eISSN: 2373-6372


Review Article Volume 15 Issue 5
1Department of Pediatric Radiology of the 1-st State Hospital, Belarus
2Dorot. Medical Center for rehabilitation and geriatrics, Israel
Correspondence: Michael D Levin, Department of Radiology, Dorot, Medical Center for rehabilitation and geriatrics, Netanya, Israel
Received: November 20, 2024 | Published: December 2, 2024
Citation: Levin MD. Gastrointestinal motility and law of the intestine. Gastroenterol Hepatol Open Access. 2024;15(5):163-172. DOI: 10.15406/ghoa.2024.15.00595
Modern gastroenterology, which occupies the pages of scientific journals without an alternative, began as an initiative of manufacturers of equipment for pH monitoring. DeMeester et al, in contradiction to scientific research, suggested the possibility of gastroesophageal reflux, which does not damage the esophagus. Therefore, they began to perform pH research in the esophagus. This is how a group led by DeMeester arose, who in 1976 published the DeMeester score, i.e., the normal limit for esophageal pH monitoring. pH <4, less than 4% of the time per day was considered normal, i.e., it was unreasonably claimed that such reflux is physiological. However, this study was carried out with numerous methodological errors, which led to an erroneous conclusion. For a long time, pH monitoring was considered the gold standard and with its help hypotheses were proposed that form the basis of modern gastroenterology. Numerous articles using pH monitoring have publicized this method. When practice showed the low diagnostic efficiency of pH monitoring, devices for impedance pH monitoring were proposed, the principle of which was based on previous false ideas about the pathological physiology of reflux disease. As a control for determining the normal limits for high-resolution manometry (HRM), individuals were selected who claimed that they had no complaints. They did not undergo an objective study, including pH monitoring. Therefore, the results of HRM are not accurate and scientific. This article proves the fallacy of 13 hypotheses, which are presented as theories. Conclusion This study provides a list of hypotheses that were previously considered theories, but since scientific evidence has proven these assumptions to be false, they should be excluded from subsequent use and citation.
Keywords: gastroenterology; gastroesophageal reflux disease; x-ray diagnosis; pH monitoring; physiology; hypothesis.
In 1899, the famous English physiologists Bayliss and Starling published the law of the intestine, which explained peristaltic movement. This law almost immediately became one of the foundation stones of physiology about which there has never been any question or argument. In the first article the following statement was formulated. “Excitation at any point of the gut excites contraction above, inhibition below. This is the law of the intestine”.1 Cannon later proposed the term “myenteric reflex” the phenomenon and showed that it could at times be elicited also in the stomach.2
Currently, even though there has not been a single study that has cast doubt on the validity of the law of the intestine, there is no mention of it in the literature. Gastrointestinal motility is associated exclusively with high-resolution manometry (HRM), where there is no place for peristalsis and the laws of physiology. Control persons for HRM were selected only based on the absence of complaints. Since in a significant percentage of patients with peptic problems the disease proceeds and progresses without clinical manifestations, some percentage of patients with gastrointestinal problems were selected as controls. Secondly, HRM has not been studied in patients with different diagnoses. Thirdly, differences in physical characteristics (integrated relaxation pressure, the distal contractile integral, distal latency, the evaluation of the EGJ at rest, 'fragmented' contractions, ineffective esophageal motility) together with the erroneous norm have no physiological meaning.3 Their significance was determined by the vote and only therefore the results of HRM are not scientific, and therefore true. Thus, HRM is not a scientifically valid diagnostic method.4
The purpose of this review is to determine the motor function of the digestive system, using scientific research on the physiology and pathology of peristaltic organs, including the digestive tract with the bile-pancreatic system, as well as the urinary tract. Based on the above, research on HRM, as a scientifically unsubstantiated method, is not considered in this work.
Since the lower esophageal sphincter (LES) opens in response to a certain pressure above it, this pressure can be created in two ways. 1). In a horizontal position, in humans, as in all animals, a bolus of any consistency, equal to the volume of one swallow, moves along the esophagus, thanks to peristalsis, in full accordance with the law of the intestine (Figure 1a, b, c. d). 2) Liquid drunk in a vertical position forms a column above the LES. When the fluid level reaches D-4, hydrostatic pressure causes the LES to open, and the fluid falls into the stomach. The LES remains open until all fluid is released into the stomach. It does not close, even though in the process of decreasing the height of the column, the pressure over the sphincter progressively decreases. This indicates that the opening of the LES is not a mechanical, but a reflex process, which occurs because of contraction of the oblique muscles of the LES, on one side attached to the wall of the esophagus, and on the other side to the lesser and greater curvature of the stomach. The opening of the lumen of the LES is accompanied by its shortening.
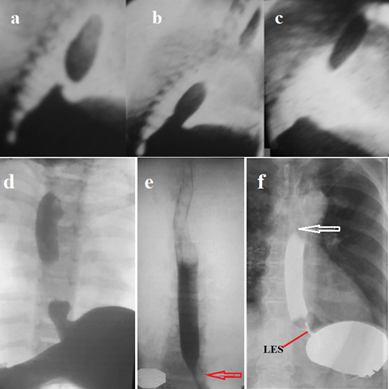
Figure 1 Variants of food move through the esophagus. (a, b, c) Video segments of peristaltic propulsion of a contrast bolus in a dog. d) In a person in a horizontal position, each bolus is advanced by peristalsis. The last peristaltic wave creates pressure, which opens the EGJ, and which is higher than the gastric one. e) In a vertical position during the intake of liquid barium, the LES (red arrow) opens under the influence of hydrostatic pressure and in this case, it remains open, despite the decrease in the length of the column, i.e., hydrostatic pressure. (f) In a horizontal position, with a sharp increase in pressure in the stomach, the LES remains open, but its length is 20% shorter than the minimum normal limit (3.2–4.2 (3.60±0.08 cm).5 The Esophagus is not dilated, and the force of the peristaltic wave (white arrow) overcomes the high tone of the LES caused by high pressure in the stomach.
The mechanism of the sphincters opening was chosen by the evolution of living organisms and is especially demonstrative during the opening of the pyloric sphincter. Contraction of the oblique fibers of the pyloric sphincter leads to the opening of its lumen, which is accompanied by its shortening. The fiber attachment sites cause expansion of the antrum and the base of the duodenal bulb.6 The mobility of the LES obeys the law of the intestine. An increase in pressure over the LES causes contraction of the segment above the bolus, and relaxation of the LES (see Figure 1d). The pressure (tone) of the LES decreases in response to stretching of the esophagus7,8 to allow the bolus to pass into the stomach. When the fundus or body of the stomach is distended the pressure (tone) of the LES increases to prevent reflux of aggressive gastric contents into the esophagus.9,10 The opening of the LES is a reflex phenomenon, which is accompanied by shortening of the sphincter by several millimeters. However, the esophagogastric junction does not move. There is no scientific evidence that the esophagus shortens when swallowing. An example of misinterpretation of an x-ray examination is the case described by Kwiatek et al.11 A patient with gastroesophageal reflux disease was examined as healthy, based on the absence of typical complaints. The abdominal part of the LES opened, causing the LES to become almost 2 times shorter, which is typical for a damaged LES in ГЭРБ patients.5 The authors regarded shortening of the “esophagus + LES” complex as shortening of the esophagus. The contrast clip attached to the esophageal mucosa during swallowing did not move relative to the vertebra. However, the authors argued that it rose, since they compared its position relative to the moving peristalsis (phrenic ampulla) (see Figure 2).
In healthy individuals, a contrast bolus swallowed in both a vertical and horizontal position penetrates the stomach within about 5 seconds, regardless of the pressure in the stomach. Since the adult human esophagus is 25–30 cm long, the peristalsis speed in the esophagus is ≈ 10 cm/sec.
Thus, the motor function of the esophagus and esophagogastric junction (EGJ) obeys the law of the intestine.
From a functional point of view, the stomach is divided into proximal and distal parts. The proximal part, including the fundus and the body of the stomach, provides reception and temporary storage of food. It regulates intragastric pressure and stimulates the tonic advancement of the chyme into the distal part. In addition, it provides space and time for pepsin and hydrochloric acid to act in the early stages of digestion. The fundus is characterized by tonic rather than peristaltic contraction.12 An important function of the proximal stomach is its ability to accommodate. More than a liter of food can enter the stomach without increasing intragastric pressure. A study of pressure on volunteers showed that intragastric pressure decreases moderately after eating and returns to the initial level as soon as solid food ingredients penetrate the duodenum.13s The motor function of the proximal stomach is regulated by reflexes: receptive relaxation and gastric accommodation. Receptive relaxation is manifested by a decrease in the tone of the proximal stomach during swallowing. For example, Shafik's study showed that «Pharyngeal distension produced a significant pressure drop of the corpus of the stomach (p < 0.05); the pyloric antrum shows no response. Upper, middle, or lower esophageal distension produced gastric response like that evoked by pharyngeal distension".14 Stomach accommodation is described as a relaxation reflex of the proximal stomach in response to distension. Unlike receptive relaxation, this reflex does not depend on the stimulation of the esophagus and pharynx. The method of evacuation of stomach contents depends on body position and volume of contents (Figure 2).
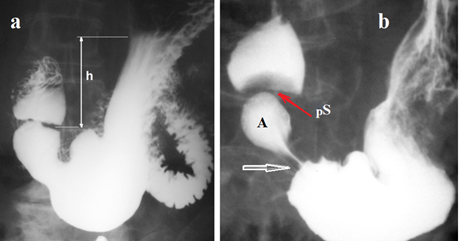
Figure 2 Stages of evacuation of the stomach in a vertical position. (a). The level of hydrostatic pressure (h) is sufficient to open the pyloric sphincter (pS). (b). When part of the contents of the stomach was evacuated into the intestine and the hydrostatic pressure decreased, pS is closed. In the antrum the peristaltic waves of the lesser and greater curvature of the stomach are converged, blocking the lumen of the stomach. A closed antral cavity (A) has developed between this antral sphincter (white arrow) and pS. The advancement of the peristaltic wave leads to an increase in pressure in the antral cavity. When it reaches the threshold pressure, the pS relaxes and the bolus enters the duodenal bulb. Normally, the volume of the bolus corresponds to the capacity of the duodenal bulb.
In a horizontal position, evacuation from the stomach is carried out using antral systole. In the distal part of the stomach, a negatively charged membrane potential is determined, on which rhythmic depolarization at three cycles per minute is superimposed. The frequency and direction of electrical activity is closely related to the slow peristaltic wave. There is evidence that the slow wave is generated by the phase depolarization of Cajal interstitial cells. These cells are located on the greater curvature of the stomach. The slow wave propagates a little faster along the greater curvature so that the myoelectric activity "running" along the greater and lesser curvatures of the stomach reaches the pylorus simultaneously.12,15 Only every 3-5 peristaltic wave closes, forming an antral chamber. The walls of the stomach and duodenal bulb are resistant to a certain level of hydrochloric acid. The mechanisms described above protect the esophagus from reflux of gastric contents. LES prevents reflux by: (1) strengthening its tone with increasing pressure in the body of the stomach; (2) low pressure is maintained in the fundus of the stomach by receptive relaxation and gastric accommodation; (3) the evacuation of the bolus from the stomach occurs at elevated pressure only in the antrum. Portioned evacuation from the stomach protects the duodenum from damage by hydrochloric acid.
Thus, the fundus and body of the stomach do not participate in peristalsis. They exhibit tonic relaxation and contraction. The different electrical properties of ICC-IM play a critical role in creating the distinct functions of the proximal and distal regions of the stomach such that the fundus acts as a reservoir of food, the corpus as a dominant pacemaker region, while the antrum acts as a region for mixing and propulsion of food.16 Below is evidence that the opening of the pyloric sphincter during antral systole occurs because of contraction of obliquely located longitudinal muscle fibers (Figure 3).
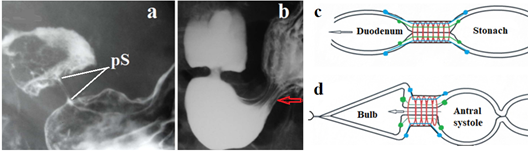
Figure 3 Radiographs of the gastroduodenal junction. (a) The pyloric sphincter (pS) is in a closed state. The width of the bulbus base is almost equal to that of the opposite side of the stomach. (b) At the moment of contraction of the antral cavity of the stomach (antral systole), when the pressure in it increases to a threshold level, a reflex opening of the pS occurs and its length decreases. (c) Schematic of the corresponding to the radiograph (a). (d) Schematic corresponding to the radiograph (b).
The duodenum is about 25 cm long and is located from the pyloric sphincter to the duodenojejunal sphincter. It is divided into 4 parts. The duodenal bulb is about 2 cm long, is the first part of the duodenum and is slightly dilated. It is at the vertebral level of L1. It has a bulb shape only on radiographs when filled with chyme from the stomach and the contraction of the postbulbar sphincter. The second part of the duodenum begins at the superior duodenal flexure. It goes down to the lower border of vertebral body L3, before making a sharp turn medially into the inferior duodenal flexure and ends near the descending part. The second part contains the Kapandji sphincter.17 In the second part, distal to the Kapandji sphincter there is the major duodenal papilla through which the pancreatic duct and common bile duct conduct pancreatic juice and bile. The third part, or horizontal part of the duodenum is 10~12 cm in length. It begins at the inferior duodenal flexure and passes transversely to the left. The third part contains Ochsner's sphincter17,18 with a length of 2 to 4.2 cm (3.2 ± 0.15 cm).6 The fourth part, or ascending part, of the duodenum passes upward up to duodenojejunal sphincter at the vertebral level L3 (Figure 4).
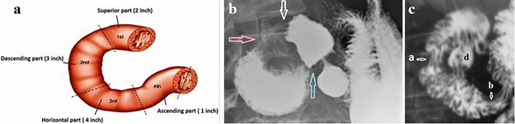
Figure 4 (a) Diagram of an empty duodenum. During anatomical examination and surgery, the first part of the duodenum (bulb) does not differ in shape from other sections. The bulb shape appears only during its functioning. ((b) Radiograph of elderly patient with duodenitis and duodenal dyskinesia. Postbulbar sphincter (white arrow). A sharp expansion of the duodenum is determined between the Kapanji sphincter (pink arrow) and the Ochsner sphincter (blue arrow). This expansion is due to the high pressure that occurs when both sphincters contract; (c) The duodenum was emptied, but the barium remained in deep folds because the barium-filled bowel was very wide. Two zones of contraction with longitudinal folds are visible: (a) the Kapanji sphincter, and (b) the Ochsner sphincter. The juxtapupillary diverticulum (d) is located between them. These diverticula result from the extrusion of the mucosa between the muscular fibers. Thus, this diverticulum is evidence of high pressure that occurs during contraction between Kapanji and Ochsner sphincters with duodenal dyskinesia.
Contraction of the postbulbar sphincter allows a certain portion of chyme to be concentrated in the bulb. Firstly, this fact does not raise doubts about the presence of a functional sphincter. Secondly, its function does not coincide with the law of the gut, which suggests the influence of specific Cajal cells as special pacemakers. After contraction of the bulb, a chemically aggressive chyme, equal to the volume of the bulb, penetrates the duodenum, where it stops due to the contraction of the Ochsner sphincter. Our studies confirmed Ochsner's assumption that this sphincter reacts by contracting acid, preventing the penetration of low-pH chyme into the jejunum.6 When the Ochsner sphincter contracts, the bolus is discarded cranially, but upon reaching the second part of the duodenum it causes contraction of the Kapandji sphincter. The repeated pendulum-like movement of the bolus between the Kapandji and Ochsner sphincters leads to the mixing of acidic chyme with bile and pancreatic secretions, which have an alkaline reaction. When the pH of the bolus increases to a certain level, the Ochsner sphincter opens and the bolus, having lost its aggressive nature, penetrates the jejunum.
Thus, the Ochsner sphincter contracts not above the bolus, as the law of the intestine states, but below it. This is probably the result of the action of specialized interstitial cells of Cajal (ICC).
The motor function of the small intestine (jejunum and ileum) has been little studied due to its inaccessibility to manometric studies and the overlap of several loops. The length of the small intestine is on average 4.5 m. It takes 3–5 hours from entry to the duodenum to exit from the ileum. Therefore, the bolus speed is about 1 meter/hour (360 sec) = 0.28 cm/sec, i.e., the speed of passage through the small intestine is 35 times slower than through the esophagus. This is more surprising because, upon leaving the duodenum, the contrast medium quickly fills the loops of the jejunum (Figure 5).
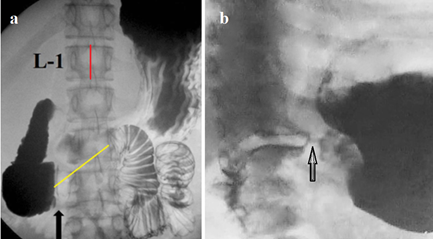
Figure 5 Evacuation of gastric contents into the small intestine. (a) Such cases are described as superior mesenteric artery (SMA) syndrome. The black arrow shows the beginning of compression of the duodenum. However, this compression cannot be caused by the SMA, since this vessel is in the midline of the vertebra. Secondly, with the diameter of the aorta ≈ 2 cm and the SMA ≈ 1 cm, the compression of the intestine cannot be more than 2 cm. Since the height of L-1 is 2.2 cm, the length of the narrowed section in the 3rd part of the duodenum (yellow line) is 4 cm, which corresponds to the location and length of Ochsner's sphincter. This radiograph is also presented here to show the rapid evacuation of gas and barium into the jejunum in a horizontal position. (b) In the infant's upright position, the gas entered the duodenum. The arrow indicates the pyloric sphincter.
In our search for an answer, we discovered that ICC of the deep myenteric plexus (ICC-DMP) is found exclusively in the small intestine. They are multipolar cells that are closely associated with nerve bundles of the DMP. Like ICC-IM, ICC-DMP also mediate enteric neurotransmission.20 The slower progression through the small intestine can be explained by the periodic retrograde movement of the bolus. The mechanism by which peristalsis is reversed—for example, in conditions of luminal toxicity—is not known. However, there is the fact that reverse peristalsis does occur in the small intestine.21
Our hypothesis suggests that slowing the movement of chyme through the small intestine allows for more complete processing and absorption of water and nutrients within the shorter length of the small intestine. An example of the functioning of the Ochsner and Kapandji sphincters in the duodenum, which is part of the small intestine, shows the mechanism of retrograde movement of chyme. Contraction of the bowel before the bolus causes the bolus to move retrograde. The pendulum-like movement between these sphincters can delay aboral movement for a long period. Probably ICC-DMP is a special type of ICC, which is an intestinal pacemaker, responsible for the retrograde movement of chyme in the small intestine.
The length of the large intestine is 1.5 m. Normal colon transit is nearly complete emptying at 72 h.22 Thus, the average speed of movement through the large intestine is 150 cm/259200 sec = 0.0006 cm/sec or 0.03 cm/min. The motor function of the colon obeys the law of the colon. The radiographs show how, as the bolus moves, its volume gradually decreases as a result of the absorption of fluid in the intestinal wall (Figure 6).
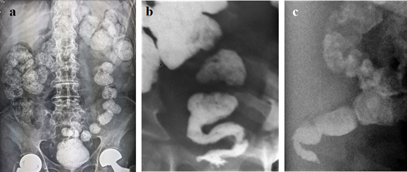
Figure 6 Patterns of motor function of the colon and rectum. (a) X-ray of the abdomen of a patient taking a drug containing a metal. The right half of the colon contains a stool containing water and gas. In the right side of the transverse colon, large individual intestinal segments appear that are denser due to the loss of water with a minute amount of gas. As these segments approach the rectum, their volume decreases sharply, and gas is not detected. (b-c) On the frontal and lateral projections of the anorectum, one can see how the intestinal segments with feces decrease in volume, turning into dense feces.
Some authors believe that segmental contractions and reverse peristalsis, mix promoting absorption occur in the colon,23 which contradicts scientific facts and is due to an erroneous interpretation of scintigraphy.24 The motor function of the large intestine is completely subject to the law of the intestine.
The “law of the intestine”, published 120 years ago, almost immediately became one of the foundation stones of physiology.1 As this study shows, this law is as relevant as it was 120 years ago. A convincing illustration of this is the passage of large tablets through the entire digestive tract (Figure 7).
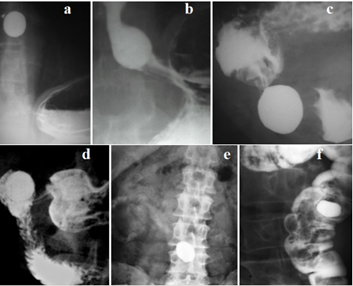
Figure 7 Radiographs of different patients who swallowed large tablets (LT) with a diameter of 2 to 3 cm. (a) LT in the middle of the esophagus; (b) above the contracted lower esophageal sphincter; (c) in the antrum of the stomach during antral systole; (d) in the duodenal bulb; (e) an x-ray was taken 28 hours after swallowing the LT. A reduced tablet is visible in the small intestine. Traces of barium from the disintegrated surface layer of the tablet are visible in the loops of the small intestine; (f) in the descending colon.
The peristaltic wave pushes the LT with a diameter ≈ 2 cm through all sphincters, which under normal conditions open to a diameter of 2-4 mm. This indicates that a strong peristaltic wave pushes the LT in a craniocaudal direction, and the caudal sphincter relaxes to allow the tablet to pass. This movement is consistent with the law of the intestine, which is valid throughout the gastrointestinal tract. The small bowel radiograph (Figure 7e) shows that the LT has traveled a long way in the small bowel, but the barium, which is far behind, moves much more slowly than the tablet. This supports the hypothesis that reverse peristalsis in the small bowel slows the movement of chyme to allow food to be fully digested and absorbed into the wall of small bowel.
The law of the intestine is more accurately called the law of peristalsis since it is also true for the urinary tract and biliary tract. For example, the tone of the ureterovesical junction decreased with increasing pressure in the ureter and increased with increasing pressure in the bladder.25 The discovery of interstitial cells of Cajal (ICC), which are called intestinal pacemakers, has opened a new era in understanding the motor function of different parts of the digestive tube. It turned out that different types of ICC have different specializations. This applies not only to different speeds of the peristaltic wave. In addition to typical peristalsis, ICCs coordinate two other types of contractions. Firstly, this concerns the storage chambers, i.e., proximal part of the stomach, gallbladder, and urinary bladder. The fundus of the stomach together with the body relaxes and contracts, because of a change in the tone of the entire section. They provide reception and temporary storage of food. The stomach can hold up to 1.5 liters of liquid without a significant change in its pressure. When the chyme begins to exit into the duodenum, the tone of the proximal section of the stomach increases to push the chyme into the antrum of the stomach. It is likely that the entire contents of these chambers are treated as a single bolus, and tonic contraction of the wall causes complete expulsion of the bolus. Peristalsis of the small intestine (duodenum, jejunum, and ileum) is modeled by a special type of pacemaker. ICC-LMP is found only in the small intestine and likely regulates retrograde and pendulum contractions. This mobility promotes better mixing of the chyme and increases the absorption time of food ingredients. This allows the shorter intestine to perform the function of the longer one.
All smooth muscle anatomical sphincter, including upper esophageal sphincter (UES), LES, pyloric sphincter, and internal anal sphincter (IAS), during surgery and anatomical examination do not differ from the adjacent intestine. Therefore, some practitioners have the impression that the LES is a thickened continuation of the esophagus, and the internal anal sphincter is a thickened continuation of the rectum. However, the function of these sphincters is very different from that of the intestinal segments. 1) They are in constant contraction; 2) They have clear boundaries and a certain length; 3) open at a certain threshold pressure above the sphincter; 4) do not participate in peristalsis; 5) shorten during opening. Around the UES, LES and IAS there are striated sphincters, which during short-term contractions enhance the function of smooth muscle sphincters. Due to rapid fatigue, their contraction progressively decreases over the course of a minute. For example, Shafik et al found that the crural diaphragm (CD) response disappeared when straining was sustained for more than 15-18 seconds (mean 16.8 ±1.2) and was not evoked after frequent successive straining because the CD consists of striated muscle which are easily fatigable and cannot remain contracted for a long period.26 This also applies to the external anal sphincter, which contracts when intra-abdominal pressure rises, but the force of its contraction quickly decreases until complete relaxation within one minute.27
The reliability of medical research depends on adherence to scientific methodology. Any research begins with an assumption, which is called a hypothesis. It should not contradict common sense, known scientific facts and recognized theories. If numerous studies confirm the correctness of a hypothesis, it becomes a theory. But if at least one reliable scientific fact contradicts the hypothesis, it should be rejected as false. Regarding gastroenterology, this means that numerous references to a hypothesis do not turn it into a theory. Secondly, the authors of the hypothesis must have a deep knowledge of the physiology of the digestive tract.
Before the proposal to perform pH monitoring in the distal part of the esophagus, it was believed that the presence of reflux of gastric contents into the esophagus was a pathological condition called gastroesophageal reflux (GER).
All conclusions based on a false hypothesis about the high diagnostic accuracy of pH monitoring are not scientific since they do not correspond to the truth:
Naive reasoning that air, swallowed with food or saliva must come out, for which in healthy individuals the LES periodically relaxes, does not stand up to criticism. Caballero et al found that gas, introduced simultaneously in large quantities in the stomach of the healthy subjects expelled per rectum, virtually no belching.36,37 This is a scientific fact. Figure 5 shows how gas flows from the stomach into the duodenum. Figure 6a shows a small amount of gas in the right part of the colon. Firstly, it does not correspond to the large volume that the patient could swallow over 6 hours. Secondly, after 12 hours of moving around the colon, gas has practically disappeared. These data suggest that swallowed air is utilized in the intestines. The consensus of Rome IV ignores the obvious fact that most young people do not know what a burp is. Rome IV participants differentiated normal from pathological based on pH monitoring. As a result of this, those GERD patients with belching, whose DeMeester score was less than 4 were mistakenly considered healthy. Thus, we can draw the following conclusions. a) All people swallow air along with food; b) All swallowed gas enters the intestines; с) Most of the swallowed air is probably utilized by the intestines; c) Repeated belching is a sign of weakness of the LES, i.e., GERD (Figure 8).
The angle of his an increase in the angle of His is considered a factor that contributes to the development of GERD. Figure 8 shows the pathogenesis of this phenomenon.
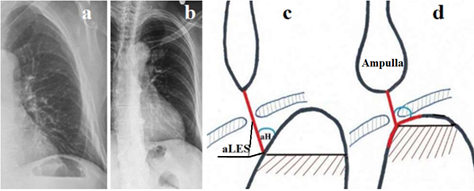
Figure 8(a-b) Radiographs of the left dome of the diaphragm of a healthy person (a) and a patient with GERD (b). (c). Scheme of the EGJ with normal LES function (red). The angle of His (aH) is acute. Large gas bubble in the stomach. (d). In GERD, the LES is shortened because the abdominal part of the LES (aLES) is not functioning. This leads to an increase in the angle of His and a decrease in the gas bubble of the stomach.
Based on manometric,38 radiological5 and histological studies,39 it has been established that the LES in GERD is shortened due to the opening of the abdominal part, which to varying degrees ceases to perform the antireflux function. As can be seen from Figure 8, shortening of the LES not only weakens its antireflux function, but also leads to an increase in the His angle. At the same time, reduces the gas bubble in the stomach. Weakness of the LES causes periodic relaxation of the LES, which is accompanied by belching. Histological studies of Chandrasoma have shown that in health the esophageal squamous epithelium transitions at the GEJ to gastric oxygentic epithelium with no intervening cardiac epithelium. The cardiac metaplasia of the squamous epithelium occurs due to exposure to gastric juice.39 This irrefutable evidence testifies that the cause of GERD is due to damage to the EGJ by hydrochloric acid. All other factors that supposedly influence the development of GERD,40 are the result of the disease, i.e., manifestations of pathogenesis. For at least 15 years, against the backdrop of pointless criticism from practical gastroenterologists, the Chandrasoma hypothesis remains valid. Moreover, it allowed us to abandon two widely common hypotheses. These are the belief that cardiac epithelium normally lines the proximal stomach, and that the GEJ is defined by the proximal limit of rugal folds.39 These two already rejected hypotheses, which were not based on scientific research, were the basis for the erroneous statement about the upward movement of the LES with shortening of the esophagus and the formation of a hiatal hernia.
Hiatal hernia: myth or reality?
А) It is believed that hiatal hernia (HH) refers to a condition in which the upper part of the stomach penetrates through the hiatus into the chest. It is also called a sliding hernia because it cannot be detected by X-ray examination in an upright position. It is assumed that in a horizontal position, conditions are created for the stomach to slide in the cranial direction due to the weakness and loss of elasticity of the phrenoesophageal ligament. It is diagnosed by barium swallow radiography, endoscopy, or manometry when greater than 2 cm in axial span.41 The theoretical basis justifying the sliding of the stomach into the chest includes several false hypotheses and experiments without adherence to scientific methodology.
a) As shown in the analysis of the article by Kwiatek et al.11 individuals who did not make complaints were selected for control. As an example, a patient with an X-ray picture of GERD was mistakenly chosen. The opening of the intra-abdominal part of the LES, which is typical of GERD, was mistakenly interpreted as shortening of the esophagus. Another piece of evidence was the assertion of cephalad displacement of the clip attached to the EGJ, i.e., to the proximal limit of rugal folds. However, the clip did not move relative to the thoracic vertebra. All the authors of this group, referring only to their own research, make the same mistakes. 1). With reflux esophagitis, the esophagus above the LES first expands. This part of the esophagus, called the phrenic ampulla, has weakened peristalsis. To create threshold pressure above the LES that would open the LES, a functional sphincter arises above the ampulla, which we called the proximal sphincter (PS). It should close the ampulla proximally, to maintain in it pressure higher the gastric pressure until the bolus enters the stomach and the LES closes the EGJ (Figure 9; see Figure 1d).
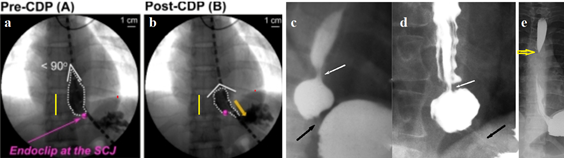
Figure 9 X-ray images of EGJ while drinking a contrast agent. (a-b). From the article by Kwiatek et al.11 The authors attached a clip to the end of the rugal folds, believing that this was a EGJ. At the moment the EGJ opened they decided that the clip had risen cranially.
As shown above, in the esophagus, and in the LES the rugal folds appear because of the inflammatory process, i.e., reflux esophagitis. The clip was attached to the top of the LES, not to the EGJ. The dilated supra diaphragmatic portion of the esophagus, limited by white spots, is the phrenic ampulla, which is the second evidence of GERD. On the radiograph (a) the distance from the clip to the stomach is about 1 cm (2 times shorter than the height D-10 - yellow line). This is the length of the LES, which is significantly shorter than normal, which is the third evidence of GERD. When the EGJ is opened (b), the clip is in the same place, near the lower left corner of D-10. In this case, the pressure in the ampulla is higher than the pressure in the stomach, which is due to contraction of the functional sphincter above the ampulla. The obtuse angle of His is caused by the opening of the abdominal part of the LES, which occurs because of shortening of the LES. This observation, firstly, proves that the selection of control persons based on the absence of complaints is erroneous. Secondly, the authors erroneously continue to consider rugal folds to be signs of the stomach, even though this hypothesis has not been scientifically substantiated and is not confirmed by histological39 and radiological studies.42 Thirdly, the statement about the shortening of the esophagus during swallowing turned out to be erroneous, both in this case and in numerous similar studies by this group of authors, starting with the works of Dodds.43 As shown above, in a horizontal position, transport of the bolus from the esophagus to the stomach occurs due to the last peristaltic wave. With reflux esophagitis, the last peristaltic wave expands and weakens, which manifests itself as an ampulla of the esophagus. To create high pressure to open the LES and deliver a bolus into the stomach, the ampoule must create pressure above gastric pressure. This occurs due to the functional sphincter above the ampulla, which we call the proximal sphincter (PS). Figure 9c-d shows the contraction zone of the esophagus above the ampulla, and figure (d) shows folds along the LES and esophagus, the different types of which depend on the intraluminal pressure.
b) In Figure 9e, in a patient with GERD, during the second barium sip, when the ampulla injected the bolus into the stomach, a sudden relaxation of the PS occurred. As a result, the pressure in the ampulla dropped and barium from the stomach entered the esophagus. This reflux proves the importance of the RS function and explains how transient LES relaxations occurs, which cannot be normal. Thus, incorrect selection of the norm and the use of pH monitoring, which detects only severe forms of GERD, have led to a false idea of the possibility of transient LES relaxations in healthy individuals. The arrow shows the contraction of the functional sphincter at the level of the aortic arch, the contraction of which prevents the reflux of chyme into the pharynx. We call it the aortic sphincter of the esophagus (AS).
From an analysis of the literature and my research, it follows that the esophagus does not shorten under any circumstances. In patients with GERD, the LES shortens due to the opening of the weakened intra-abdominal part of the LES. The distal peak pressure is caused by the contraction of the LES, which does not move cranially, and CD. The proximally peak is caused by contraction of the PS or the phrenic ampulla, which may be less or more than 2 cm. Thus, what is considered a “hiatal hernia” based on numerous false hypotheses is the esophageal ampulla. Esophageal ampulla is not a predisposing factor for GERD but is strong evidence of GERD. The current idea that a hiatal hernia (read “phrenic ampulla”) may be without GERD is based on an erroneous pH diagnosis of the GERD. A “hiatal hernia” (read "phrenic ampulla") is visible only in a horizontal position, not because the stomach slides into the chest, but because the ampulla functions only in a horizontal position.
High resolution manometry and gastroesophageal reflux
As seen in the study by Mittal et al.,44 the interpretation of HRM depends on the understanding of normal and pathological EGJ physiology (Figure 10).
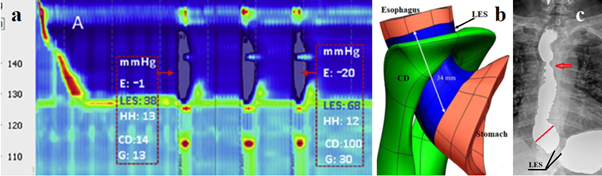
Figure 10 (a) High resolution manometry from the article by Mittal et al.44 The two high-pressure zones (brown spots) do not have specific characteristics based on which anatomical affiliation could be accurately established. The length and pressure value of the нижней zone, которая обозначена как CD, are larger than of the higher one. These designations for high-pressure zones correspond to the false idea of shortening the esophagus and displacement of the LES into the chest. This leads to the misconception that CD plays a more important role than LES, which contradicts all previous studies of the physiology of the EGJ. (b) Three-dimensional model of the EGJ.45 The length of the LES is 3.4 cm (blue). Its abdominal part is ≈2 cm. About 1 cm is located at the level of the CD and 0.4 cm above the diaphragm. (с) In a patient with GERD, high pressure in the stomach during rapid ingestion of barium led to a reflex contraction of the upper and lower esophageal sphincters. The length of the LES is significantly shorter than normal (1.7 cm versus 3.6 cm). The arrow shows functional narrowing at the level of the aortic arch. This is a functional sphincter that prevents reflux into the upper esophagus. We call it the aortic sphincter of esophagus (AS). It is also shown by the arrow in Figure 9 e.
Firstly, as shown above, the idea of shortening of the esophagus does not correspond to scientific research and therefore oral displacement of the LES is excluded. The cranial peak pressure, which is smaller in length and magnitude of pressure, cannot be caused by the pressure of the LES also because the length of the LES is 3.4-4.1 cm and it is in constant contraction, performing the main function of preventing reflux.46 The length of the CD in the hiatal canal is approximately 1 cm.44 Secondly, the CD consists of striated muscles, the contraction of which is sustained for more than 15-18 seconds (mean 16.8+/-1.2) and is not evoked after frequent successive straining.26 In addition, in patients with GERD the average cardia perimeter is 8.9 cm, in patients with Barrett’s esophagus – 13.8 cm, which is significantly more than in control subjects – 6.3 cm.47 Obviously, the wider the hiatal canal, the less influence CD has on the tone of the constantly contracted LES. Thirdly, the statement that CD can create pressure greater than the LES contradicts the statement of the same authors that it is the relaxation of the LES that causes GERD.
Analysis of scientific studies indicate that the CD is an external sphincter of the EGJ, which, together with the LES, relaxes to allow the bolus to pass into the stomach and short-term contracts to enhance the competence of the LES with inspiration, and during sudden increase in abdominal pressure.48 Thus, the high pressure (100 mmHg) at the level of the EGJ (Figure 10a) is due mainly to LES tone and partly to CD tone. The pressure (68 mmHg) in the lower part of the esophagus is caused by contraction of the PS, which has a length of 0.5-0.7 cm.42
This study provides a list of hypotheses that were previously considered theories, but since scientific evidence has proven these assumptions to be false, they should be excluded from subsequent use and citation.
None.

©2024 Levin. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.