done in selected patients by experienced endoscopist.
Another advanced method is Endosonographic Cholangio Pancretography (ESCP). Nowadays endoscopic ultrasound (EUS) is being used commonly for biliary and pancreatic diseases. EUS guided biliary access and ESCP is useful especially in anatomically altered patients (e.g. Billroth II gastrectomy, Whipple operation, hepaticojejunostomy, etc.). Of course the details of this method are not the subject of this paper, however further reading can be found in the literature.15
Biliary cannulation directly affects the success rate and is one of the major steps of ERCP. There are both commonly known and rarely used techniques and methods for achieving biliary tract cannulation. These are mentioned above. It is important to know when and how to perform alternative methods depending on your experience and skill. Sometimes doing nothing makes more sense than anything else. If cannulation fails despite all of the above methods and techniques, referring the patient to a more experienced/skilled endoscopist/center may be an alternative. Similarly, if the indication and clinical status of the patient is adequate, waiting one or two days may resolve the edema in the papilla and simplify biliary access.“Difficult cannulation” alternatives are shown in the algorithm in Figure 3.
None.
The authors declare there is no conflict of interests.
None.

©2017 Koruk. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.